| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 1, Number 1, February 2012, pages 19-23
Cutaneous Metastasis of Endometrial Carcinoma: A Case Report and Literature Review
Fatima Zahra El M’rabeta, b, d, Andreas Hottingera, George Anne Claudea, Jean Christophe Tillec, Omar El Mesbahib, Monica Castiglione-Gertscha, Alexandre Bodmera
aDepartment of Medical Oncology, Geneva University Hospital. Geneva, Switzerland
bDepartment of Medical Oncology, University Hospital Hassan II. Fez, Morocco
cDepartment of Clinical pathology, Geneva University Hospital. Geneva, Switzerland
dCorresponding author: Fatima Zahra. El M’rabet, Unit of Medical Onco Gynecology, Bd. de la Cluse 30,1211, Geneva, Switzerland
Manuscript accepted for publication November 2, 2011
Short title: Cutaneous Metastasis of Endometrial Carcinoma
doi: https://doi.org/10.4021/jcgo6e
| Abstract | ▴Top |
Cutaneous metastases from endometrial adenocarcinoma are rare with poor prognosis. Despite large autopsy studies quoting a frequency of cutaneous metastases from endometrial adenocarcinoma of under 1 %. The most common presentation of cutaneous metastases is rapidly developing nodules or tumors. The diagnosis of cutaneous metastatic carcinoma hinges on histopathologic evaluation of the involved skin lesion. We report a case of cutaneous metastasis of endometrial adenocarcinoma with fatal evolution.
Keywords: Endometrial carcinoma; Skin; Metastases; Prognosis
| Introduction | ▴Top |
In clinical practice, cutaneous metastases from cancer are uncommon, but when present may herald the diagnosis of internal malignancy. Rasbach et al. [1] and Damewood et al. [2] reviewed postmortem examinations of 2279 autopsy studies of patients who died from internal neoplasm; only 58 cases of skin metastasis (2.5%) were identified. The majority of these lesions were located on the trunk and extremities. Breast (69%), colon (9%), melanoma (5%), and ovary cancer (4%) were identified as the primary tumors that typically metastasize to the skin. Despite the high incidence of uterine adenocarcinoma, cutaneous metastases are uncommon and only few cases have been reported in the literature. Only 1 case of skin metastasis was observed in 86 cases of endometrial cancer (1.1%) [3]. We report a case of endometrial adenocarcinoma with initial limited disease, presumed to have been completely resected after staging and grading, which recurred as a cutaneous metastasis associated with lung metastasis.
| Case Report | ▴Top |
A 72-year-old woman, postmenopausal for 24 years, was followed regularly for hypertension and a history of retinal melanoma treated 3 years ago by accelerated proton beam. She was diagnosed with FIGO Stage IC, Grade 1 adenocarcinoma of the endometrium-endometrioid type and underwent a total abdominal hysterectomy, bilateral salpingo-oophorectomy, and pelvic and paraaortic lymph node sampling. She did not need adjuvant therapy and was deemed disease free after her intervention. Six months after her initial therapy she presented in the emergency room with stade IV dyspnea and the appearance of multiple subcutaneous nodules located on her trunk, extremities and scalp.
The clinical examination was remarkable for a patient with reduced performance status (WHO 3), a right effusion syndrome and the presence of multiple painful subcutaneous nodules, of hard consistency, affecting mainly the trunk, with one lesion on the scalp. The patient underwent an extensive metastatic evaluation both to determine the extent of disease and to rule out the possibility of a second primary adenocarcinoma. A thoracic, abdominal and pelvic computed tomography (CT) not only confirmed the presence of multiple subcutaneous nodules, but also showed intramuscular thoracic and abdominal lesions, as well as numerous retroperitoneal, and mediastinal lymph nodes and a right pleural effusion (Fig.1A and B). CT of the brain showed a single lesion in the right frontal region of the scalp. The pleural fluid cytology showed the presence of neoplasic cells compatible with adenocarcinoma. An incisional biopsy of a subcutaneous nodule was performed and the histological exam confirmed a cutaneous metastasis of a moderately differentiated adenocarcinoma, Immunohistochemically, the tumor cells were positive for cytokeratine 7 while negative for cytokeratine 20, Melan-A and S-100 protein, compatible with the known adenocarcinoma of the endometrium (Fig. 2 and 3). Because of the poor general condition and the rapid deterioration of the patient, no treatment was started. The evolution was rapidly fatal; the patient died two week after her admission due to respiratory failure.
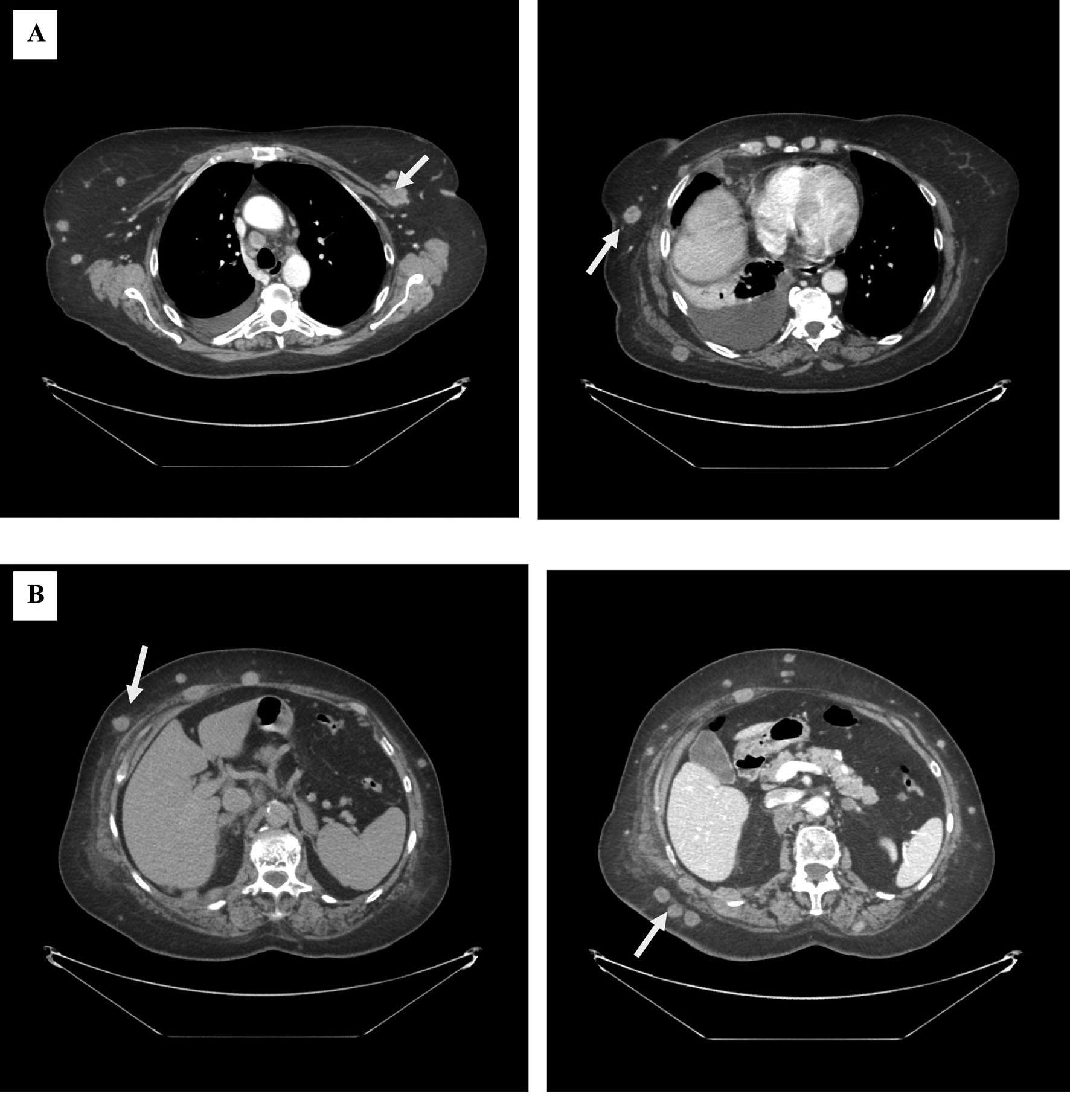 Click for large image | Figure 1. CT scan showing multiple subcutaneous nodules in the thoracic (A) and abdominal (B) of various sizes, referring first of metastatic lesions. |
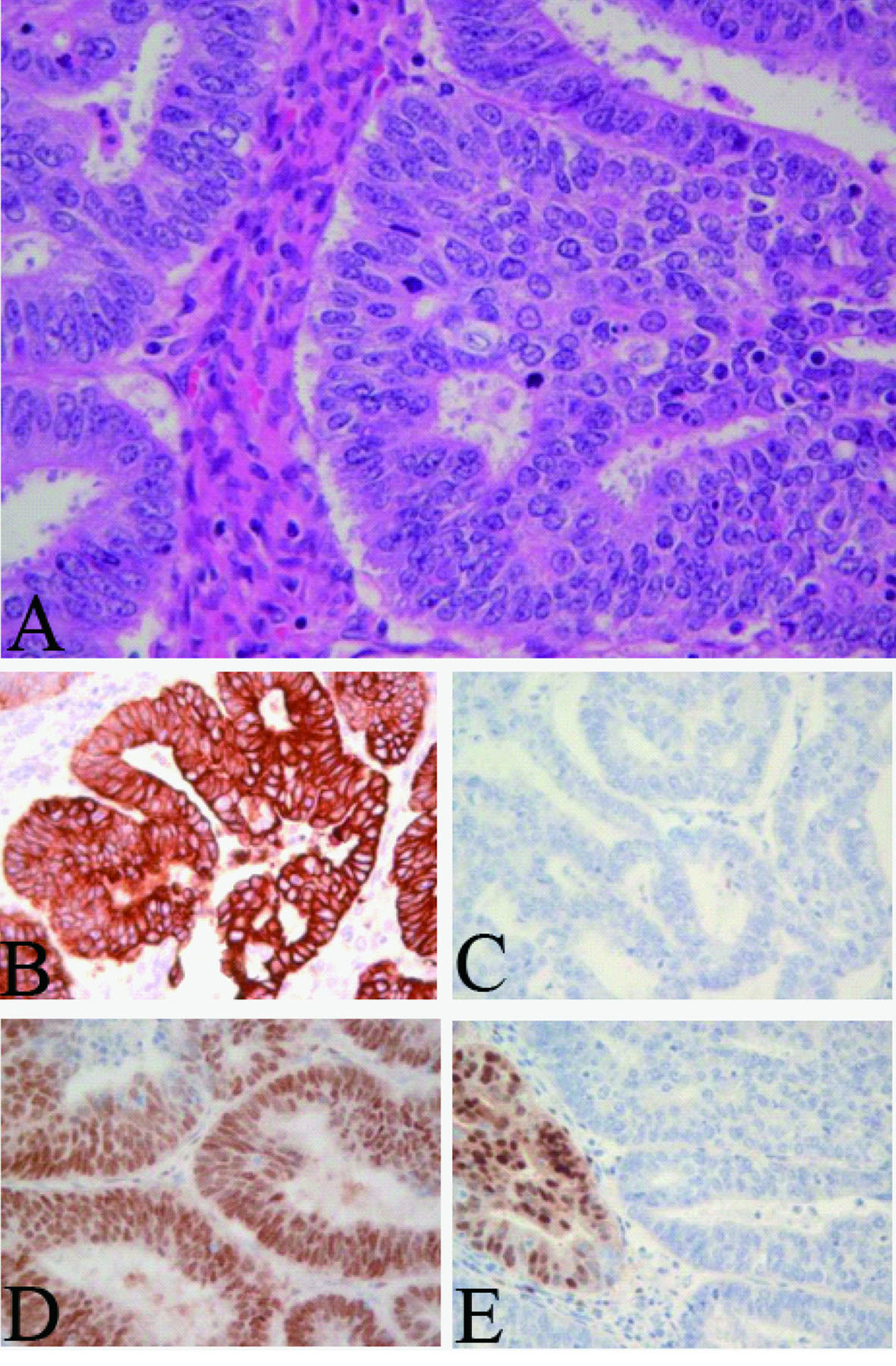 Click for large image | Figure 2. Endometrial carcinoma. A: Hemalun-eosin staining, magnification 400 ×. B: Cytokeratin 7 positivity; C: Loss expression of PTEN; D: Estrogen receptor expression; E: Focal expression of progesterone receptor. Same immunohistochemical expression in both lesions compatible with a skin metastasis of the endometrioid carcinoma. |
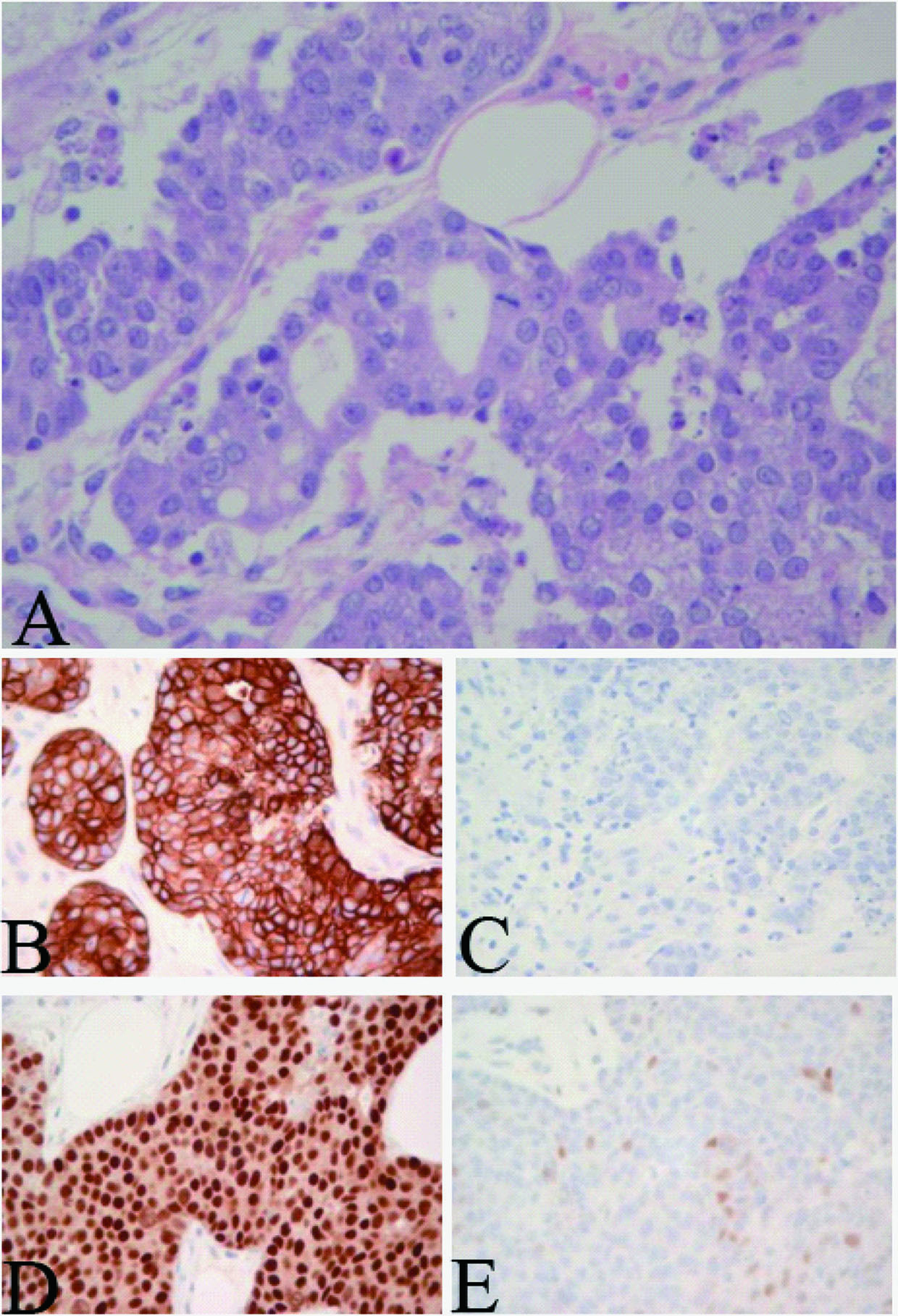 Click for large image | Figure 3. Skin metastasis. A: Hemalun-eosin staining, magnification 400 ×; B: Cytokeratin 7 positivity; C: Loss expression of PTEN; D: Estrogen receptor expression; E: Focal expression of progesterone receptor. Same immunohistochemical expression in both lesions compatible with a skin metastasis of the endometrioid carcinoma. |
| Discussion | ▴Top |
Metastases to the skin from internal carcinoma are relatively rare, with a reported incidence of 0.7 - 9% [3]. Cutaneous metastases may be the first presentation of such malignancies, accompany other symptoms, or occur during follow-up [4]. Breast cancer is the most common origin of cutaneous metastases in women and lung cancer is the most common origin in men [4]. Skin metastases from endometrial adenocarcinoma are extremely rare [5]. Fortunately, most cases are diagnosed at an early stage when surgery alone may be adequate for cure. Women with recurrent or metastatic endometrial cancer represent a heterogeneous group. The disease usually spreads by local or lymphatic dissemination. Distant metastases are less common and usually involve the lung, liver, and bone [4]. Despite the high incidence of endometrial adenocarcinoma, there is a paucity of reports of skin metastases in this disease, and most of these reports emphasize the rarity of this pattern of dissemination. In the reported cases, metastasis from endometrial cancer has been most commonly noted at the site of initial surgery and radiotherapy. Therefore, the initial surgical and radiotherapy site must be examined carefully for skin metastasis. More rarely, distant cutaneous sites, including scalp, toes and trunk have been reported [6, 7]. Cutaneous metastases may vary in number, from a single nodule, to greater than 20 lesions, such as in our patient. In this report, cutaneous metastases were primarily localized in the trunk, with a single scalp nodule discovered incidentally on CT. Skin metastases from endometrial carcinoma are usually confined to the subcutaneous tissue and present as discrete movable painless masses. They are often highly vascular [8, 9]. These lesions may appear in several forms such as inflammatory lesions, discrete nodules, or plaques. Carcinoma reaches the skin by a variety of mechanisms including direct extension, lymphangitic or hematogenous spread, and through implantation in surgical scars. Diffuse distribution of subcutaneous nodules suggests hematogenous rather than lymphatic spread, as reported by others [10]. When skin metastases are identified, they usually represent widespread dissemination of the underlying malignancy [10]. However, in this case, endometrial carcinoma was diagnosed at an early stage when surgery alone was adequate for cure. Cutaneous metastases were discovered at the same time as lung metastasis, suggesting widespread hematogenous dissemination.
Depending upon prior therapy and the nature of the recurrence, these patients may be treated with palliative or curative intent. To date, no effective treatment has been demonstrated due to the rarity of this specific site of metastasis. However, treatment strategies have been based on experience with other presentations of recurrent endometrial cancer. Current recommendations include local excision if feasible, with a single skin metastasis [11]. The treatment for most patients is palliative, and, although chemotherapy and radiotherapy are often used in these patients, they are ineffective in many cases (Table 1) [12].
 Click to view | Table 1. Skin Metastasis of Endometrial Carcinoma: Review of Reports in the Literature [12]. |
Cutaneous metastases of disseminated adenocarcinoma reflect an almost universally poor prognosis, with mean life expectancy being reported as approximately 3 months [10], although rare examples may survive considerably longer. An awareness of this rare manifestation of a relatively common malignancy is important, in that its identification significantly affects prognosis. In our case, no treatment could be started due to the rapid progression of the disease. The evolution was rapidly fatal and the patient died a two week after her admission due to respiratory failure.
Conclusion
Although endometrial cancer is one of the most frequent malignancies in women, skin metastasis from endometrial cancer is very rare. The appearance of subcutaneous nodules is evidence of widespread dissemination and a harbinger of early demise, demonstrating the poor prognosis for these patients.
Competing Interests
The authors declare that they have no competing interests.
| References | ▴Top |
- Rasbach D, Hendricks A, Stoltzner G. Endometrial adenocarcinoma metastatic to the scalp. Arch Dermatol. 1978;114(11):1708-1709.
pubmed doi - Damewood MD, Rosenshein NB, Grumbine FC, Parmley TH. Cutaneous metastasis of endometrial carcinoma. Cancer. 1980;46(6):1471-1475.
pubmed doi - Krathen RA, Orengo IF, Rosen T. Cutaneous metastasis: a meta-analysis of data. South Med J. 2003;96(2):164-167.
pubmed doi - Lookingbill DP, Spangler N, Sexton FM. Skin involvement as the presenting sign of internal carcinoma. A retrospective study of 7316 cancer patients. J Am Acad Dermatol. 1990;22(1):19-26.
pubmed doi - Reingold IM. Cutaneous metastases from internal carcinoma. Cancer. 1966;19(2):162-168.
pubmed doi - Mandrekas DP, Dimopoulos AM, Moulopoulou D, Papamichalis G, Gougoulakis AG. Distant cutaneous metastasis from carcinoma of the uterus. A case report. Eur J Gynaecol Oncol. 1999;20(3):212-213.
pubmed - Giardina VN, Morton BF, Potter GK, Mesa-Tejada R, Waterfield WC. Metastatic endometrial adenocarcinoma to the skin of a toe. Am J Dermatopathol. 1996;18(1):94-98.
pubmed doi - Brownstein MH, Helwig EB. Patterns of cutaneous metastasis. Arch Dermatol. 1972;105(6):862-868.
pubmed doi - Taboada CF, Fred HL. Cutaneous metastases. Arch Intern Med. 1966;117(4):516-519.
pubmed doi - Elit L, Lukka H, Friedman E. Cutaneous metastasis of papillary serous uterine cancer. Gynecol Oncol. 2001;82(1):208-211.
pubmed doi - Awtrey CS, Cadungog MG, Leitao MM, Alektiar KM, Aghajanian C, Hummer AJ, Barakat RR, et al. Surgical resection of recurrent endometrial carcinoma. Gynecol Oncol. 2006;102(3):480-488.
pubmed doi - Mustafa MS, Al-Nuaim L, Inayat-Ur-Rahman N. Scalp and cranial bone metastasis of endometrial carcinoma: a case report and literature review. Gynecol Oncol. 2001;81(1):105-109.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
