| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Review
Volume 2, Number 2, September 2013, pages 47-50
Breast Disorders During Pregnancy and Lactation: The Differential Diagnoses
Hayden Bella, e, Gudrun Petersb, c, Anne Lynchd, Robin Harlea
aRoyal Hobart Hospital, GPO Box 1061, Hobart, Tasmania 7001, Australia
bRegional Imaging Tasmania, 49 Augusta Road, Lenah Valley, 7008 Tasmania, Australia
cBreastScreen Tasmania, Level 4, 25 Argyle Street, Hobart 7001 Tasmania, Australia
dMonash BreastScreen, Centre Road, P O Box 72, East Bentleigh VIC 3165, Australia
eCorresponding author: Hayden Bell, Royal Hobart Hospital, GPO Box 1061, Hobart, Tasmania 7001, Australia
Manuscript accepted for publication May 3, 2013
Short title: Breast Disorders During Pregnancy and Lactation
doi: https://doi.org/10.4021/jcgo140w
- Abstract
- Introduction
- Galactocele
- Fibroadenoma
- Lactating Adenoma
- Puerperal Mastitis/Abscess Disease
- Pregnancy-Associated Breast Cancer
- Conclusion
- References
| Abstract | ▴Top |
This article reviews breast disorders which can present as palpable masses during pregnancy or lactation. It focuses on the most common differential diagnoses: galactocele, fibroadenoma, lactating adenoma, mastitis and abscess, and pregnancy-associated breast cancer.
Keywords: Breast mass; Breast; Lactation; Pregnancy; Galactocele; Fibroadenoma; Lactating adenoma; Mastitis; Abscess; Pregnancy associated breast cancer
| Introduction | ▴Top |
In preparation for lactation, pregnancy is a time of unique change to breast tissue. Due to higher circulating levels of hormones, there is more ductal and lobular growth, increased vascularity and a reduction in stroma [1, 2]. This usually results in significantly increased breast density, which can cause difficulty in the clinical and radiological diagnosis of pregnancy and lactation-associated breast masses [2, 3].
A pregnancy-related breast disorder is defined as a diagnosis made during pregnancy, within one year post-partum or during lactation [4]. Most disorders are similar to those in non-pregnant women, however there are a number of conditions unique to pregnancy and lactating women. These conditions almost always present as a palpable mass [4] and are often a source of great anxiety for the woman and her family. The main differential diagnoses for palpable breast masses in pregnant or lactating women include: fibroadenoma, lactational adenoma, mastitis with or without abscess formation, galactocele and normal breast tissue with lactational change.
| Galactocele | ▴Top |
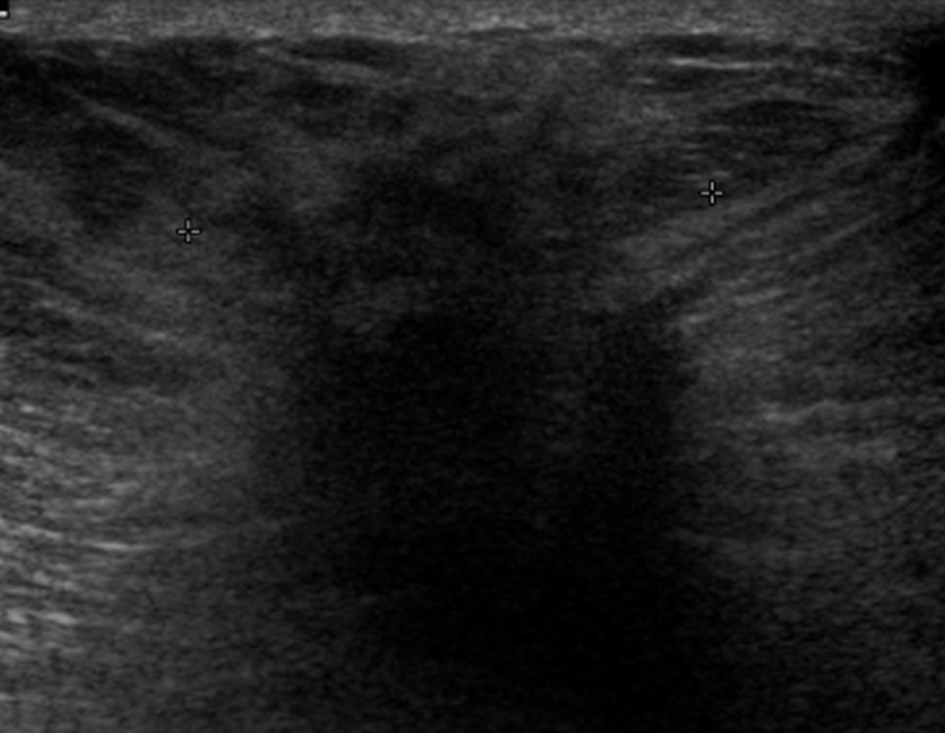
A galactocele (Fig. 1) is the most common benign mass lesion diagnosed during lactation. It often develops following cessation of breastfeeding, when milk is stagnant [1]. This can lead to duct dilatation and obstruction/rupture, with extravasation of milk into the surrounding stroma. Galactoceles can be associated with inflammation and necrosis [1]. Clinically a galactocele appears as a well circumscribed smooth mass that is often mobile [5].
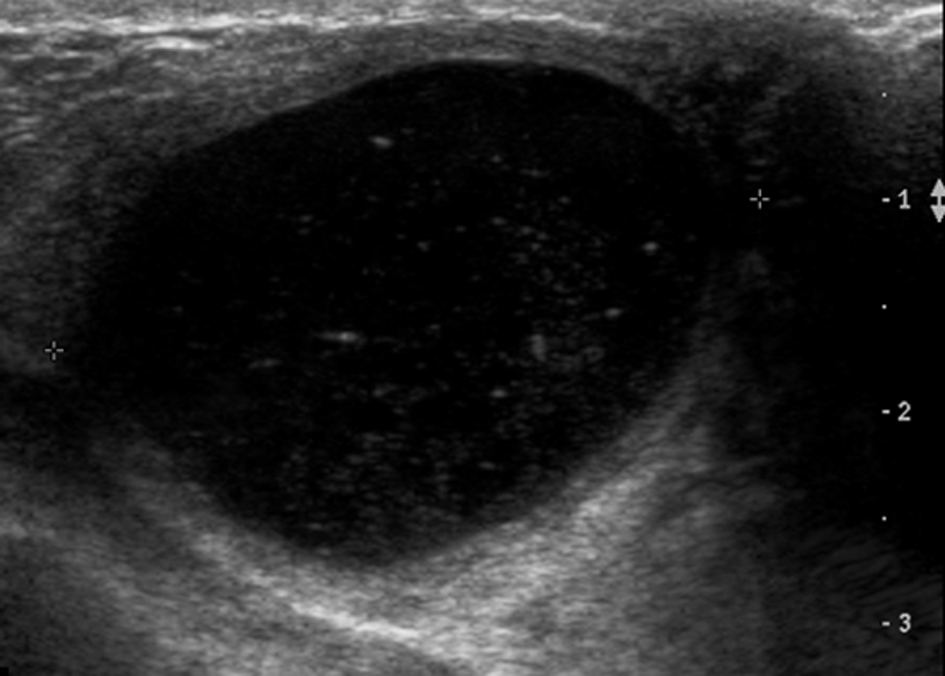 Click for large image | Figure 1. Complex cystic mass on ultrasound. Fine needle aspiration confirmed a galactocele. |
Ultrasound findings are those of a simple or complicated cyst, with a well circumscribed, ovoid, anechoic or hypoechoic mass showing posterior acoustic enhancement [6]. The appearance on ultrasound and mammography can be variable depending on the fat and protein content present [1]. Aspiration of a galactocele is both diagnostic and therapeutic.
| Fibroadenoma | ▴Top |
A fibroadenoma (Fig. 2) is the most common benign solid breast lesion, and results from proliferation of intralobular stroma [7]. Fibroadenomas are hormone sensitive and are therefore expected to grow during pregnancy and breastfeeding due to increased hormone levels, resulting in detection of a previously unnoticed lump [1].
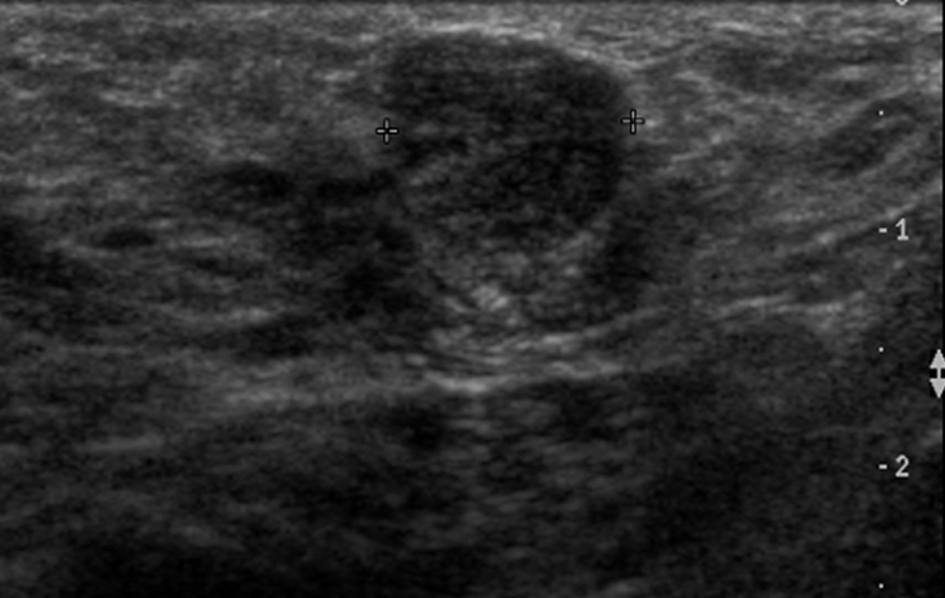 Click for large image | Figure 2. Hypoechoic mass with well circumscribed margins. Confirmed as a fibroadenoma on histopathology. |
The ultrasound appearance is often no different to a fibroadenoma in a non-pregnant or non-lactating woman (hypoechoic, well defined mass), but they may be less conspicuous due to proliferation of surrounding isoechoic glandular tissue. Occasionally, due to rapid growth, a fibroadenoma may have complex features such as cystic spaces and increased vascularity. These lesions may also undergo spontaneous infarction. This can result in imaging findings that are more suspicious such as heterogeneous echotexture and shadowing on ultrasound [8].
A tissue diagnosis is required for presumed fibroadenomata that are solitary and palpable, or that display atypical features on clinical examination or imaging [9].
| Lactating Adenoma | ▴Top |
A lactating adenoma (Fig. 3) is a benign stromal tumour which often presents as a palpable mobile mass with rapid growth during pregnancy. Ultrasound is the imaging modality of choice. The appearance of a lactating adenoma can be almost identical to a fibroadenoma [1]. On ultrasound it often appears as a hypoechoic lesion with well circumscribed or gently lobulated margins, parallel to the skin (wider-than-tall). However, imaging features suggestive of malignancy may be present [1, 10]. In this situation, a tissue sample must also be sought to make a definitive diagnosis.
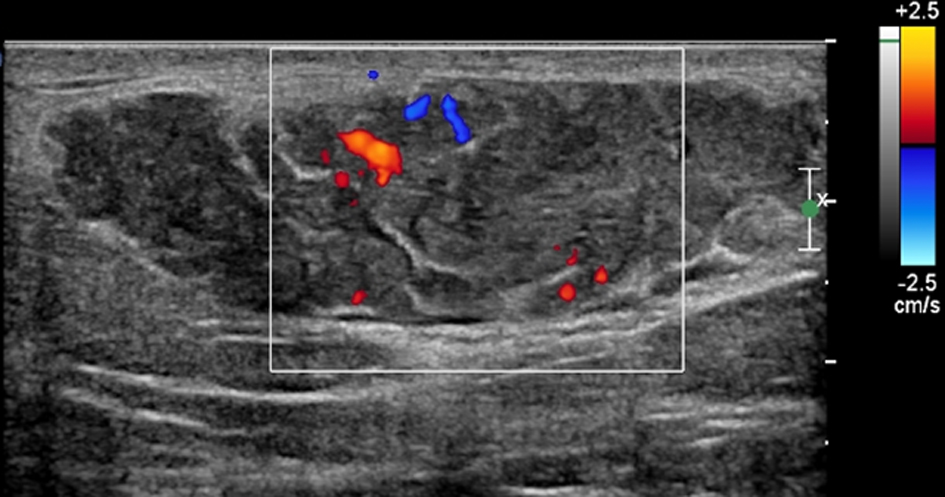 Click for large image | Figure 3. Lobulated hypoechoic lesion demonstrating hypervascularity on colour Doppler flow. Histopathology confirmed a lactating adenoma. |
| Puerperal Mastitis/Abscess Disease | ▴Top |
Puerperal mastitis is inflammation (Fig. 4a, b) of the breast that occurs during pregnancy, lactation or weaning. It is rare during pregnancy but is relatively common during lactation [1]. A breast abscess is a localised collection of pus within the breast. It often forms as a complication of mastitis however it is estimated that only approximately 5-11% of lactating women with infectious mastitis will develop breast abscesses [4].
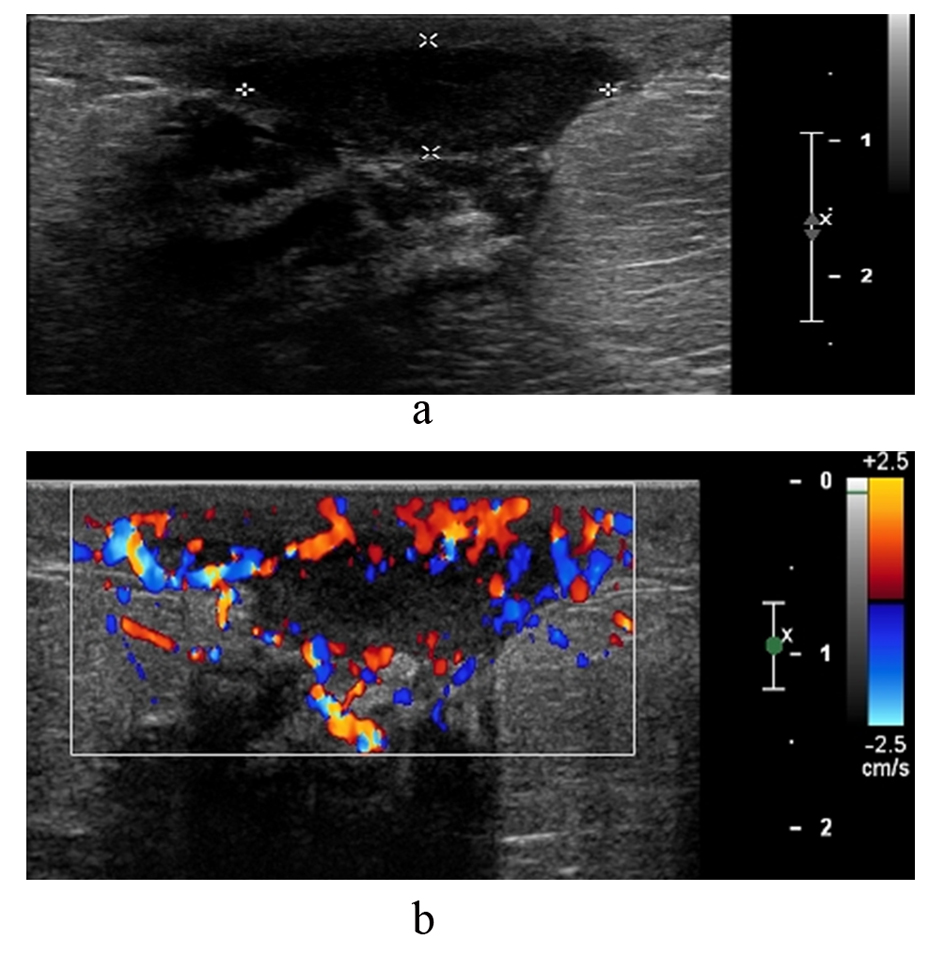 Click for large image | Figure 4. (a and b). This patient was 3 months post-partum and presented with inflammation of the breast. Ultrasound shows a fluid collection in the retroareolar region with hypervascularity of the surrounding tissue. Imaging findings confirmed a retroareolar abscess with mastitis of the adjacent tissue. |
The clinical presentation of a breast abscess is similar to that of mastitis. It tends to present with fever and malaise, focal painful inflammation of the breast, and with a tender palpable fluctuant mass [11].
The primary organisms responsible for infection are staphylococcus aureus, followed by streptococcus. These organisms originate from the feeding infant’s nose/throat and enter via epithelial disruption of the nipple or surrounding areola. The presence of stagnant milk is important as it provides a culture medium for these bacteria [1].
Ultrasound is used to investigate whether abscess formation has occurred, and for image-guided abscess drainage. Malignancy must be ruled out with tissue sampling if a patient’s condition does not improve with antibiotic therapy [1].
| Pregnancy-Associated Breast Cancer | ▴Top |
Pregnancy-associated breast cancer (PABC) refers to breast cancer diagnosed during pregnancy, one year post-partum or anytime during lactation. It occurs in approximately 0.3/1,000 pregnancies [12]. Most women diagnosed with PABC present with a palpable lump [13]. It has been noted that when age and stage of presentation are matched with non-pregnant women, there is no difference in prognosis for early disease. Pregnant women with more advanced disease have a poorer prognosis when compared with non-pregnancy associated breast cancer [13].
A delay in diagnosis can be attributed to hypertrophy of breast tissue during pregnancy and lactation, which can mask symptoms [3, 5]. Mammography in pregnant and lactating women often shows dense breast tissue. For this reason, ultrasound is the most appropriate first line imaging method for assessment and carries no risk of foetal irradiation [11].
Even though mammography in pregnant or lactating women is not recommended as a first line investigation, it has a reported sensitivity during pregnancy and lactation of 78-90% [13], and has been proven safe for the foetus with proper abdominal shielding [1, 3, 13]. Radiological features of pregnancy-associated breast cancers (Fig. 5) on ultrasound are similar to those of non-pregnancy-related breast cancer [4] and include hypoechogenicity, acoustic shadowing, angular margins, interruption of the normal planes of breast tissue and ‘taller than wide’ shape. Obtaining a tissue sample is a vital component of diagnosis and is required for lumps which persist during pregnancy and lactation [5].
 Click for large image | Figure 5. Mass lesion with indistinct margins. The lesion was a grade 2 invasive lobular cancer on histopathology. |
| Conclusion | ▴Top |
A palpable breast mass is always cause for concern and results in great anxiety for the pregnant or lactating patient. Knowledge of the potential differential diagnoses, and of appropriate avenues for investigation and management are therefore essential skills for medical practitioners dealing with a breast mass in this group of women.
| References | ▴Top |
- Sabate JM, Clotet M, Torrubia S, Gomez A, Guerrero R, de lasHeras P, Lerma E. Radiologic evaluation of breast disorders related to pregnancy and lactation. Radiographics. 2007;27(Suppl 1):S101-124.
doi pubmed - Robbins J, Jeffries D, Roubidoux M, Helvie M. Accuracy of diagnostic mammography and breast ultrasound during pregnancy and lactation. AJR Am J Roentgenol. 2011;196(3):716-722.
doi pubmed - Taylor D, Lazberger J, Ives A, Wylie E, Saunders C. Reducing delay in the diagnosis of pregnancy-associated breast cancer: how imaging can help us. J Med Imaging RadiatOncol. 2011;55(1):33-42.
doi pubmed - Son EJ, Oh KK, Kim EK. Pregnancy-associated breast disease: radiologic features and diagnostic dilemmas. Yonsei Med J. 2006;47(1):34-42.
doi pubmed - Whang IY, Lee J, Kim KT. Galactocele as a changing axillary lump in a pregnant woman. Arch Gynecol Obstet. 2007;276(4):379-382.
doi pubmed - Hicks DH, Lester SC. Diagnostic Pathology: Breast. Volume 9. Salt Lake City: Amirsys, 2012.
pubmed - Oh YJ, Choi SH, Chung SY, Yang I, Woo JY, Lee MJ. Spontaneously infarcted fibroadenoma mimicking breast cancer. J Ultrasound Med. 2009;28(10):1421-1423.
pubmed - Brennan M, Houssami N, French J. Management of benign breast conditions. Part 2—breast lumps and lesions. AustFam Physician. 2005;34(4):253-255.
pubmed - Baker TP, Lenert JT, Parker J, Kemp B, Kushwaha A, Evans G, Hunt KK. Lactating adenoma: a diagnosis of exclusion. Breast J. 2001;7(5):354-357.
doi pubmed - Dixon JM. Breast Abscess. In: UpTo Date, Basow DS, UpTo Date, Waltham, MA, 2012.
- Ayyappan AP, Kulkarni S, Crystal P. Pregnancy-associated breast cancer: spectrum of imaging appearances. Br J Radiol. 2010;83(990):529-534.
doi pubmed - Litton JK, Theriault RL, Gonzalez-Angulo AM. Breast cancer diagnosis during pregnancy. Womens Health (LondEngl). 2009;5(3):243-249.
doi pubmed - Barnes DM, Newman LA. Pregnancy-associated breast cancer: a literature review. SurgClin North Am. 2007;87(2):417-430, x.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.