| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 5, Number 2, June 2016, pages 71-73
Fallopian Tube Papilloma: An Unusual Case of Tubal Obstruction
Ruchi Rathorea, b, Usha Rani Singha, Sonal Sharmaa
aDepartment of Pathology, University College of Medical Sciences, Delhi, India
bCorresponding Author: Ruchi Rathore, Department of Pathology, University College of Medical Sciences, Delhi, India
Manuscript accepted for publication November 25, 2015
Short title: Fallopian Tube Papilloma
doi: http://dx.doi.org/10.14740/jcgo302w
| Abstract | ▴Top |
Fallopian tube (FT) neoplasms either benign or malignant are uncommon in pathology. Papillomas are rare benign neoplasms of the FT. This report describes the presence of a benign papilloma of FT presenting as a ruptured ectopic pregnancy in emergency. A 24-year-old female presented to the gynecology emergency with chief complains of acute pain abdomen for 6 hours and bleeding per vaginum (PV) for 1 day. Left salpingectomy with a right tubal segment ligation was done and sent for histopathologic examination. It was subsequently diagnosed as FT papilloma with no evidence of tubal gestation on histopathology. FT papilloma, although rare and often found incidentally, could be a significant factor in occluding the lumen of the tube, thereby resulting in abortion or sterility of the patient. Since the management is mainly conservative and prognosis is good, it is also essential to differentiate these lesions from the other proliferative lesions of FT.
Keywords: Fallopian tube; Papilloma; Benign; Proliferative; Epithelial
| Introduction | ▴Top |
Fallopian tube (FT) neoplasms either benign or malignant are uncommon in pathology. Papillomas are rare benign neoplasms of the FT [1]. Only very few cases of these tumors have been reported so far. They are mimicked by tubal hyperplasias which are known to occur in response to chronic salpingitis or hormonal stimulation, thereby making it is essential to differentiate between the two [2, 3]. This report describes the presence of a benign papilloma of FT presenting as a ruptured ectopic pregnancy in emergency.
| Case Report | ▴Top |
A 24-year-old gravida 3, para 2, live 2, female presented to the gynecology emergency with chief complains of acute pain abdomen for 6 h and bleeding per vaginum (PV) for 1 day. Her last childbirth was 4 years back and she was not on any contraceptives since then. There was no history of irregular or missed menstrual bleeding, passage of blood clots or dysmenorrhea. On per speculum and PV examination, there was mild bleeding PV, uterus was free and of normal size, right adnexa was unremarkable but a 4 × 4 cm tubo-ovarian mass was felt in the left fornix. Patient’s urine was positive for urine pregnancy test with raised serum beta HCG levels (3,449.10 mIU/mL). Ultrasound abdomen revealed a normal uterus with homogenous endometrium and no gestational sac in the cavity. The left adnexa however showed a mixed echogenic area measuring 5.3 × 3.2 cm suggestive of a left tubo-ovarian mass. Ectopic could not be ruled out. Based on these evidences, a left salpingectomy with a right tubal segment ligation was done. The postoperative course was uneventful, and the patient was sent home 4 days after the operation. Repeat beta HCG levels came down to normal levels on follow-up.
Pathological observations
Left salpingectomy specimen was received in Department of Pathology measuring 5.5 cm in length, which was grossly dilated and edematous but had no areas of congestion or hemorrhage on the external surface. On cut section, there was an irregular pale yellow papillary growth of the mucosa in the infundibular region near the fimbrial end, which almost occluded its lumen. No blood clots, chorionic villi or gestational sac were identified on gross examination. Microscopy showed a complex radiating adenomatous as well as papillary proliferation of the mucosa. These papillae had a complex branching pattern with loose fibrovascular cores and were lined by a single layer of columnar epithelial cells including ciliated and secretory cells (Figs. 1, 2). The nuclei were bland and had no atypia or mitotic activity (Fig. 3). There was no evidence of any significant preexisting salpingitis, on microscopy, the serosa however had serositis with focal area of hemorrhage and fibrinoid necrosis. On processing, the whole tube, in search of chorionic villi, no evidence of a tubal ectopic gestation was found. The right tubal segment sent was unremarkable. Based on the above gross and microscopic features, a diagnosis of left FT papilloma was offered and a possibility of aborted tubal gestation was suggested.
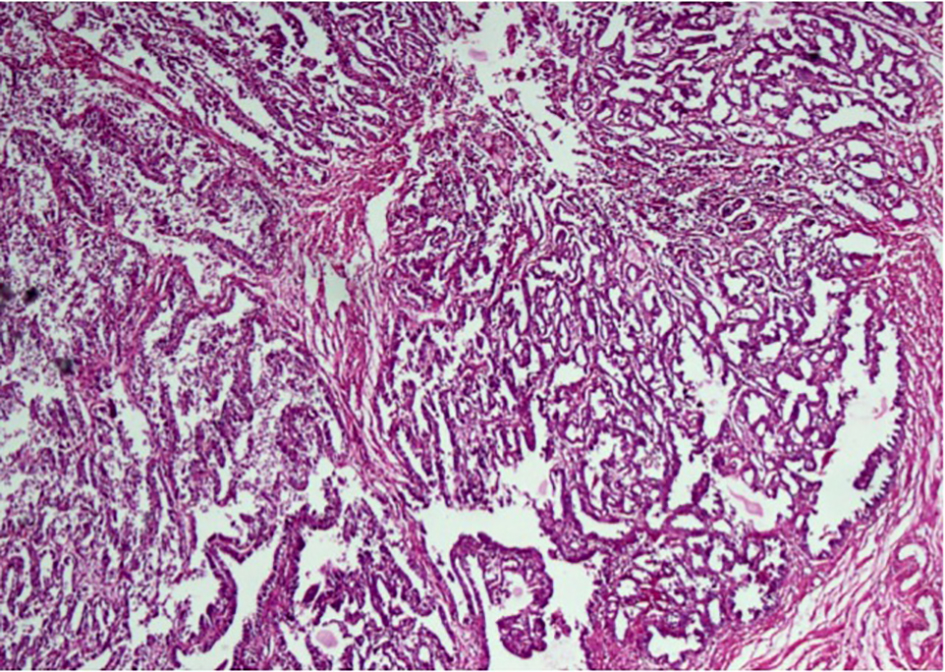 Click for large image | Figure 1. Low power view of a fallopian tube papilloma showing an obliterated lumen due to tumor in the form of papillae and glands (H&E, × 100). |
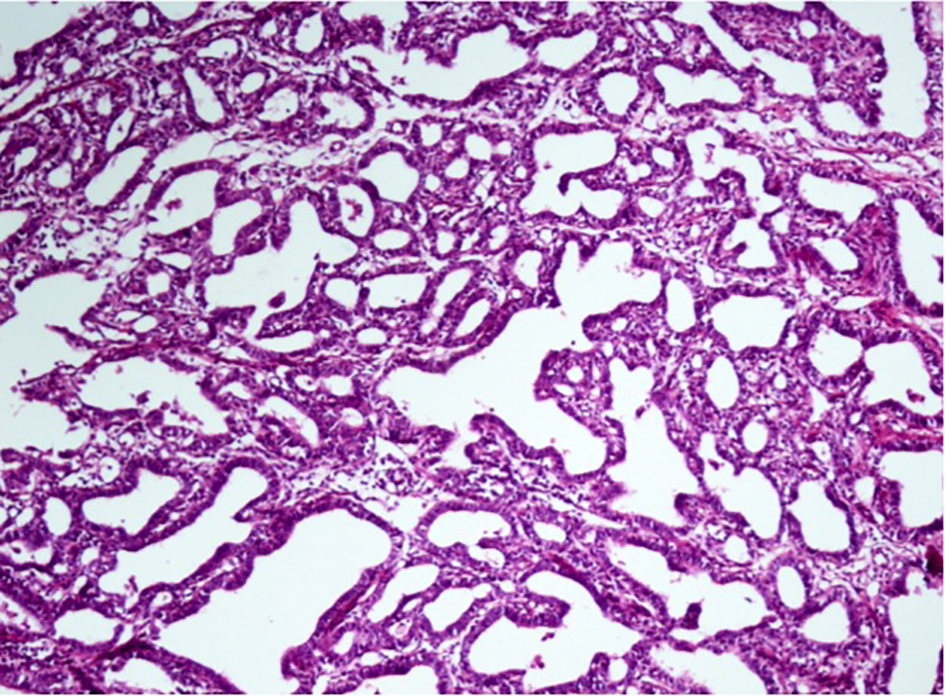 Click for large image | Figure 2. The tumor consisting predominantly of papillae and glands lined by a single layer of cuboidal cells (H&E, × 200). |
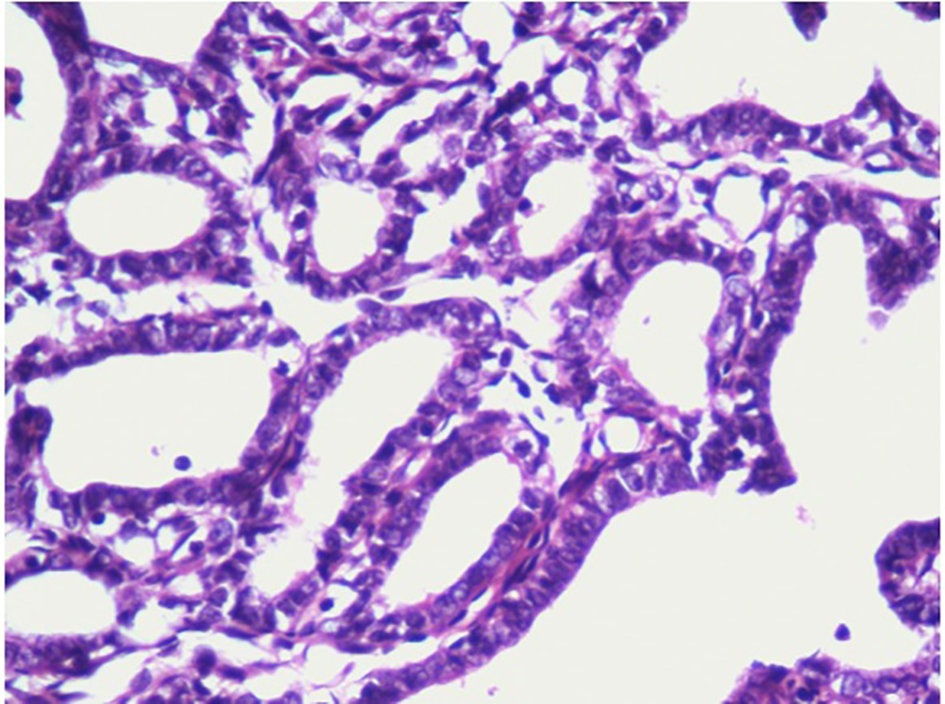 Click for large image | Figure 3. High power view showing glands and ill formed papillae lined by a single layer of columnar epithelial cells with bland nuclei, no atypia and no mitotic activity (H&E, × 400). |
| Discussion | ▴Top |
FT neoplasms both benign and malignant are uncommonly encountered neoplasms in the routinely examined FT specimens. Benign tumors of the tube include polypoid adenofibromas, papilloma, metaplastic papillary tumor and benign serous cystadenoma [2]. FT papillomas are rare tumors of the tube, with only eight cases reported so far in English literature, ours being the ninth such case [1, 3, 4]. These tumors are either discovered incidentally [1] or they may be symptomatic presenting as a mass lesion [3]. In our case, the tumor was incidentally found in a patient who was clinically and sonologically diagnosed as tubal gestation, which might have occurred secondary to tubal obstruction caused by papilloma.
Papillomas are usually found in the infundibular part of FT [3]. The pale yellow growth seen in the infundibulum near the fimbrial end almost blocking the lumen of the tube seen in our case was in accordance with similar lesions described in literature. On microscopy, there were delicate branching papillae arising from the tubal epithelium lined by single layer of columnar to secretory cells with bland nuclei, no atypia or mitosis. Similar to previous studies, our case also had mildly hyperplastic or blunted papillae at the fimbrial end as well as at some distance from the growth [3].
The etiology and pathogenesis of these tubal papillomas still remains unknown. Since the tubal epithelium is responsive to the cyclical hormonal changes, it is hypothesized that an abnormal proliferation of tubal epithelium may occur during such hormonal hyperstimulation or inflammatory conditions, resulting in hyperplasia. However, it is also known that this hyperstimulation causes hyperplasia of almost whole of the tubal epithelium unlike papillomas, which are localized benign neoplasms of the tube as described by Kaspersen et al [2, 5]. Exuberant tubal papillary proliferations are commonly seen in cases of salpingitis and a diagnosis of papilloma should not be rendered when there is significant inflammation or distortion of plicae [6]. The absence of significant inflammation or distortion of plicae, a predominantly localized proliferation, presence of delicate papillae, absence of atypical cell changes and mitosis in our case favors the diagnosis of a papilloma against a reactive hyperplasia associated with salpingitis.
Metaplastic papillary tumor is another benign entity that needs to be considered in the differential diagnosis of an FT papilloma. These rare tumors are typically encountered incidentally in post-partum state and are characterized by broad papillae lined by stratified and tufted epithelium with cells showing abundant eosinophilic cytoplasm and the nuclei not exhibiting any malignant features [7-9]. In our case, although the patient had history and investigations suggestive of tubal abortion, the microscopic absence of broad papillae, stratification, tufting of lining epithelium or moderate eosinophilic cytoplasm of cells, ruled out the diagnosis of metaplastic papillary tumor.
Some studies also describe the frequent association of pseudocarcinomatous lesions of FT with hyperstimulatory conditions like inflammation or hormonal hyperstimulation [10]. In a retrospective study by Rose et al during a period of 23 years, 40 cases were detected to be primary FT cancer and in another 24 cases, tube was involved as a part of multifocal upper genital malignancy. There was transition from in situ to invasive carcinoma in 13 cases [11]. Therefore, it is important to identify a proliferative lesion correctly as in situ carcinoma. Moore and Enterline opine that a papillary or solid lesion, which is mitotically active, could represent pre-invasive carcinoma [10]. Although our case had a proliferative lesion of the tube, but it lacked significant mitosis and nuclear atypia, so a differential diagnosis of a carcinoma in situ was ruled out. As far as the behavior of papillomas is concerned, their malignant potential is still unknown [6].
Kaspersen et al described an FT papilloma which had considerably occluded the lumen of tube thereby was considered a significant factor in patients sterility. We suggest that in our case the presence of FT papilloma might have caused partial occlusion of the lumen, resulting in a tubal abortion into the peritoneal cavity leading to serositis. The very fact that this is the only case where an FT papilloma is the cause of ectopic pregnancy in a young patient with no other associated pathology makes it unique.
In conclusion, FT papillomas, which are incidentally found in the tube, could be a significant factor in occluding the lumen of the tube, thereby resulting in abortion or sterility of the patient. Although rare, it is also important to correctly recognize this entity and distinguish it from various other non-neoplastic epithelial proliferative lesions on one hand and the in situ carcinomas on the other, with its more serious implications. Management of the papilloma can be conservative even when symptomatic.
Conflicts of Interest
None.
Financial Support
No financial support of any form has been taken from any agency for this study.
Author Contributions
All authors have contributed in work and drafting of the manuscript.
| References | ▴Top |
- Narasimhaiah A, Ansari M, Haritwal A, Awasthi S. Fallopian tube papilloma - case report of a rare tumor. Kathmandu Univ Med J (KUMJ). 2013;11(43):250-252.
- Kaspersen P, Buhl L, Moller BR. Fallopian tube papilloma in a patient with primary sterility. Acta Obstet Gynecol Scand. 1988;67(1):93-94.
doi pubmed - Gisser SD. Obstructing fallopian tube papilloma. Int J Gynecol Pathol. 1986;5(2):179-182.
doi pubmed - Ries E. Primary Papilloma and Primary Carcinoma of the Fallopian Tube. JAMA. 1987;XXVIII(21):962-968.
doi - Mostufi-Zahdeh M, Scully RE. Pseudocarcinomaous lesions of the fallopian tube. Lab Invest. 1983;48:61A.
- Wheeler JE. Diseases of the Fallopian tube. In: Kurman RJ, ed, Blaustein's Pathology of the Female Genital Tract. 5th ed. India: Springer-Verlag; 2002;617-648.
- Bartnik J, Powell WS, Moriber-Katz S, Amenta PS. Metaplastic papillary tumor of the fallopian tube. Case report, immunohistochemical features, and review of the literature. Arch Pathol Lab Med. 1989;113(5):545-547.
pubmed - Young RH, Clement PB, Scully RE. The Fallopian Tube and Broad Ligament. In: Mills SE, ed. Sternberg's Diagnostic Surgical Pathology. 4th ed. India: Jaypee Brothers Medical Publisher Ltd; 2004. p. 2653-2675.
- Fallopian Tube (including broad and round ligament). In: Juan Rosai, ed. Rosai Ackerman's Surgical Pathology. 9th ed. India: Elsevier; 2004. p. 1636-1648.
- Moore SW, Enterline HT. Significance of proliferative epithelial lesions of the uterine tube. Obstet Gynecol. 1975;45(4):385-390.
pubmed - Rose PG, Piver MS, Tsukada Y. Fallopian tube cancer. The Roswell Park experience. Cancer. 1990;66(12):2661-2667.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
