| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 2, Number 2, September 2013, pages 81-83
A Case of Monochorionic-Diamniotic Twin Pregnancy Complicated by Massive Subchorionic Hemorrhage
Yukiko Fusea, Yoshie Hiraizumia, Hidehiko Miyakea, Shunji Suzukia, b
aDepartment of Obstetrics and Gynecology, Japanese Red Cross Katsushika Maternity Hospital, Tokyo, Japan
bCorresponding author: Shunji Suzuki, Department of Obstetrics and Gynecology, Japanese Red Cross Katsushika Maternity Hospital, 5-11-12 Tateishi, Katsushika-ku, Tokyo 124-0012, Japan
Manuscript accepted for publication May 3, 2013
Short title: Monochorionic-Diamniotic Twin Pregnancy Complicated
doi: https://doi.org/10.4021/jcgo135w
| Abstract | ▴Top |
We encountered a case of monochorionic-diamniotic twin pregnancy complicated by massive subchorionic hemorrhage (MSH) observed after 28 weeks of gestation. In this case, the presence of MSH seemed to affect the circulation of fetus in the hemorrhagic side (Twin A) as well as the circulation of another fetus (Twin B) after 28 weeks of gestation. In Twin A, the presence of MSH caused chronic anemia and oligohydramnios, eventually it led to non-reassuring fetal status. In addition, MSH led to oligohydramnios in Twin B.
Keywords: Monochorionic-diamniotic twin pregnancy; Massive subchorionic hemorrhage; Oligohydramnios
| Introduction | ▴Top |
Massive subchorionic hemorrhage (MSH), which was first described by Breus in 1892 (Breus’ mole) [1], is a serious condition in pregnancy that is frequently complicated by perinatal abnormalities such as feta growth restriction, oligohydramnios, preterm labor and fetal demise due to uteroplacental circulatory insufficiency from MSH mainly formed by a large quantity maternal blood [2-4]. For example, Thomas et al [3] observed the presence of redistribution in the fetoplacental circulation in their 2 cases of MSH by Doppler ultrasound examination. Recently, we encountered a case of monochorionic-diamniotic twin pregnancy complicated by MSH observed after 28 weeks of gestation which led to the changes in fetal circulation of the both twins.
| Case Report | ▴Top |
A 32-year-old woman, gravida 1, para 0 was referred to our hospital at 14 weeks of gestation for a high-risk obstetric consultation due to monochorionic-diamniotic twin pregnancy. The medical and genetic family and past histories of the patient and her husband were unremarkable. During the first trimester of the twin pregnancy, there were no complications such as infection, anemia or trauma in the patient. At this time, in addition, there was no measurable discordance between amniotic fluid pockets or fetal weights.
At 20 weeks of gestation, however, ultrasound examination revealed an amniotic fluid discordance between the twins (amniotic fluid pocket: Twin A 2.1 cm, Twin B 6.8 cm). There was 20.3% discordance between fetal weights (estimated fetal weight: Twin A 294 g, Twin B 369 g). Thus, weekly ultrasound examination including Doppler evaluations of umbilical and cerebral arteries of both twins was performed thereafter. Figure 1 shows the changes in the amniotic fluid pocket in the both twins during pregnancy.
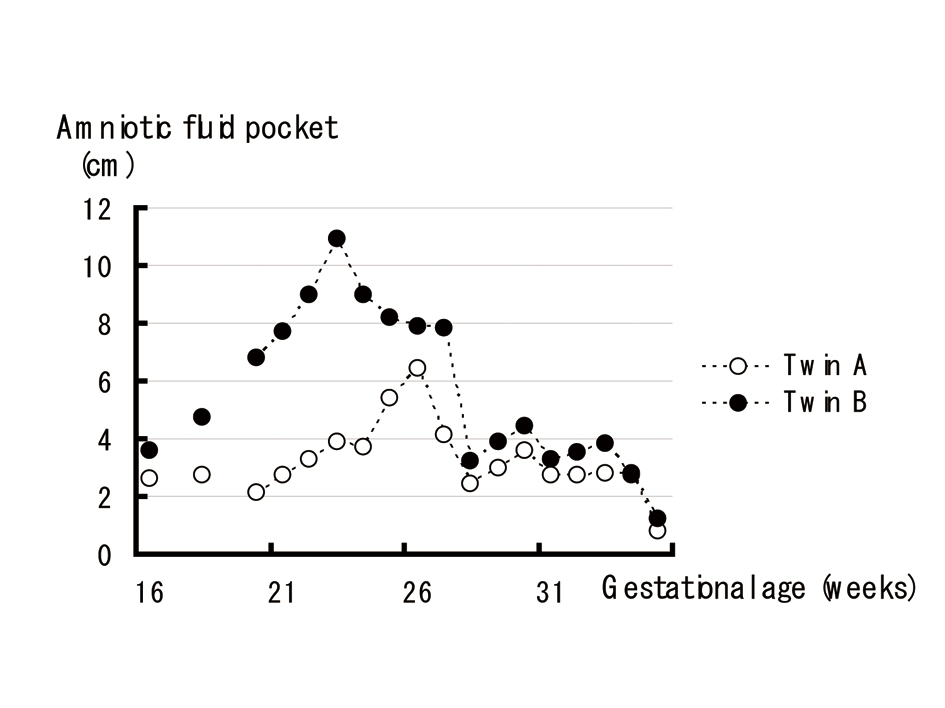 Click for large image | Figure 1. The changes in the amniotic fluid pocket in the both twins. |
At 28 weeks of gestation, ultrasound examination revealed a large homogenous and hyperechoic zone at the Twin A’s side of the placenta (6 × 4 cm) (Fig. 2). The amniotic fluid pockets of Twin A and B were decreased from 4.1 and 7.8 cm at 27 weeks to 2.4 and 3.2 cm at 28 weeks of gestation, respectively. Because the patient felt irregular uterine contraction, she was admitted for tocolysis with MgSO4 infusion until delivery (24 g/day).
 Click for large image | Figure 2. A large homogenous and hyperechoic zone at the Twin A’s side of the placenta (arrows: 6 × 4 cm) by ultrasound examination. |
At 35 weeks and 4 days of gestation, the fetal cardiotocograms showed severe variable decelerations in Twin A. In addition, ultrasound examination revealed an increased hyperechoic zone (15 × 10 cm) (Fig. 3) and oligohydramnios in the both twins (amniotic fluid pocket: Twin A 1.2 cm, Twin B 0.8 cm). An emergency cesarean section was performed. Twin A was a female baby weighing 1,632 g (light for gestational age) with Apgar score of 8 (1 min) and 9 (5 min), respectively, while Twin B was a female baby weighing 2,102 g (appropriate for gestational age; 22.4% growth discordance between the twins) with Apgar score of 8 (1 min) and 9 (5 min), respectively. The umbilical artery pH in Twin A and B were 7.313 and 7.363, respectively. The umbilical venous hemoglobin level in Twin B was 18.0 g/dL (normal: 13 - 22 g/dL), while it was 12.6 g/dL with reticulocyte counts 10.7% (normal: < 7%) in Twin A.
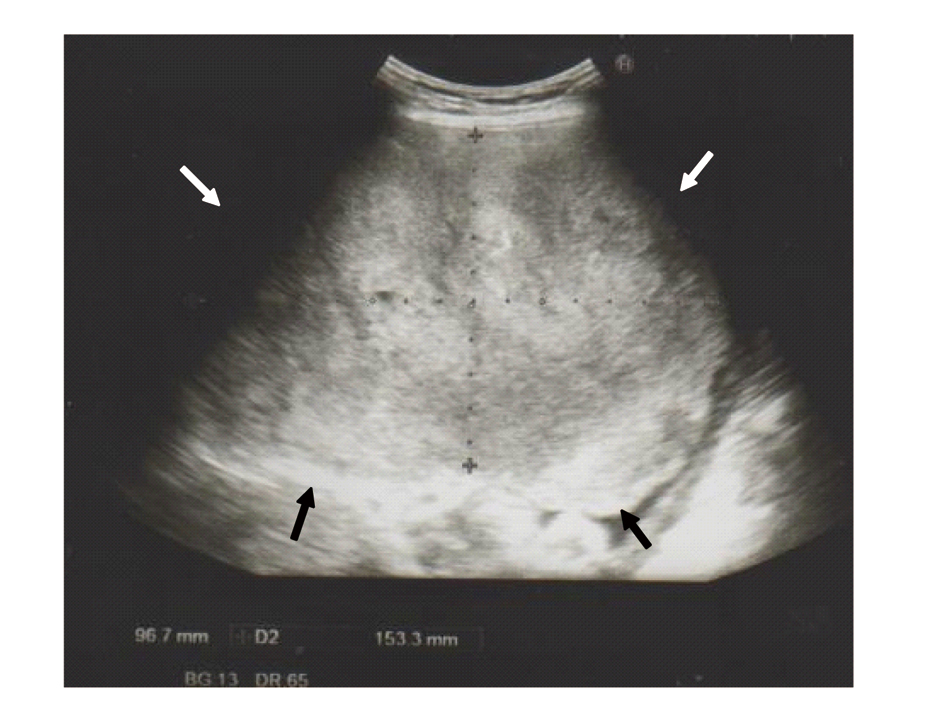 Click for large image | Figure 3. An increased hyperechoic zone (arrows: 15 × 10 cm) by ultrasound examination. |
During manual removal of the placenta, an escape of dark blood of about 1,000 mL with no clots was noted from subchorionic space of the placenta. The placenta measured 20 × 17 × 3 cm and weighed 920 g. There was a subchorionic space in the base of the fibrosis of the placenta in which we speculated a large quantity of blood was stored. The hemorrhage did not extend beneath the insertion of the umbilical cord of Twin A or B. Microscopically, the subchorionic infarction, hemorrhage and chorioamnionitis of the placenta were confirmed.
| Discussion | ▴Top |
This may be the first case report of twin pregnancy complicated by MSH which led to the changes in fetal circulation of the both twins.
In the current case, the presence of MSH seemed to affect the circulation of fetus in the hemorrhagic side (Twin A) as well as the circulation of another fetus (Twin B) after 28 weeks of gestation. In Twin A, the presence of MSH caused chronic anemia and oligohydramnios, eventually it led to non-reassuring fetal status. These consequences might be due to uteroplacental circulatory insufficiency from MSH. In this case, in addition, MSH led to oligohydramnios in Twin B. The cause of the oligohydramnios in Twin B is unclear, either due to the uteroplacental circulatory insufficiency through the massive placental hemorrhage or due to fetoplacental circulatory failure through the placental vascular anastomoses between the twins. Therefore, a further concerning may be needed with the accumulation of similar case reports.
Although we cannot deny the insufficiency of the consideration and/or inspection in the present case, the clinical importance of MSH was re-realized with this case.
Conflict of Interests
The authors report no conflicts of interest.
| References | ▴Top |
- Breus C. Das Tuberose Subchoriale Haematom der Decidua. Leipzig, Deuticke, 1892.
- Shimizu I, Shikado K, Mituda N, Iwata M, Nagata M, Fuke S, Bekku S, Wasada K, Kawamoto A, Nakayama M, Suehara N. Ultrasonographic findings in massive subchorionic hematoma (Breus' mole). Ultrasound Obstet Gynecol 1995;6(suppl):163.
- Thomas D, Makhoul J, Muller C. Fetal growth retardation due to massive subchorionic thrombohematoma: report of two cases. J Ultrasound Med. 1992;11(5):245-247.
pubmed - Tam WH, Fung HY, Fung TY, Lau TK, To KF. Intra-uterine growth retardation and transverse lie due to massive subchorionic thrombohematoma and overlying large subchorionic cyst. Acta Obstet Gynecol Scand. 1997;76(4):381-383.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
