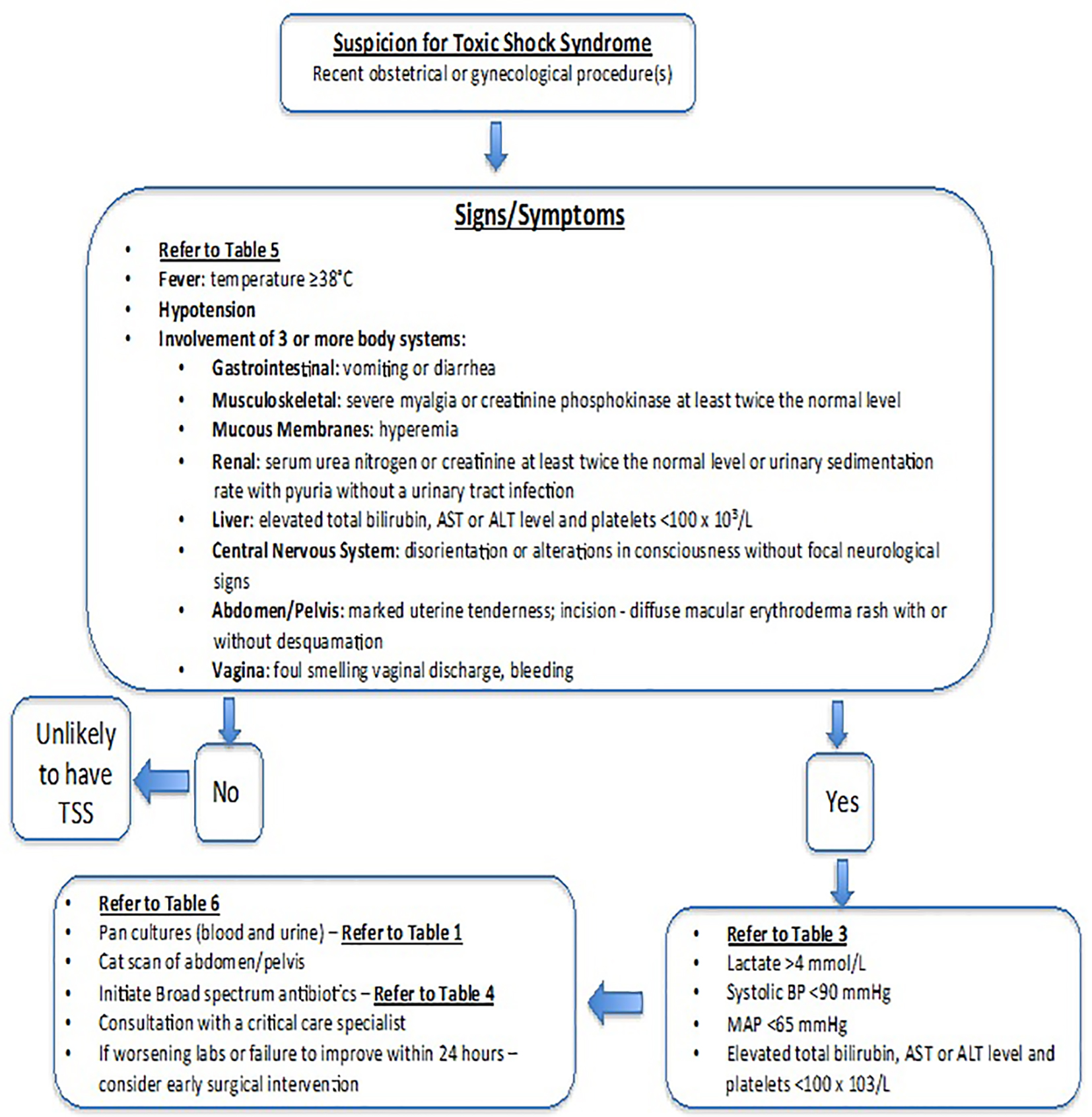
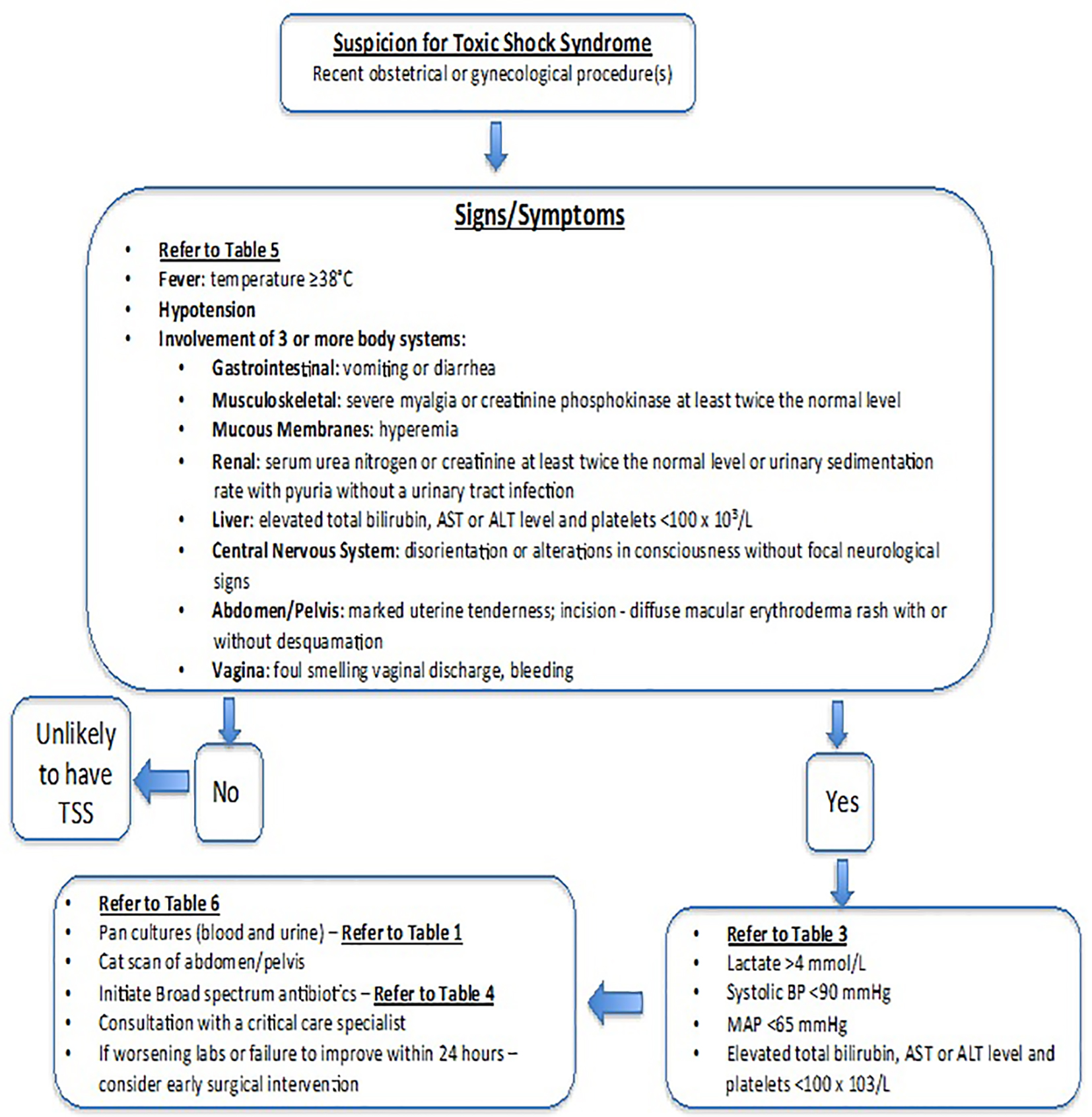
Figure 1. Algorithm for diagnosing and managing suspected toxic shock syndrome in obstetrics and gynecology.
| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Review
Volume 5, Number 1, March 2016, pages 1-16
Severe Infections in Obstetrics and Gynecology: How Early Surgical Intervention Saves Lives
Figure
Tables
| S. aureus: Staphylococcus aureus. |
| Gram-positive bacteria |
| Staphylococcus aureus (including methicillin-resistant S. aureus) |
| Streptococcus pyogenes (group A streptococcus) |
| Necrotizing soft tissue infections |
| Mixed aerobes and anaerobes |
| Staphylococcus aureus (including methicillin-resistant S. aureus) |
| Streptococcus pyogenes (group A streptococcus) |
| Clostridium perfringens |
| Clostridium sordellii |
| Clostridium septicum |
| Toxic shock syndrome |
| Staphylococcus aureus (including methicillin-resistant S. aureus) |
| Streptococcus pyogenes (group A streptococcus) |
| Clostridium perfringens |
| Clostridium sordellii |
| Clostridium septicum |
| Age | Procedure | Time from procedure to onset of symptoms | Time from symptom onset to death | As reported in |
|---|---|---|---|---|
| 32 | Cervical cone | 12 days | 6 h | Ho et al [20] |
| 40 | Cervical laser | 3 days | 2 days | Ho et al [20] |
| 16 | Oral and vaginal mifepristone | 5 days | 18 h | Reis et al [24] |
| 21 | Childbirth and vaginal laceration | 4 days | Aldape et al [11] | |
| 29 | Cesarean section | 2 days | Bitti et al [18] | |
| 24 | Childbirth and episiotomy | 4 days | Soper [22] | |
| 24 | Childbirth and episiotomy | 24 h | 5 days | Sosolik et al [13] |
| 40 | Childbirth | 4 days | 4 days | Rorbye et al [19] |
| 18 | Oral mifepristone, vaginal misoprostol | 4 days | 7 - 8 days | Fischer et al [14] |
| 21 | Oral mifepristone vaginal misoprostol | 5 days | < 24 h | Fischer et al [14] |
| 22 | Oral mifepristone, vaginal misoprostol | 5 days | 23 h | Fischer et al [14] |
| 34 | Oral mifepristone, vaginal misoprostol | 4 days | 12 h | Fischer et al [14] |
| 26 | Medical abortion | 7 days | < 3 days | Sinave et al [12] |
| 39 | Spontaneous endometritis | Not applicable | 18 h | Hogan et al [23] |
| Hysterectomy | Harvey et al [25] | |||
| 29 | Oral mifepristone, vaginal misoprostol | 4 days | 2 days | Meites et al [17] |
| 21 | Oral mifepristone, vaginal misoprostol | 6 days | 6 days | Meites et al [17] |
| Cesarean section | 2 months | 37 h | Cohen et al [16] | |
| 28 | Vaginal mifepristone | 11 h | 2 days | Cohen et al [16] |
| 24 | Oral mifepristone, vaginal misoprostol | 1 day | 7 days | Cohen et al [16] |
| 25 | Spontaneous abortion | Survived | Cohen et al [16] | |
| 18 | Oral mifepristone, vaginal misoprostol | 5 days | 3 days | Cohen et al [16] |
| 23 | Childbirth and episiotomy | 56 hours | 2 days | Golde [26] |
| 27 | Oral mifepristone, vaginal misoprostol | 3 days | 4 days | Wiebe et al [21] |
| 28 | Childbirth and episiotomy with retained vaginal sponge | 5 days | < 24 h | McGregor et al [15] |
| 23 | Cesarean section and cervical myoma degeneration | 6 days | Survived | McGregor et al [15] |
| 23 | Childbirth | 2 days | 3 days | McGregor et al [15] |
| mmol: millimole; dL: deciliter; mEq: milliequivalent; mg: milligram; mL: milliliter. |
| Complete blood count (CBC) |
| White blood cells (WBC) are generally > 25,000/mL or < 4,000/mL. |
| Marked bandemia (> 10%), independent of the total WBC |
| Hemolysis: hemoglobin level < 11 mg/dL |
| Massive hemoconcentration (hematocrit > 45%) secondary to fluid pouring into necrotic areas, resulting in third-spacing and edema and an intravascular depletion of fluid |
| Thrombocytopenia, as a result of disseminated intravascular coagulopathy |
| Complete metabolic profile (CMP) |
| Serum sodium of < 135 mEq/L |
| Creatinine level of > 1.6 mg/dL |
| Glucose level of >180 mg/dL |
| Anion gap metabolic acidosis |
| Bicarbonate < 15 mg/dL |
| Lactic acid > 2.2 mmol/L |
| Blood cultures |
| Infrequently positive, but if present would note: |
| Gram-positive cocci in chains indicate Streptococcus pyogenes |
| Gram-positive anaerobic rods indicate clostridial species |
| Gram-positive cocci in clusters indicate Staphylococcus aureus |
| Tissue diagnosis |
| Isolation of microbe or its associated virulence factors from infected tissue |
| Tissue should be sent to microbiology lab, or to a tertiary testing facility, such as the Center for Disease Control and Prevention (CDC), for molecular microbiologic analysis. |
| IV: intravenous; MRSA: methicillin-resistant Staphylococcus aureus. |
| Recommended first line regimen |
| Penicillin G 20 million units IV every 24 h |
| Or |
| Meropenem 1 - 2 g IV every 8 h |
| If MRSA - vancomycin 15 mg/kg IV every 12 h |
| Plus |
| Clindamycin 600 mg IV every 8 h |
| Alternative therapy (penicillin allergy - not anaphylaxis) |
| Cefazolin 1 - 2 g IV every 6 h |
| If MRSA - vancomycin 15 mg/kg IV every 12 h |
| Plus |
| Clindamycin 600 mg IV every 8 h |
| Alternative therapy (penicillin allergy - anaphylaxis) |
| Vancomycin 15 mg/kg IV every 12 h |
| Plus |
| Clindamycin 600 mg IV every 8 h |
| GAS: group A streptococcus. |
| Sepsis |
| Presentation: sudden onset of high fever, generally > 102 °F, shaking chills, flushing and surprising minimal amount of abdominal or uterine tenderness. |
| Blood cultures are frequently positive. |
| Postpartum endometritis |
| Presentation: influenza-like symptoms, chills, myalgia, nausea, vomiting, and diarrhea. |
| Fever usually exceeds 102 °F. |
| Pelvic organ tenderness or other physical findings may be minimal and not indicative of the severity of infection. |
| Wound infections |
| Presentation: rapid onset of acute cellulitis (subcutaneous tissue inflammation with marked local pain, tenderness, swelling, and erythema). |
| Quickly progresses to involve both the upper and superficial lymph nodes. |
| Generally occurs within hours of an abdominal incision for a laparotomy, cesarean delivery or in the perineum after an episiotomy or vaginal laceration. |
| Necrotizing soft tissue infections |
| Presentation: marked skin edema, bullae formation, local skin necrosis, and thrombosis of surrounding perforating vessels, ischemia and devitalized tissue, which is noted when tissue fails to bleed when cut into. |
| Severe local pain out of proportion to the observed abnormality with progression of erythema and edema are hallmark features. |
| The death rate from necrotizing fasciitis of patients who do not undergo surgical debridement approaches 100%. |
| Toxic shock syndrome |
| Presentation: initiates as an endometritis, cellulitis, or vulvar infection caused by GAS, non-focal abdominal pain that is out of proportion to physical findings, associated with a fever, leukocytosis, bandemia, and metabolic acidosis. |
| Progresses to fulminant multi-organ failure, shock and ultimately death within 48 - 96 h, if left untreated. |
| Release of superantigens by GAS results in a massive inflammatory storm. |
| TSS: toxic shock syndrome; WBC: white blood cell; mmol/L: millimole per liter. |
| Major indications |
| Failure to respond to antimicrobial therapy alone in the first 24 h |
| Rapid deterioration in clinical status with medical therapy intervention |
| Evidence of necrotizing soft tissue infection |
| Evidence of intraabdominal or pelvic fluid collection concerning for abscess collection |
| Evidence of gas within the uterine myometrial tissue, concerning for necrotizing soft tissue infection with clostridial species |
| Source expected to be the uterus |
| Postpartum (cesarean or vaginal delivery) |
| Postabortal or septic abortion |
| Worsening laboratory signs of TSS and/or tissue necrosis, despite medical therapy |
| Refer to Table 3. |
| Systemic signs of sepsis |
| Septic shock |
| Adult respiratory distress syndrome |
| Disseminated intravascular coagulation |
| Hemolysis |