| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Original Article
Volume 2, Number 2, September 2013, pages 76-80
Microvascular Density as a Parameter of Endometrial Assessment in Infertile Women
Pooja Jaina, e, Shipra Paulb, Usha Guptac, Anita Tulib, Manjula Jaind
aAnatomy department, All India Institute of Medical Sciences (AIIMS), New Delhi, India
bDepartment of Anatomy, Lady Hardinge Medical College, New Delhi, India
cDepartment of Obstetrics and Gynaecology, Lady Hardinge Medical College & Smt Sucheta Kriplani Hospital, New Delhi, India
dDepartment of pathology, Lady Hardinge Medical College & Smt Sucheta Kriplani Hospital, New Delhi, India
eCorresponding author: Pooja Jain, Department of Anatomy, Teaching block, AIIMS, Ansari nagar, 29 Aurobindo Marg, New Delhi-110029, India
Manuscript accepted for publication June 19, 2013
Short title: Endometrial Microvascular Density
doi: https://doi.org/10.4021/jcgo168w
| Abstract | ▴Top |
Background: A good blood flow towards the endometrium is an essential prerequisite for its development and differentiation, for the implantation of blastocyst and continuation of pregnancy. Diminished endometrial perfusion may be the one of the important reason behind the patients with unexplained infertility. The present study was carried out to estimate the cut-off of microvascular density determinative of good endometrial receptivity.
Methods: The study included 60 patients who qualified the exclusion and inclusion criteria. Transvaginal Doppler ultrasonographic examination was performed for all patients prior to the scheduled premenstrual biopsy to determine sub endometrial blood flow. The biopsied endometrial tissue was processed. The blood vessels were identified in endometrial tissue and counted in 5 high power fields/slide. Total area of the field was calculated using stage micrometer. The density of the vessels was calculated as number of vessels/mm2 of the fields.
Results: Three vascular penetration zones based on Doppler ultrasonographic examination were identified as zone 1, zone 2, and zone 3 i.e. poor, intermediate and good vascularity respectively. The endometrial microvascular density in patients with vascularity falling in zone 1, zone 2, and zone 3 were 14.18 ± 4.07 vessels/mm2, 24.53 ± 4.65 vessels/mm2 and 42.3 ± 6.1 vessels/mm2 respectively. Comparative observation between Doppler and microvascular density revealed that in all patients with zone 3 vascularity, the microvascular density was more than 35 vessels/mm2.
Conclusions: A quantitative parameter was obtained from this study which identifies good endometrial receptivity and predicts the fertility of the patient which can be used as a prognostic marker in infertile patients particularly in developing countries.
Keywords: Endometrial receptivity; Microvascular density; Human endometrium; Endometrial perfusion
| Introduction | ▴Top |
The natural conception depends upon good general health status of the couple. Infertility affects about 10% of all couples of which female factor alone comprises 50 - 60% of the cases. Female infertility is a representation spectrum of causes ranging from the abnormalities in oogenesis, tubal disorders to diminished endometrial receptivity [1]. Endometrial receptivity can be an important determinant of fertility in woman with unexplained causes. Preparation of a receptive endometrium requires changes in its pattern, thickness and angiogenesis which are accompanied by the increase in vascular permeability that not only supports endometrial proliferation but at the same time transforms thin dense endometrium into thick, highly permeable secretory endometrium [2]. Implantation of the fertilized ovum in endometrium is a dynamic process [3, 4]. Through the menstrual cycle, the endometrium undergoes a precisely defined morphological change that establishes a receptive endometrium [5-7]. A good blood supply towards the endometrium is an essential prerequisite for successful implantation. Implantation failure may be directly related to the insufficient uterine perfusion [8, 9]. Since the adequate blood flow is a basic requirement in implantation and maintenance of pregnancy [10], the present study was undertaken to assess endometrial vascularity by Doppler velocimetry and to compare it with morphometric analysis of vascular density on histopathological study of the endometrium in infertile women.
| Materials and Methods | ▴Top |
The present study was conducted in the Department of Anatomy in collaboration with Department of Obstetrics & Gynaecology and Department of Pathology of Lady Hardinge Medical College and Smt. Sucheta Kriplani hospital, New Delhi. 150 patients attending gynaecology OPD with history of primary or secondary infertility were considered for the study. These patients were subjected to routine investigations of infertility as per the hospital’s protocol to rule out known causes of infertility. Husband’s semen analysis was done as per standard WHO guidelines to rule out male factors of infertility. Routine haematological examinations i.e. complete blood count with ESR, blood sugar, VDRL, liver and kidney function test were done to rule out metabolic factors. Transabdominal Ultrasonography was done for all patients and those with known causes like uterine malformations, fibroids, Asherman’s syndrome, tubercular endometritis and tubal blockage were excluded. Tubal patency was determined by hystero-salpingography (HSG).
After the preliminary investigations 60 patients with unknown causes of infertility were included in the study group. This included patients in the age group of 20 - 35 years. Maximum number of patients i.e. 41 had a period of infertility ranging between 1 - 5 years, 14 had infertility for 6 - 10 years while 5 patients had a prolonged period of infertility i.e. 11 - 15 years. 39 patients of the study group were the cases of primary infertility with no prior documented conception while 21 patients had one or more documented conception not necessarily a live birth i.e. secondary infertility.
These patients were then followed with Doppler ultrasonographic examination with a 5 MHz endovaginal probe using Nemio XG SSA-580A (Toshiba), which was performed during secretory phase of the endometrial cycle (day 24/25) just prior to the scheduled endometrial biopsy. Endometrial tissue was collected using 022720 MedGyn Endosampler (25/bx), the endometrial sampling device. The tissue thus obtained was fixed in formalin, dehydrated, embedded in paraffin and sectioned (4 - 6 µm thickness). It was stained with Haematoxylin & Eosin stain and observed under light microscope (Fig. 1).The blood vessels were identified and counted in 5 high power fields/slide. Vessel concentration or density is defined as average number of vessel cross-section counted within one eyefield at 400x magnification. Total area of the field was calculated using stage micrometer. The density of the vessels was calculated as number of vessels/mm2. Three slides were studied per patient and the average vessel density calculated.
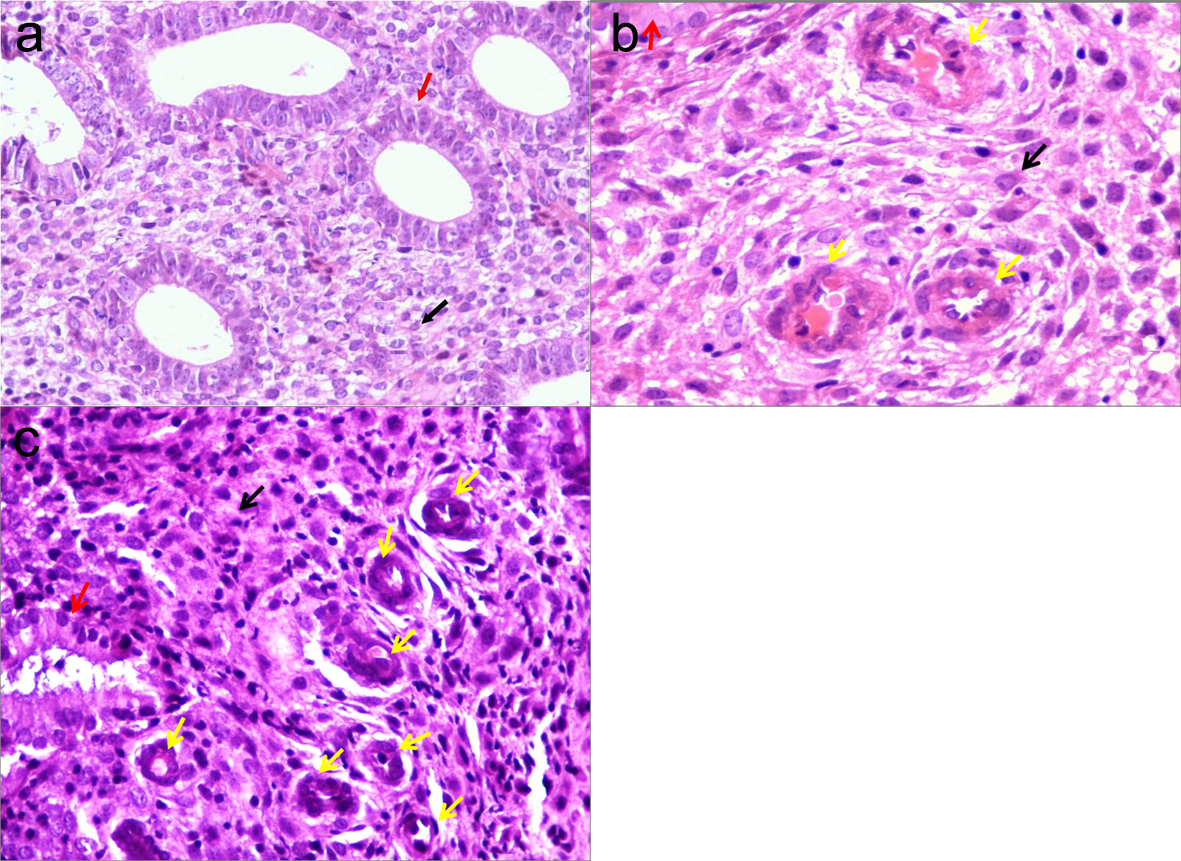 Click for large image | Figure 1. Photomicrograph showing poor (a), intermediate (b) and good (c) endometrial vascularity (400 X). Black arrow: stroma. Red arrow: endometrial glands. Yellow arrow: blood vessels. Flowchart of study subjects. |
| Results | ▴Top |
The mean of microvascular density for all the patients was found to be 24.75 ± 11.40 vessels/mm2. The histological changes in the endometrium correspond to the cyclical changes in a menstrual cycle. When the histological dating is within a day of the chronological date the endometrium is known as in phase and when the difference is more than a day it is out of phase endometrium. The mean microvascular densities in patients with proliferative, secretory (out of phase) and secretory (in phase) endometrium were 13.63 ± 4.22vessels/mm2, 18.4 vessels/mm2 and 29.32 ± 10.42 vessels/mm2 respectively (Fig. 2). The range of microvascular density of all patients with secretory (in phase) endometrium was seen to be falling between 11.2 to 53.5 vessels/mm2. On extensive literature search no prior study of the microvascular density in endometrium of fertile women was available i.e. a cut-off value to determine good endometrial vascularity was not available, the colour doppler findings of endometrial vascularity were taken as gold standard for comparison of microvascular density on HPE. Colour Doppler imaging was performed in all patients just before the patients were subjected to endometrial biopsy to identify the degree of endometrial vascular penetration i.e. endometrial vascularity. The endometrium of the patients was categorized as per vascular penetration in three zones [11].
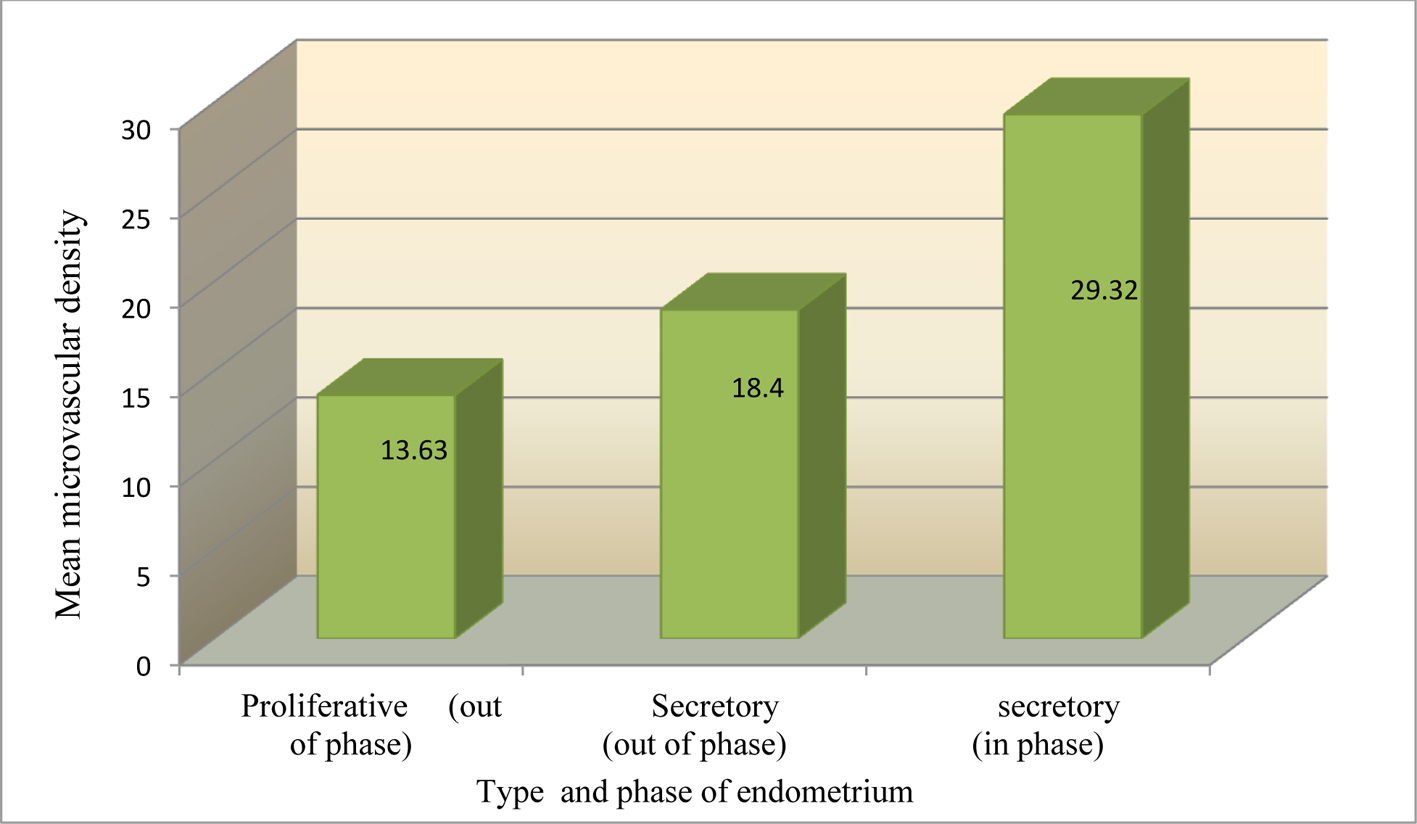 Click for large image | Figure 2. Mean microvascular density (vessels/mm2) in patients with proliferative, secretory (out of phase), and secretory (in phase) endometrium. |
Zone 1 (poor vascularity): the vascular penetration was present only in the myometrium or the outermost endometrial lining (Fig. 3a).
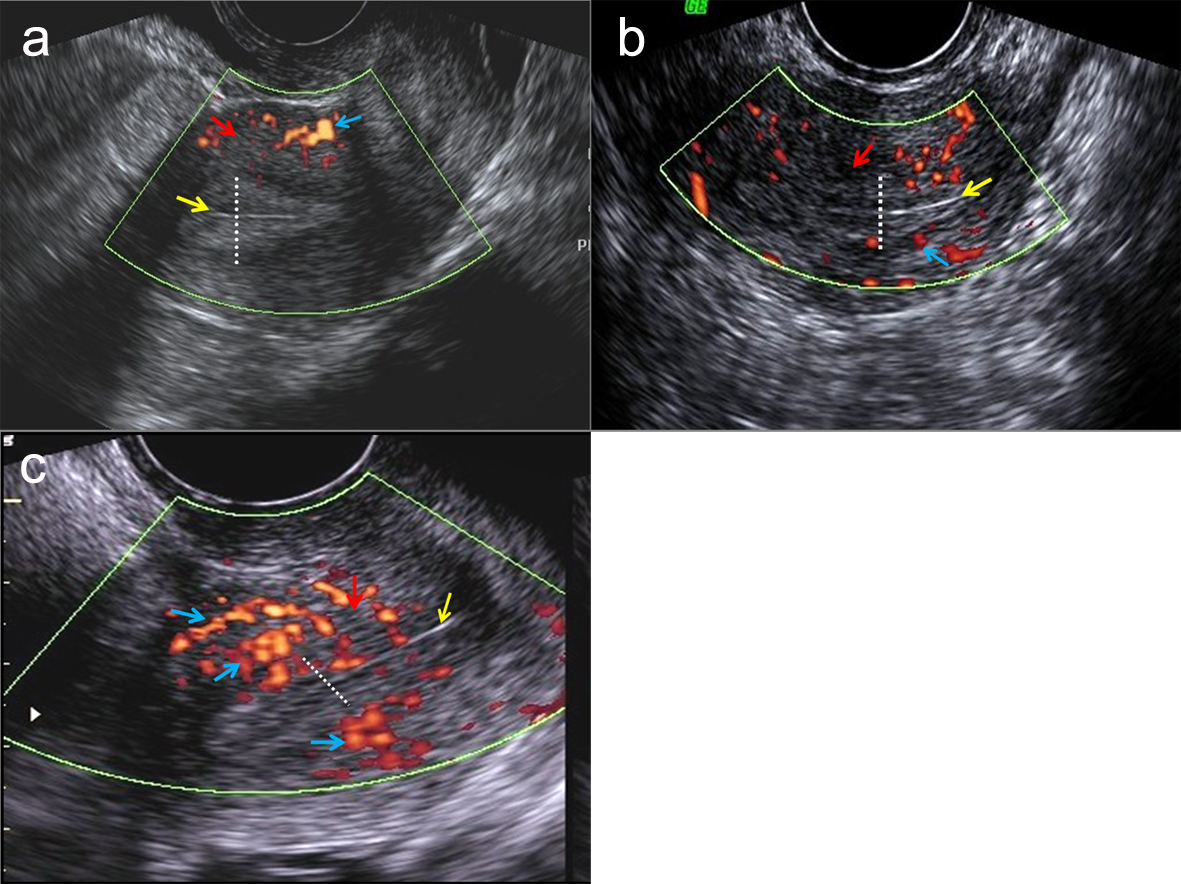 Click for large image | Figure 3. Doppler photographs showing different levels of vascular penetration-zone1 (a), zone 2 (b) and zone 3 (c). Dotted line: extent of endometrium. Yellow arrow: innermost endometrial lining. Red arrow: myometrium. Blue arrow: vascularity as seen as red patches. |
Zone 2 (intermediate vascularity): the vascular penetration present in the outer half of the endometrial thickness, not reaching till its innermost lining (Fig. 3b).
Zone 3 (good vascularity): vascular penetration present in whole of the endometrium i.e. till its innermost endometrial lining (Fig 3c).
The total numbers of patients were now distributed according to the Doppler zones of vascularity. Majority of the patients fell in Zone 1 and Zone 2 i.e. poor and intermediate vascularity being 21patients (35%) and 26 patients (43.33%) respectively, while only 13 patients (21.67%) were found to have vascular penetration till innermost endometrial lining i.e. Zone 3. The mean of microvascular density (MVD) in patients with Zone 3, Zone 2 and Zone 1 vascularity was found to be 42.3 ± 6.1 vessels/mm2, 24.53 ± 4.65 vessels/mm2 and 14.18 ± 4.07 vessels/mm2 respectively. This difference of mean microvascular density in patients with Doppler vascular penetration zones was highly significant (p < 0.01). In patients with zone 3 Doppler vascularity, the MVD was invariably found to be ranging between 35 - 53.5 vessels/mm2. Thus, the MVD > 35 vessels/mm2 was labelled as good vascularity. Similarly in all patients with Zone 2 Doppler vascularity the microvascular density was found in the range of 20 - 35 vessels/mm2. Therefore the microvascular density of 20 - 35 vessels/mm2 was labelled as intermediate, whereas < 20 vessels/mm2 as poor vascularity.
| Discussion | ▴Top |
The endometrium undergoes increase in the thickness and vascularity through the menstrual cycle which is required for the implantation of the fertilized ovum. Poor uterine perfusion can be one of the important reasons behind the cases of unexplained infertility [8]. Chien et al observed a significantly higher pregnancy and implantation rates in patients with increased vascularity as compared to the patients in which there was no detectable blood flow on Doppler [12]. Similar observation was made in the present study, where the total 5 patients who subsequently conceived, 4 (30.76%) belonged to the patient group of 13 patients with good vascularity i.e. vascularity reaching till the innermost endometrial lining while 1 (7.69%) belonged to patient group with (26 patients) intermediate vascularity. No conception was noted in the patient group (21 patients) with poor vascularity. The higher conception rate in patients with good vascularity supports the conjecture that a good blood flow is an important determinant of endometrial receptivity.
A significantly greater microvascular density was observed by Blackwell et al in the secretory phase endometrium i.e. 25.0 ± 12.7 vessels/sq mm as compared to 12.2 ± 6.3 vessels/sq mm (p < 0.005) in mid-proliferative phase [13]. Similarly in the present study the mean microvascular density was 29.32 ± 10.42 vessels/mm2 in secretory (in phase) endometrium as compared to 18.4 vessels/mm2 in secretory (out of phase) and 13.63 ± 4.22 vessels/mm2 in the proliferative endometrium (p = 0.000). Makhija et al in their study on morphometric evaluation of endometrial blood vessels have compared mean blood vessel concentration in 17 endometrial specimens of infertile patients with 63 endometrial samples taken as controls. It was observed that there was no statistically significant difference in the mean blood vessel concentration, congestion or dilatation between control and the infertile group. Makhija et al reported a lower concentration of the endometrial vessels of 3.86 ± 0.71/ high power fields as compared to the mean microvascular concentration of 4.86 ± 2.23 vessels/ high power fields (equivalent to 24.75 ± 11.40 vessels/mm2 under 40x magnification) in the present study [14].This difference in the mean microvascular concentration may be due to the fact that it was not clear in their study regarding the cause of infertility i.e. the type of endometrial biopsy, phase of menstrual cycle, as compared to the present study where only the patients with uterine causes of infertility were taken and endometrial tissue was obtained only in the premenstrual phase.
Comparative observation between Doppler and microvascular density revealed that in all patients with zone 3 vascularity, the microvascular density was more than 35 vessels/mm2. In all patients with zone 2 vascularity, the microvascular density was found in the range between 20 - 35 vessels/mm2. Therefore in the present study the vascularity more than 35 vessels/mm2 was considered as good, between 20 - 35 vessels/mm2 as intermediate and less than 20 vessels/mm2 as poor. Thus a quantitative parameter was obtained from this study which defines good endometrial receptivity and predicts the fertility of the patient which can be used as a prognostic marker in infertility patients. Microvascular endometrial density is a cost effective alternate to the Doppler studies which can determine patient’s endometrial vascularity vis a vis receptivity at places like peripheral health centers where doppler facilities are not available. Study of endometrial microvascular density in infertile women widens the horizon of treatment to the treating gynecologists and drugs that improve uterine blood flow and hence the receptivity.
Acknowledgments
The study was financially supported by Lady Hardinge Medical College (LHMC), New Delhi. The authors express sincere thanks to the resident doctors and the technical staff of LHMC for their contribution to the work, without which the study would not have taken its present form.
Disclosure
There is absence of any financial interest in the information contained in the present manuscript by any company or institute.
| References | ▴Top |
- Raine-Fenning NJ, Campbell BK, Kendall NR, Clewes JS, Johnson IR. Endometrial and subendometrial perfusion are impaired in women with unexplained subfertility. Hum Reprod. 2004;19(11):2605-2614.
doi pubmed - Kohnen G, Campbell S, Jeffers MD, Cameron IT. Spatially regulated differentiation of endometrial vascular smooth muscle cells. Hum Reprod. 2000;15(2):284-292.
doi pubmed - Smith SK. Angiogenesis and implantation. Hum Reprod. 2000;15(Suppl 6):59-66.
pubmed - Rogers PA, Abberton KM. Endometrial arteriogenesis: vascular smooth muscle cell proliferation and differentiation during the menstrual cycle and changes associated with endometrial bleeding disorders. Microsc Res Tech. 2003;60(4):412-419.
doi pubmed - Check JH, Nowroozi K, Choe J, Dietterich C. Influence of endometrial thickness and echo patterns on pregnancy rates during in vitro fertilization. Fertil Steril. 1991;56(6):1173-1175.
pubmed - Dickey RP, Olar TT, Curole DN, Taylor SN, Rye PH. Endometrial pattern and thickness associated with pregnancy outcome after assisted reproduction technologies. Hum Reprod. 1992;7(3):418-421.
pubmed - Noyes N, Liu HC, Sultan K, Schattman G, Rosenwaks Z. Endometrial thickness appears to be a significant factor in embryo implantation in in-vitro fertilization. Hum Reprod. 1995;10(4):919-922.
pubmed - Goswamy RK, Williams G, Steptoe PC. Decreased uterine perfusion—a cause of infertility. Hum Reprod. 1988;3(8):955-959.
pubmed - Raine-Fenning NJ, Campbell BK, Kendall NR, Clewes JS, Johnson IR. Quantifying the changes in endometrial vascularity throughout the normal menstrual cycle with three-dimensional power Doppler angiography. Hum Reprod. 2004;19(2):330-338.
doi pubmed - Steer CV, Tan SL, Mason BA, Campbell S. Midluteal-phase vaginal color Doppler assessment of uterine artery impedance in a subfertile population. Fertil Steril. 1994;61(1):53-58.
pubmed - Ahmadi F, Vosough A, Irani S and Zafarani F. Correlation between Endometrial Parameters in Doppler Sonography and Success Rate of Implantation in Assisted Reproductive Program. Iran J Fertil Steril. 2007; 1(2): 63-68.
- Chien LW, Au HK, Chen PL, Xiao J, Tzeng CR. Assessment of uterine receptivity by the endometrial-subendometrial blood flow distribution pattern in women undergoing in vitro fertilization-embryo transfer. Fertil Steril. 2002;78(2):245-251.
doi - Blackwell PM, Fraser IS. A morphometric and ultrastructural study of the microvessels of the functional zone of normal human endometrium with some notions on possible secretory functions of the endothelial cells. Asia Oceania J Obstet Gynaecol. 1988;14(2):233-250.
doi pubmed - Makhija D, Mathai AM, Naik R, Kumar S, Rai S, Pai MR, Baliga P. Morphometric evaluation of endometrial blood vessels. Indian J Pathol Microbiol. 2008;51(3):346-350.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
