| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 2, Number 1, June 2013, pages 38-41
Recurrent Non-Peutz-Jeghers Syndrome Associated Ovarian Sex Cord Tumor With Annular Tubules: A Case Report With Literature Review
Amal Abd El-hafez Abd El-mageeda, c, Amir Monir Shafikb
aPathology Department, Faculty of Medicine, Mansoura University, Egypt
bRadiology Department, Faculty of Medicine, Mansoura University, Egypt
cCorresponding author: Amal Abd El-hafez Abd El-mageed, Radiology department, Saudi German Hospital, Madinah Munwarah, Saudi Arabia
Manuscript accepted for publication March 19, 2013
Short title: Sex Cord Stromal Tumor With Annular Tubules
doi: https://doi.org/10.4021/jcgo141e
| Abstract | ▴Top |
This report describes the late recurrence of an unusual ovarian neoplasm namely sex cord stromal tumor with annular tubules (SCTAT). This tumor was detected in a non-Peutz-Jeghers syndrome (PJS) female patient aging 54-years after 9 years of primary surgery. The patient undergone pelvic ultrasonography and MRI followed by laparotomy for frozen section. Total abdominal hysterectomy and bilateral salpingo-oophorectomy were performed. Microscopic examination revealed diagnostic features of SCTAT. A review of the literature reporting the clinico-pathologic features, differential diagnosis and the biologic behavior of SCTAT in patients with and without PJS is presented. In addition immunohistochemical profile was assessed for sex cord tumor markers. This report highlights the importance of considering the pathological features and behavior of SCTAT during the diagnosis and management of patients with ovarian neoplasia.
Keywords: Sex cord tumor with annular tubules; Immunohistochemistry; Recurrent; WT-1; Calretinin; Inhibin
| Introduction | ▴Top |
Sex cord tumor with annular tubules (SCTAT) is an unusual variant of ovarian neoplasms, first described by Scully in 1970 [1]. About one third of SCTATs are Peutz-Jeghers (PJS) syndrome associated and the remainder is sporadic. SCTATs have been reported in patients ranging in age from 4 to 76 years [2]. Controversy exists whether these tumors are related to Sertoli cell or granulosa cell tumors [3]. Because of its unique features, SCTAT was suggested to be placed in a separate category [1]; therefore, the World Health Organization included it in the category of mixed/unclassified cell-type sex cord-stromal cell tumors [4]. SCTAT may induce isosexual precocity, menstrual irregularities or postmenopausal bleeding [2, 5]. PJS associated tumors are almost benign, bilateral, multifocal, calcified, very small (less than 3 cm) or even discovered accidentally. In contrast, sporadic SCTATs are unilateral and large and may have a malignant behavior [6, 7].
This report describes an exceptional case of recurrent non-Peutz-Jeghers syndrome associated ovarian SCTAT arising in a 54-year-old woman after 9 years of primary surgery emphasizing its clinical, radiological and histo-pathological features with its differential diagnosis and immunohistochemical profile.
| Case Report | ▴Top |
A 54-year-old woman presented with irregular vaginal bleeding and a palpable pelvi-abdominal mass. The patient had history of previous excision of a pelvic mass since 9 years diagnosed as “adult granulosa cell tumor without atypia or mitotic activity”. Subsequently, the patient did not receive chemo or radiotherapy. After clinical examination, no diagnostic clinical features of Peutz-Jeghers Syndrome were detected (for example, gastrointestinal polyps with melanin spots on the oral mucosa, lips, and skin).
Radiological examination
Pelvic ultrasoography demonstrated a solid and cystic mass occupying the region of the right ovary, with minimal free ascites. The mass was suspicious of malignancy. Pelvic MRI (Fig. 1) was performed and revealed an irregular mixed cystic and solid mass of heterogeneous signal intensity involving the mid and right pelvis with multiple hemorrhagic components and minimal surrounding fluid reaction.
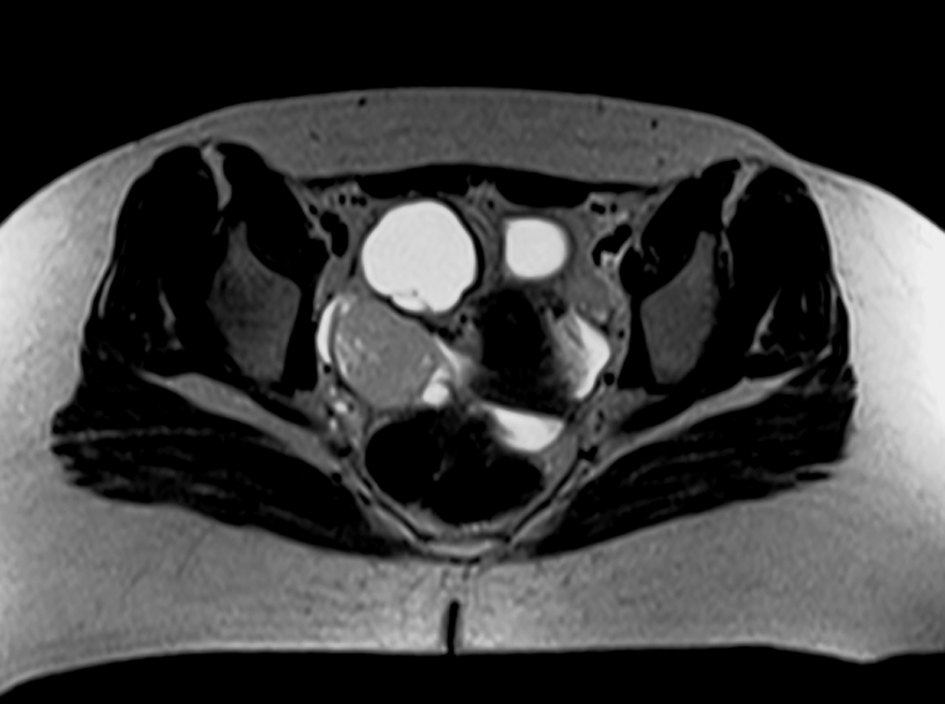 Click for large image | Figure 1. MRI of the pelvis, axial section demonstrating a mid and right pelvic irregular mixed cystic and solid mass of heterogeneous signal intensity. |
Operative procedure
The patient was subjected laparotomy for frozen section and pathological diagnosis, then, total abdominal hysterectomy and bilateral salpingo-oophorectomy were performed. At surgery, the tumor tissue was adherent to adjacent pelvic structures and could not be completely excised.
Macroscopic examination
On gross pathological examination, the right ovary was totally replaced by an irregular mass, firm in consistency measuring nearly 14 × 9 × 7.5 cm. Cut section showed tan yellow surface with small cystic areas ranging in diameter from 0.2 to 1.5 cm. and foci of hemorrhage and necrosis. Residual normal ovarian tissue was not identified. The uterus, cervix, fallopian tubes and the left ovary appeared normal.
Microscopic examination
The resection specimen was processed routinely and histopathology sections were prepared and stained with hematoxylin and eosin (H&E). Histologically, the right ovarian mass was completely formed of tumor having the typical cytoarchitectural features of SCTAT. Simple and complex annular tubules of various sizes were revolving around central hyaline cores of basement membrane-like material. Tumor cells were columnar with eosinophilic to pale cytoplasm and round nuclei. The nuclei were arranged in an antipodal fashion around both the central core and the periphery of individual tubules. Tumor cells showed minimal atypia and no mitosis (Fig. 2a, b). In addition, there were few foci of more elongated tubule-like structures simulating Sertoli cell tumor (Fig. 2c) and a microscopic focus of cells arranged in a diffuse pattern resembling granulosa cell tumor and microcysts (Fig. 2b). Furthermore, review of the original histologic slides revealed the same microscopic findings with the predominance of granulosa cell tumor-like foci. The left ovary did not show tumor deposits. The uterine cervix was free of both squamous and glandular neoplasia. The endometrium had a disordered proliferative pattern.
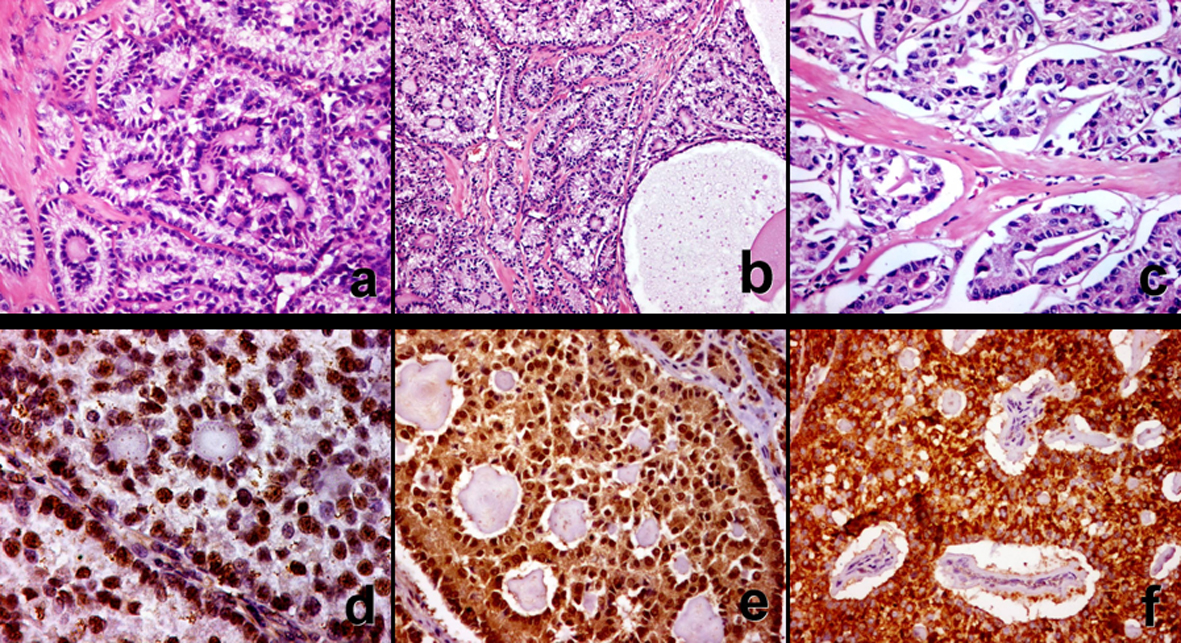 Click for large image | Figure 2. Ovarian sex cord tumor with annular tubules in non- Peutz-Jeghers syndrome patient. It shows simple and complex tubules and the typical antipodal arrangement of tumor cells, which encircle hyaline basement membrane-like material. Foci simulating Sertoli cell tumor (c). Strong diffuse immunohistochemical staining for Wilms’ tumor-1(d), calretinin (e), and inhibin-α (f). |
Immunohistochemistry
In order to assess the immunohistochemical profile, formalin fixed paraffin embedded tumor sections were stained for the followings: Wilms’ tumor-1 gene Protein (WT-1, Ab-4, and Clone WLM04 Lab-vision); anti-calretinin antibody (Zymed corporation product CMA758) and inhibin-α (Ab-1, Clone R1 Lab-vision). The standard avidin-biotin technique was applied using diaminobenzidine (DAB) for visualization and hematoxylin for counterstaining. Immunohistochemistry revealed diffuse and strong nuclear staining of tumor cells for WT-1, both nuclear and cytoplasmic staining for calretinin and cytoplasmic staining for inhibin-α (Fig. 2d, e, f).
| Discussion | ▴Top |
Sex cord tumor with annular tubules (SCTAT) applies for a peculiar form of ovarian tumors, which caused curiosity about its histogenesis and differentiating potentiality [1, 2].
This report describes an unusual manifestation of an exceptional tumor, namely, the late recurrence of ovarian sex cord tumor with annular tubules (SCTAT) after 9 years of primary tumor excision in a woman aging 54 years. In literature, the reported time of first recurrence in cases of malignant SCTAT ranged from 3 months to 20 years [2, 8, 9].
Although SCTAT is capable of producing estrogen, progesterone and mullerian inhibiting substance, estrogenic manifestations were frequently reported in patients with SCTAT whether or not they have PJS syndrome [10]. This case was presented by symptoms of hyperestrinism evidenced microscopically by the finding of disordered proliferative endometrium. Adherence to pelvic structures, which was documented in only one previous report of malignant SCTAT [8], was present in our case despite the bland microscopic findings, on the contrary, other case reports did not describe adherence to pelvic structures [2, 6, 8, 9].
Some studies proposed that SCTAT should be grouped with Sertoli cell tumors because of its tubular pattern, lack of neoplastic stromal component and the presence of the distinctive ultrastructural finding of Sertoli cells, Charcot-Bottcher crystals, in some cases. In addition, all other ovarian neoplasms associated with Peutz-Jegher syndrome are Sertoli cell tumors [8]. Others supported the closer relation to granulosa cell tumors based on focal merging of histologic patterns and similar ultrastructural features [3]. Yet, there is some consensus that the tumor is composed of primitive cells of sex cord origin which have a potential for differentiating into either granulosa or Sertoli cells [11]. In this case, the histologic findings of simple and complex annular tubules encircling central hyaline masses were typical of SCTAT. Despite the presence of foci of Sertoli-like tubules, in our case, the primary tumor more closely resembled granulosa cell tumor showing a diffuse pattern of tumor cell arrangement and microcysts. These findings suggest a closer relation to granulosa cell tumor. This is not surprising because SCTAT may contain additional histologic patterns, particularly in cases in not associated with the PJS [1, 2, 10]. On the contrary, other study did not find neither solid nor hollow tubules typical of Sertoli cell tumor nor foci histologically resembling granulosa cell tumor observed [6].
The malignant potential of SCTAT cannot be reliably predicted by microscopic examination of the primary tumor and the reported mitotic counts ranged from rare to 7 to 10 mitoses per 10 high power fields [2, 8, 12]. In agreement with that, the reported case imparted bland cellular features and mitosis was sparse.
The differential diagnosis of SCTAT includes Brenner tumor, Sertoli-cell tumor, granulosa cell tumor and gynandroblastoma [1]. The resemblance between SCTAT and gonadoblastoma can be striking but they are differentiated by the presence of germ cell elements in the latter [13]. The wide differential diagnosis and the relative rarity of SCTAT may explain the misdiagnosis of our case as granulosa cell tumor in the primary resection.
Very few studies have tested immunohistochemical profile of SCTAT. To approve the immunohistochemical profile of SCTAT, we applied the panel suggested by Deavers et al [14], to diagnose most sex cord stromal tumors which includes: WT-1, calretinin and inhibin-α. In this report, SCTAT was strongly and diffusely positive for these three markers. This result recapitulates other previous studies [14, 15].
In conclusion, SCTAT represents a unique entity that must be taken in consideration during interpretation of a case of ovarian neoplasia to avoid diagnostic pitfalls and ensure proper case management. Its unusual behavior evidenced by delayed recurrence despite the bland cytologic features, as in our case, necessitates proper and long-term patient’s follow up. Yet, the diagnosis of SCTAT could be established on pathologic examination based on morphologic features of the tumor and the marker expression profile on immunohistochemistry.
Disclosure
No relevant financial affiliations or conflicts of interest to disclose.
| References | ▴Top |
- Scully RE. Sex cord tumor with annular tubules a distinctive ovarian tumor of the Peutz-Jeghers syndrome. Cancer. 1970;25(5):1107-1121.
doi - Young RH, Welch WR, Dickersin GR, Scully RE. Ovarian sex cord tumor with annular tubules: review of 74 cases including 27 with Peutz-Jeghers syndrome and four with adenoma malignum of the cervix. Cancer. 1982;50(7):1384-1402.
doi - Roth LM. Recent advances in the pathology and classification of ovarian sex cord-stromal tumors. Int J Gynecol Pathol. 2006;25(3):199-215.
doi pubmed - Tavassoli FA, Devilee P. Pathology and genetics of tumors of the breast and female genital organs. World health organization classification of tumors. Lyon, IARC Press; 2003:113-202.
- Solh HM, Azoury RS, Najjar SS. Peutz-Jeghers syndrome associated with precocious puberty. J Pediatr. 1983;103(4):593-595.
doi - Lele SM, Sawh RN, Zaharopoulos P, Adesokan A, Smith M, Linhart JM, Arrastia CD, et al. Malignant ovarian sex cord tumor with annular tubules in a patient with Peutz-Jeghers syndrome: a case report. Mod Pathol. 2000;13(4):466-470.
doi pubmed - Young RH. Sex cord-stromal tumors of the ovary and testis: their similarities and differences with consideration of selected problems. Mod Pathol. 2005;18 (Suppl 2): 81–98.
doi pubmed - Tavassoli FA, Norris HJ. Sertoli tumors of the ovary. A clinicopathologic study of 28 cases with ultrastructural observations. Cancer. 1980;46(10):2281-2297.
doi - Shen K, Wu PC, Lang JH, Huang RL, Tang MT, Lian LJ. Ovarian sex cord tumor with annular tubules: a report of six cases. Gynecol Oncol. 1993;48(2):180-184.
doi pubmed - Song SH, Lee JK, Saw HS, Choi SY, Koo BH, Kim A, Yeom BW, et al. Peutz-Jeghers Syndrome with multiple genital tract tumors and breast cancer: a case report with a review of literatures. J Korean Med Sci. 2006;21(4):752-757.
doi pubmed - Moon WS, Lee DG. Ovarian sex cord tumor with annular tubules in a patient with Turner syndrome. J Korean Med Sci. 1998;13(1):89-94.
pubmed - Hart WR, Kumar N, Crissman JD. Ovarian neoplasms resembling sex cord tumors with annular tubules. Cancer. 1980;45(9):2352-2363.
doi - Talerman A, Roth LM. Recent advances in the pathology and classification of gonadal neoplasms composed of germ cells and sex cord derivatives. Int J Gynecol Pathol. 2007;26(3):313-321.
doi pubmed - Deavers MT, Malpica A, Liu J, Broaddus R, Silva EG. Ovarian sex cord-stromal tumors: an immunohistochemical study including a comparison of calretinin and inhibin. Mod Pathol. 2003;16(6):584-590.
doi pubmed - Zheng W, Senturk BZ, Parkash V. Inhibin immunohistochemical staining: a practical approach for the surgical pathologist in the diagnoses of ovarian sex cord-stromal tumors. Adv Anat Pathol. 2003;10(1):27-38.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
