| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 1, Number 4-5, October 2012, pages 79-81
A Rare Case of Postmenopausal Bleeding: Choriocarcinoma
Mehmet Siddik Evsena, e, Sak Muhammet Erdala, Soydinc Hatice Endera, Senturk Senemb, Firat Ugurc, Kucukoner Mehmetd
aDicle University, School of Medicine, Department of Obstetrics and Gynecology, Diyarbakir, Turkey
bDicle University, School of Medicine, Department of Radiology, Diyarbakir, Turkey
cDicle University, School of Medicine, Department of Pathology, Diyarbakir, Turkey
dDicle University, School of Medicine, Department of Medical Oncology, Diyarbakir, Turkey
eCorresponding author: Mehmet Siddik Evsen
Manuscript accepted for publication June 7, 2012
Short title: Postmenopausal Choriocarcinoma
doi: https://doi.org/10.4021/jcgo19w
| Abstract | ▴Top |
Choriocarcinoma is an aggressive malignant tumor comprised of sheets of anaplastic cytotrophoblast/syncytiotrophoblast cells. The majority of choriocarcinoma cases are of intra-uterine, gestational origin and generally develops within the first year following pregnancy, consequently it is generally observed within reproductive age groups. A 58-year-old woman was presented to our clinic with vaginal bleeding in the preceding months. The serum B-HCG level was 12414 mIU/mL. A pelvic ultrasound showed a 41 × 37 mm heterogeneous mass on the right anterior fundal wall of the corpus uteri, to which blood flow was increased on colour Doppler examination. Here in study, we present a case of postmenopausal uterine choriocarcinoma. Practitioner must be awareness of choriocarcinoma as a cause of postmenopausal vaginal bleeding.
Keywords: Uterus; Choriocarcinoma; Postmenopausal
| Introduction | ▴Top |
Choriocarcinoma is an aggressive malignant tumor comprised of sheets of anaplastic cytotrophoblast syncytiotrophoblast cells, arising in 1 in 20,000 - 25,000 pregnancies in Western countries [1]. The majority of choriocarcinoma cases are of intra-uterine and gestational origin. Gestational choriocarcinoma usually arises from a prior-molar pregnancy or on occasions, from a non-molar gestation. Vaginal bleeding is the most common symptom of choriocarcinoma [2]. The carcinoma generally develops within the first year following pregnancy and as a consequence, gestational choriocarcinoma is typically observed within reproductive age groups [1, 3]. In the present study, we present a case of uterine choriocarcinoma in a 58-year-old woman whose last pregnancy was 6 years earlier, as a molar gestation.
| Case Report | ▴Top |
A 58-year-old woman was admitted to our clinic with two discrete episodes of vaginal spotting in the preceding months. The patient went through menopause at the age of 55 and did not receive hormonal therapy during this period. All her deliveries were vaginal, uncomplicated, term pregnancies, her last pregnancy being 14 years ago. The patient had a history of molar pregnancy at the age of 52, 3 years prior to the menopause. Following curettage for the molar pregnancy, she reported that she was followed for 1 year and displayed no sign of gestational trophoblastic disease. She was a non-smoker and had received oral anti-diabetic drugs for type 2 diabetes mellitus for 2 years. She was sexually active.
In the physical examination; her general condition was normal with no abnormal findings. On pelvic examination; the vulva and vagina were normal, the cervix was multiparous, the size of uterus was normal and no palpable adnexal mass was evident. A pelvic ultrasound showed the dimensions of her uterus to be 97 × 52 mm with an endometrial thickness of 6 mm and a 41 × 37 mm heterogeneous mass on the right anterior fundal wall of the corpus uteri, to which blood flow was increased on colour Doppler examination. The serum B-HCG level was 12414 mIU/mL. Biochemical and hematological parameters were within normal limits.
Upon pelvic magnetic resonance imaging, sagittal T2-weighted images revealed a heterogeneous hypointense intramural uterine mass with irregular lobulated margins. The mass had minimal indentation on the endometrial cavity. Following contrast administration, heterogeneous peripheral enhancement was observed with T1W images (Fig. 1a, b). Gestational trophoblastic neoplasia thought of as a presumptive diagnosis because of the high values of b-HCG observed. No metastatic disease was found. Total abdominal hysterectomy and bilateral salpingo-oophorectomy were performed. Macroscopically, hemorrhagic areas were observed on cut surfaces of the specimen (Fig. 2a, b). Microscopic examination revealed infiltrative atypical pleomorphic trophoblastic cells within the myometrium. Immunohistochemical analysis showed that the tumor cells were positive for Epitelial Membrane Antigen, and the Ki-67 proliferation index was up to 30%. The pathological diagnosis was choriocarcinoma (Fig. 3a, b).
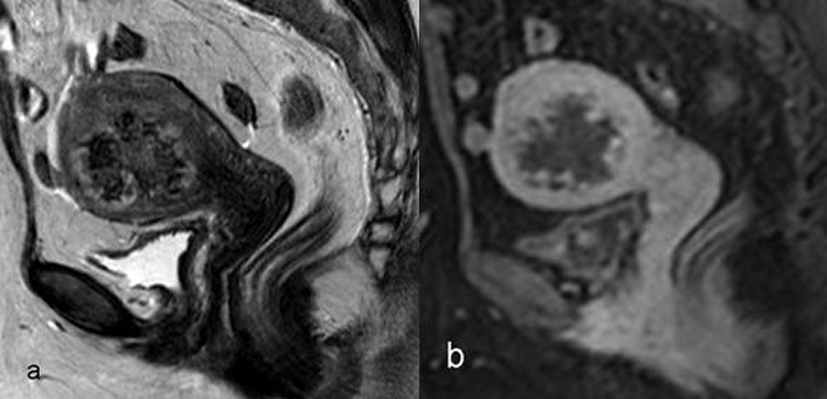 Click for large image | Figure 1. Magnetic resonance images of the uterus. |
 Click for large image | Figure 2. Gross apperance of the uterus. |
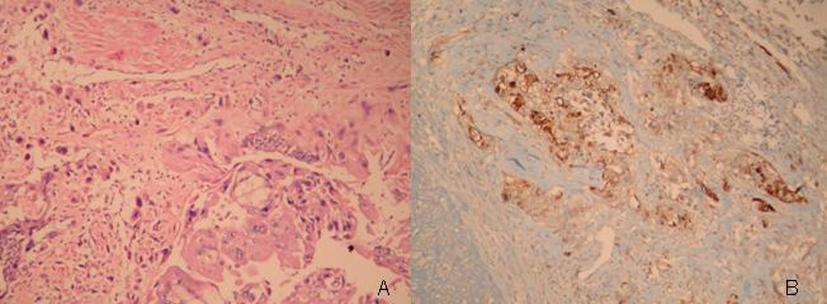 Click for large image | Figure 3. Pathological apperance of the lesion, (a;H&E stain, x100, b; Immunoperoxidase, x100). |
The B-HCG levels fell to 1587 mIU/mL during the first postoperative week. A multi-agent chemotherapy regimen was then initiated. Following the first chemotherapy regimen, the B-HCG levels decreased, to 50 mIU/mL. One week after the second chemotherapy regimen, grade-four hematological toxicity began. The patient died secondary to febrile neutropenia and sepsis.
| Discussion | ▴Top |
This patient had a history of a molar pregnancy while she was 52 years old, experienced her menopause 3 years previously, and developed choricarcinoma at the age of 58 years old. The risk of a hydatidiform mole increased significantly with increasing maternal age. In literature reported that 27% of women aged 50 years and over with trophoblastic disease developed gestational trophoblastic neoplasia. In younger women, the incidence of gestational trophoblastic neoplasia is typically 5% following trophoblastic disease [4].
Choriocarcinoma is generally observed in woman of a reproductive age within a year of an antecedent pregnancy, but can also be observed in postmenopausal woman in rare cases, following a long latent period from previous pregnancies. Desai et al. reported a choriocarcinoma case in a 73-year-old woman developing 38 years after pregnancy and 23 years after her final menstrual period [2, 3].
Choriocarcinoma can be divided in two types: gestational or non-gestational. Gestational choriocarcinoma generally occurs following a molar or non-molar pregnancy in woman of a reproductive age. Non-gestational choriocarcinoma can arise from germ cells or the trophoblastic differentiation of endometrial carcinomas [2]. In our patient, preoperative endometrial sampling resembled decidualization and no evidence of endometrial adenocarcinoma was seen.
The most frequent symptom in uterine choriocarcinoma is abnormal vaginal bleeding. High B-HCG levels and immunohistochemical tests for B-HCG may also be indicative of choriocarcinoma. An early and correct diagnosis of choriocarcinoma is important because it is a chemosensitive tumor with a good prognosis even in advanced stages [5].
Chemotherapy regimens are selected following the identification of high- and low-risk patients. Lurian et al. proposed multi-agent EMACO regimens if a patient displayed high risk factors for the treatment of choriocarcinoma. High risk factors included advanced age, a long interval time from index pregnancy, pre-treatment serum B-HCG levels, a large tumor size, and the presence of metastases [5].
In conclusion, a very rare choriocarcinoma was evident in a postmenopausal woman and should be considered in the differential diagnosis of postmenopausal bleeding. An accurate, early diagnosis and treatment are important because the choriocarcinoma is considered the most curable gynecological cancer. Chemotherapy may occasionally cause fatalities due to treatment-related complications.
| References | ▴Top |
- O'Neill CJ, Houghton F, Clarke J, McCluggage WG. Uterine gestational choriocarcinoma developing after a long latent period in a postmenopausal woman: the value of DNA polymorphism studies. Int J Surg Pathol. 2008;16(2):226-229.
pubmed doi - Desai NR, Gupta S, Said R, Desai P, Dai Q. Choriocarcinoma in a 73-year-old woman: a case report and review of the literature. J Med Case Rep. 2010;4:379.
pubmed - Marcu M, Chefani A, Sajin M. Postmenopausal choriocarcinoma: a case report. Rom J Morphol Embryol. 2005;46(2):145-148.
pubmed - Chittenden B, Ahamed E, Maheshwari A. Choriocarcinoma in a postmenopausal woman. Obstet Gynecol. 2009;114(2 Pt 2):462-465.
pubmed doi - Lurain JR. High-risk metastatic gestational trophoblastic tumors. Current management. J Reprod Med. 1994;39(3):217-222.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
