| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Original Article
Volume 2, Number 2, September 2013, pages 56-60
Evaluation of Uterine Volume in Total Laparoscopic Hysterectomy for Uterine Leiomyomas
Aiko Shigemitsua, Naoto Furukawaa, b, Fuminori Itoa, Juria Akasakaa, Yasuhito Tanasea, Shozo Yoshidaa, Hiroshi Kobayashia
aDepartment of Obstetrics and Gynecology, Nara Medical University, 840 Shijo-cho, Kashihara, Nara, 634-8522, Japan
bCorresponding author: Naoto Furukawa, 840 Shijo-cho, Kashihara, Nara, 634-8522, Japan
Manuscript accepted for publication August 2, 2013
Short title: Evaluation of Uterine Volume
doi: https://doi.org/10.4021/jcgo179w
| Abstract | ▴Top |
Background: The aim of this retrospective study was to evaluate uterine volume in patients who underwent transabdominal hysterectomy (TAH) or total laparoscopic hysterectomy (TLH) for uterine leiomyomas in our teaching hospital and to determine the appropriate uterine volume in patients who could undergo TLH.
Methods: This retrospective study was based on a cohort 47 consecutive cases that underwent TLH for uterine leiomyomas in our institution between April 2008 and April 2012 (TLH group). Controls were defined as 134 patients who underwent TAH for uterine leiomyomas in our institution between April 2008 and April 2012 (TAH group).
Results: The TLH group comprised 45 cases because two surgeries in the TLH group were converted to TAH. Uterine volume was significantly smaller in the TLH group than in the TAH group (median 342 g vs. 788 g). Surgical duration was significantly longer in the TLH group than in the TAH group (median 214 minutes vs. 152 minutes). Blood loss was significantly lower in the TLH group than in the TAH group (median 0 mL vs. 250 mL). The incidence of postoperative complications was lower in the TLH group than in the TAH group (0/45 vs. 15/134). The hospital stay was significantly shorter for the TLH group than for the TAH group. In the TLH group, surgical duration correlated with uterine volume (regression coefficient = 1.6598, P = 0.0014).
Conclusion: There seems to be no limitation of uterine volume in TLH for uterine leiomyomas because TLH is safer than TAH except for the longer surgical duration.
Keywords: Total laparoscopic hysterectomy; Uterine volume; Leiomyoma
| Introduction | ▴Top |
Uterine leiomyomas, including fibroids or myomas, are frequent benign tumors of the uterus among women of reproductive age [1]. Treatment options for uterine leiomyomas include surgery, drugs, and embolization. Hysterectomy is commonly selected when patients do not wish to have more children or have hypermenorrhea. The number of laparoscopic hysterectomy procedures has recently increased, but transabdominal and transvaginal hysterectomies are also common approaches. In the United States, laparoscopic hysterectomies accounted for 30.5% of hysterectomy procedures in 2010 compared with 24.3% in 2007 [2]. The first laparoscopic access was combined with vaginal removal of the uterus and was referred to as laparoscopy-assisted vaginal hysterectomy (LAVH). In general, uterine vessel ligation and stump closure are performed vaginally in LAVH. This procedure, however, has now been replaced worldwide by total laparoscopic hysterectomy (TLH). In TLH, the uterine vessel, cardinal ligaments, and stump closure are performed laparoscopically, and thus TLH is more difficult than LAVH. A recent Cochrane review reported that laparoscopic hysterectomy is associated with less blood loss and a shorter hospital stay compared with abdominal hysterectomy [3]. In contrast, laparoscopic hysterectomy is associated with longer surgical duration and urinary tract injuries [4]. Uterine volume is also a factor in the selection of the hysterectomy approach. The reported cut-off uterine volume for laparoscopic hysterectomy is 280 g [5]. Few studies, however, have compared uterine volume with hysterectomy approach.
The aim of this retrospective study was to evaluate uterine volume in patients who underwent transabdominal hysterectomy (TAH) or TLH for uterine leiomyomas in our teaching hospital and to determine the appropriate uterine volume in patients who could undergo TLH.
| Patients and Methods | ▴Top |
This retrospective study was based on a cohort 47 consecutive cases that underwent TLH for uterine leiomyomas in our institution between April 2008 and April 2012 (TLH group). Controls were defined as 134 patients who underwent TAH for uterine leiomyomas in our institution between April 2008 and April 2012 (TAH group). Assignment of the hysterectomy approach was as follows; one patient was placed in the TLH group, and three consecutive subsequent patients were placed in the TAH group. Patient data were collected from the medical records.
Surgical procedure for TLH
After the induction of general anesthesia, patients were placed in a dorsal lithotomy position. A uterine manipulator (Thomas Medical Inc., Indianapolis, IN) was used. The pneumo-occluder was slipped over the tip and into the shaft, followed by attachment of an appropriately sized KOH ring. A 10 mm trocar was put through the umbilicus to hold the laparoscope with the mounted camera and create the pneumoperitoneum. Three 5 mm trocars were placed in the lower abdomen, with the lateral trocar positioned laterally to the epigastric vessels at the level of the superior iliac spine. After bringing the patient to Trendelenburg position, the round ligament was sealed and dissected using a Harmonic Ace (Johnson and Johnson, Tokyo, Japan), and the peritoneum was dissected down to the vesicouterine pouch using the Harmonic Ace. The bladder peritoneum was dissected from that of the uterus. The pararectal space was opened, and the external and internal iliac arteries were identified to visualize the ureters. By following the internal iliac artery, the origin of the uterine artery was identified. The uterine artery was completely isolated and sealed and dissected using the Harmonic Ace, or ligated by Vicryl (Johnson and Johnson) and dissected by scissors. The infundibulopelvic or utero-ovarian ligaments were sealed and dissected using the Harmonic Ace.
Circular colpotomy was performed along the rim of KOH ring using the Harmonic Ace and the uterus was removed. After detaching the uterus, it was extracted through the vagina if possible. If the uterus was too big, a morcellator (Olympus or Gyrus ACMI) was used through a 10 mm port after augmenting the left lateral access. The vagina was closed laparoscopically by running sutures with poly-dioxanone delayed absorbable sutures (PDSII; Johnson and Johnson). Finally, cystoscopy was performed to confirm urine flow from the ureters.
Statistical analysis
All statistical analyses were conducted using SPSS software Version 17 (SPSS Inc., Chicago, IL). The Chi2 test and Fisher’s exact test were used for analysis of categorical data. Quantitative measures were analyzed using the two-tailed unpaired Student’s t test. Probability values of less than 0.05 were considered to indicate statistical significance. Linear regression analysis was used to evaluate the relation between uterine volume and surgical duration.
| Results | ▴Top |
Two surgeries in the TLH group were converted to TAH, due to anesthesia problems and a large uterine volume of 1,320 g. The TLH group therefore comprised 45 cases. There were no differences between groups with respect to age and parity. The patient characteristics are shown in Table 1. Body mass index (BMI) and history of previous intra-pelvic surgeries were significantly lower in the TLH group than in the TAH group (P = 0.0092, 0.0136, respectively). The intra-operative data and complications are shown in Table 2. Blood loss was significantly lower in the TLH group than in the TAH group (median 0 mL vs. 250 mL; P < 0.0001). Uterine volume was significantly smaller in the TLH group than in the TAH group (median 342 g vs. 788 g; P < 0.0001). Surgical duration was significantly longer in the TLH group than in the TAH group (median 214 minutes vs. 152 minutes; P < 0.0001). In the TLH group, the median surgical duration tended to decrease year by year, 230.3 minutes in 2008 (n = 3), 232 minutes in 2009 (n = 9), 243.6 minutes in 2010 (n = 14), 194.1 minutes in 2011 (n = 11), and 190.8 minutes in 2012 (n = 8). In the TLH group, median uterine volume was 272 g (n = 3) in 2008, 382 g (n = 9) in 2009, 330 g (n = 14) in 2010, 268 g (n = 11) in 2011, and 343 g (n = 8) in 2012. No intraoperative complications occurred in either group. The incidence of postoperative complications was lower in the TLH group than in the TAH group (0/45 vs. 15/134; P = 0.0190). The details of the postoperative complications are shown in Table 3. The hospital stay was significantly shorter for the TLH group than for the TAH group (P < 0.0001). In the TLH group, surgical duration correlated with uterine volume (regression coefficient = 1.6598, P = 0.0014); (Fig. 1). The uterine volume in patients undergoing TLH was estimated to be 272 g, based on the result of linear regression analysis using 152 minutes, which was the median surgical duration in TAH.
 Click to view | Table 1. Patient Characteristics |
 Click to view | Table 2. Intra-Operative Data and Complications |
 Click to view | Table 3. Postoperative Data and Complications |
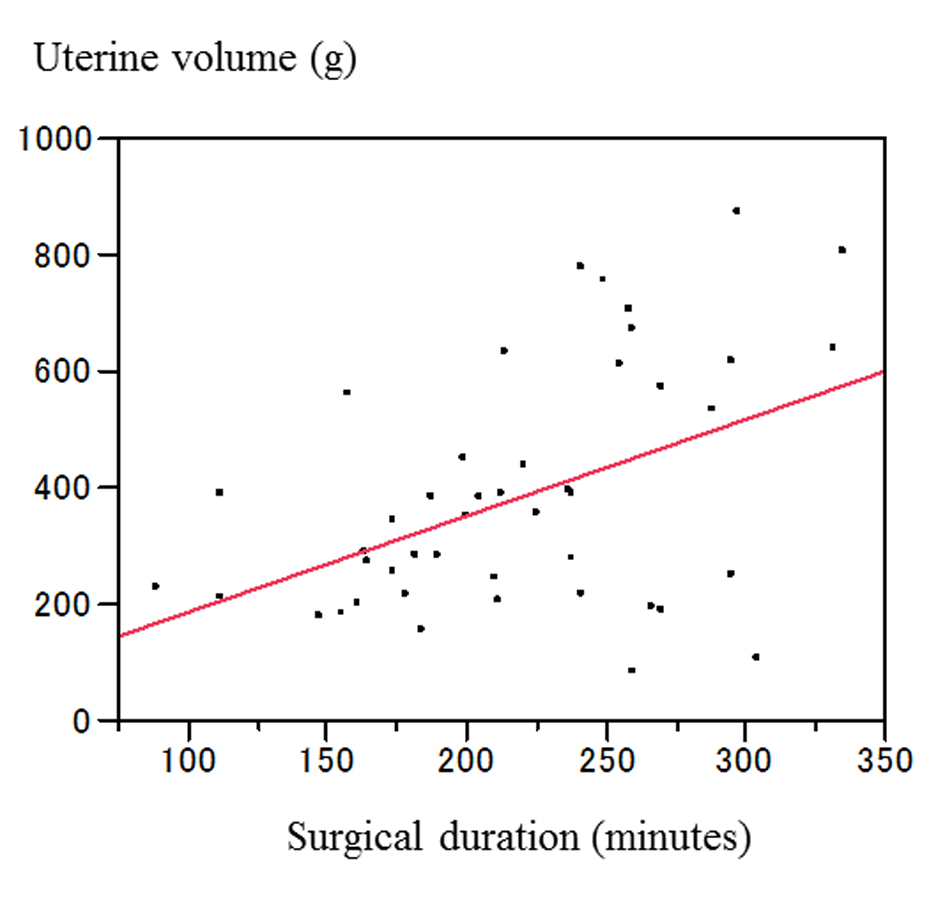 Click for large image | Figure 1. Linear regression between blood loss and uterine volume in TLH. Regression coefficient = 1.6598, P = 0.0014. Uterine volume (g) = 21.454628 + 1.6597504 × surgical duration (minute). |
| Discussion | ▴Top |
The results of meta-analyses indicate that vaginal hysterectomy is the most beneficial procedure for hysterectomy for benign disease [3]. In addition, patients who underwent laparoscopic hysterectomy reported a better quality of life compared with those undergoing abdominal hysterectomy [6]. Therefore, LAVH and TLH are preferable to TAH when a vaginal hysterectomy is not feasible [3]. The benefits were not significantly different between TLH and LAVH [3]. Uterine volume, however, was significantly greater in patients who underwent TLH compared with those who underwent LAVH, consistent with a previous report [7], and less blood loss occurred in TLH vs. LAVH, also consistent with a previous report [3]. Therefore, TLH is preferable to LAVH for resection of large uteri such as those with leiomyomas. Recent results of a meta-analysis indicated that TLH might offer benefits such as less postoperative pain and a shorter hospital stay, compared with vaginal hysterectomy for benign disease [8]. In the present study, BMI and history of previous intra-pelvic operations were significantly lower in the TLH group than in the TAH group. A selection bias might have occurred, though, because the present study was retrospective although patients were selected as described above. Based on the intra-operative data, blood loss was significantly lower in the TLH group than in the TAH group. In contrast, surgical duration was significantly longer in the TLH group than in the TAH group. These results are the same as those in a previous report [3]. Intra-operative complications, however, did not occur in the present study. The postoperative data revealed that hospital stay was significantly shorter for the TLH group than for TAH group, as reported previously [3]. The results of a meta-analysis indicated no significant differences in the occurrence of pelvic hematoma, vaginal cuff infection, or urinary tract infection between TLH and TAH [3]. In contrast, no postoperative complications occurred in the TLH group in the present study. The reason no postoperative complications including vaginal cuff dehiscence and wound complications occurred may be because BMI and history of previous intra-pelvic operation were lower in the TLH group than in the TAH group, and there was a small sample size in the TLH group. Among patients with a BMI of more than 30, complications including hemorrhage and hematoma, requiring blood transfusion, traumatic or burning bowel, and urinary tract injury, were more common than among patients with a BMI of less than 30 [9]. Surgical wounds were wider in TAH than in TLH, making wound disruption more common in TAH than in TLH. TLH was estimated to be, and experienced as, significantly more difficult than TAH [10]. Surgical duration tends to be longer in TLH than in TAH [3]. In the present study, the surgical duration was significantly longer in the TLH group than in the TAH group, and uterine volume was significantly smaller in the TLH group than in the TAH group. Surgical duration was significantly correlated with uterine volume in TLH in the present study. The results of a large-number case-control study indicated that uterine volume and physician experience are independent predictors of surgical duration [11]. In the present study, surgical duration was shorter in 2012 than in 2008. It is expected that surgical duration can be further decreased as physicians acquire experience. An appropriate uterine volume for TLH is estimated to be 272 g when the uterine volume in TLH is calculated using 152 minutes, which was the median surgical duration in TAH in the present study. Surgical duration, however, is more likely related to the morphology of uterus, mobility of the uterus, and the presence of adhesions than to uterine volume. Furthermore, there are other merits of TLH, including less blood loss, fewer complications, and shorter hospital stay compared with TAH, based on both the present study and many previous reports [3]. Therefore, a uterine volume of 868 g, which was maximal in the present study, can be operable by TLH based on the results of the present study. TLH is feasible and safe, resulting in a short hospital stay, minimal blood loss, minimal operating time, and few complications for patients regardless of uterine weight [11]. TLH is considered feasible for selected patients with uteri weighing more than 1,000 g [12]. Some studies, however, have reported a limitation of TLH related to uterine volume as well. A laparoscopic hysterectomy approach is reported to have a cut-off uterine volume of 280 g [5]. In addition, a uterine volume of more than 500 g seems to be risk factor for the occurrence of intra-operative hemorrhage and postoperative complications [13]. When the uterus is too enlarged, working space is limited, and identifying uterine vessels may be difficult or morcellator-related visceral injuries may occur [14]. The limitations of the present study include the small sample size and the fact that it is a retrospective study.
In conclusion, the present study showed that TLH is feasible in patients with uterine leiomyomas with a volume up to 272 g. There seems to be no limitation of uterine volume in TLH, however, because TLH is safer than TAH except for the longer surgical duration. TLH must be safely performed in consideration of factors such as uterine morphology and uterine volume. Moreover, the surgical duration can be decreased by additional surgical experience.
Conflicts of Interest
All the authors declare that there are no conflicts of interest.
| References | ▴Top |
- Schwartz SM, Marshall LM, Baird DD. Epidemiologic contributions to understanding the etiology of uterine leiomyomata. Environ Health Perspect. 2000;108(Suppl 5):821-827.
pubmed - Wright JD, Ananth CV, Lewin SN, Burke WM, Lu YS, Neugut AI, Herzog TJ, et al. Robotically assisted vs laparoscopic hysterectomy among women with benign gynecologic disease. JAMA. 2013;309(7):689-698.
doi pubmed - Nieboer TE, Johnson N, Lethaby A, Tavender E, Curr E, Garry R, van Voorst S, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2009;(3):CD003677.
pubmed - Johnson N, Barlow D, Lethaby A, Tavender E, Curr L, Garry R. Methods of hysterectomy: systematic review and meta-analysis of randomised controlled trials. BMJ. 2005;330(7506):1478.
doi pubmed - Mebes I, Diedrich K, Banz-Jansen C. Total laparoscopic hysterectomy without uterine manipulator at big uterus weight (>280 g). Arch Gynecol Obstet. 2012;286(1):131-134.
doi pubmed - Nieboer TE, Hendriks JC, Bongers MY, Vierhout ME, Kluivers KB. Quality of life after laparoscopic and abdominal hysterectomy: a randomized controlled trial. Obstet Gynecol. 2012;119(1):85-91.
doi pubmed - Hobson DT, Imudia AN, Al-Safi ZA, Shade G, Kruger M, Diamond MP, Awonuga AO. Comparative analysis of different laparoscopic hysterectomy procedures. Arch Gynecol Obstet. 2012;285(5):1353-1361.
doi pubmed - Gendy R, Walsh CA, Walsh SR, Karantanis E. Vaginal hysterectomy versus total laparoscopic hysterectomy for benign disease: a metaanalysis of randomized controlled trials. Am J Obstet Gynecol. 2011;204(5):388 e381-388.
- Morgan-Ortiz F, Soto-Pineda JM, Lopez-Zepeda MA, Peraza-Garay Fde J. Effect of body mass index on clinical outcomes of patients undergoing total laparoscopic hysterectomy. Int J Gynaecol Obstet. 2013;120(1):61-64.
doi pubmed - Nieboer TE, Spaanderman ME, Bongers MY, Vierhout ME, Kluivers KB. Gynaecologists estimate and experience laparoscopic hysterectomy as more difficult compared with abdominal hysterectomy. Gynecol Surg. 2010;7(4):359-363.
doi pubmed - O'Hanlan KA, McCutcheon SP, McCutcheon JG. Laparoscopic hysterectomy: impact of uterine size. J Minim Invasive Gynecol. 2011;18(1):85-91.
doi pubmed - Kondo W, Bourdel N, Marengo F, Botchorishvili R, Pouly JL, Jardon K, Rabischong B, et al. Is laparoscopic hysterectomy feasible for uteri larger than 1000 g? Eur J Obstet Gynecol Reprod Biol. 2011;158(1):76-81.
doi pubmed - Bonilla DJ, Mains L, Whitaker R, Crawford B, Finan M, Magnus M. Uterine weight as a predictor of morbidity after a benign abdominal and total laparoscopic hysterectomy. J Reprod Med. 2007;52(6):490-498.
pubmed - Milad MP, Sokol E. Laparoscopic morcellator-related injuries. J Am Assoc Gynecol Laparosc. 2003;10(3):383-385.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
