| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Original Article
Volume 4, Number 2, June 2015, pages 209-211
Emergency Department Use by Postpartum Patients: Implications for an Accountable Care Organization
Debra Gussmana, b, Jonathan D. Bauma, Andrew Blechmana
aDepartment of Obstetrics and Gynecology, Jersey Shore University Medical Center, 1945 Corlies Ave., Neptune, NJ 07754, USA
bCorresponding Author: Debra Gussman, Department of Obstetrics and Gynecology, Jersey Shore University Medical Center, 1945 Corlies Ave., Neptune, NJ 07754, USA
Manuscript accepted for publication May 01, 2015
Short title: ED Use by Postpartum Patients
doi: http://dx.doi.org/10.14740/jcgo312w
| Abstract | ▴Top |
Background: As part of Accountable Care Organization (ACO) planning, we tracked our obstetrical population to see how they utilize services and access care. One area of scrutiny was emergency department (ED) use after delivery.
Methods: Patients who delivered at Jersey Shore University Medical Center (JSUMC) were identified. Health Information Systems searched the database for ED visits within 6 weeks of the delivery date. Of those who appeared in the ED, data was collected about mode of delivery, reason for ED visit, and the number of days postpartum.
Results: Within the study period, there were 2,022 women who delivered and 154 (7.6%) presented to the ED during their postpartum course for a total of 187 ED visits. There were 1,285 vaginal deliveries (63.6%) and 737 (36.4%) cesarean deliveries. Of the 154 patients who presented to the ED, 100 (64.9%) women were delivered via cesarean and 54 (35.1%) had vaginal deliveries. Obstetrical complications accounted for 137 (73%) of the ED visits. Complications unrelated to pregnancy accounted for 50 (27%) of the ED visits. Eighty-three visits (44%) occurred during the first week postpartum.
Conclusions: Postpartum ED utilization rates may be used as a measure of both efficiency and safety of obstetrical practice. Participating obstetricians in the ACOs should design the clinical standards and quality measures to optimize care of pregnant patients so that safe vaginal delivery is promoted. Physicians who can safely lower their cesarean delivery rates, have low ED utilization, and low readmission rates should be rewarded and retained.
Keywords: Postpartum; Emergency department; Accountable Care Organization
| Introduction | ▴Top |
As part of Accountable Care Organization (ACO) planning, we tracked our obstetrical population to see how they utilize services and access care. One area of scrutiny was emergency department (ED) use after delivery.
Niska et al [1] reported that there were 117 million ED visits in the United States in 2007. For women between 15 and 64, abdominal pain and obstetrical complications were the leading primary diagnoses. There were 1.8 million visits for complications of pregnancy and the postpartum period. Valdya [2] reported that the average cost for an ED visit in 2010 was over $1,000 which translates into almost two billion dollars. Madlon-Kay and DeFor [3] said that childbirth is the most frequent reason for admission to a hospital. They followed 23,000 patients, of whom 3% had urgent care or ED visits within 2 months of discharge. In their population, ED visits were more likely after caesarean delivery. Clark et al [4] established that 5% of women who deliver will be seen in the ED prior to their 6-week routine postpartum visit. Therefore, in our suburban hospital which performs 2,000 deliveries, we expected 60 - 100 ED visits by postpartum patients. Internal audit showed our ED rates to be 7% which was higher than predicted. The purpose of this paper was to examine ED use by our postpartum patients and to make recommendations to the ACO.
| Methods | ▴Top |
Institutional review board approval (IRB) was obtained. All patients who delivered at Jersey Shore University Medical Center (JSUMC) from July 1, 2010 to June 30, 2011 were identified. Health Information Systems searched the database for ED visits within 6 weeks of the delivery date. Of those who appeared in the ED, data was collected about mode of delivery, reason for ED visit, and the number of days postpartum.
| Results | ▴Top |
There were 2,022 women who delivered and 154 (7.6%) presented to the ED during their postpartum course for a total of 187 ED visits. There were 1,285 vaginal deliveries (63.6%) and 737 (36.4%) cesarean deliveries. Of the 154 patients who presented to the ED, 100 (64.9%) women were delivered via cesarean and 54 (35.1%) had vaginal deliveries.
Obstetrical complications accounted for 137 (73%) of the ED visits (Table 1). Complications unrelated to pregnancy accounted for 50 (27%) of the ED visits. Eighty-three visits (44%) occurred during the first week postpartum. Figure 1 shows the distribution of visits.
 Click to view | Table 1. Obstetrical Complications |
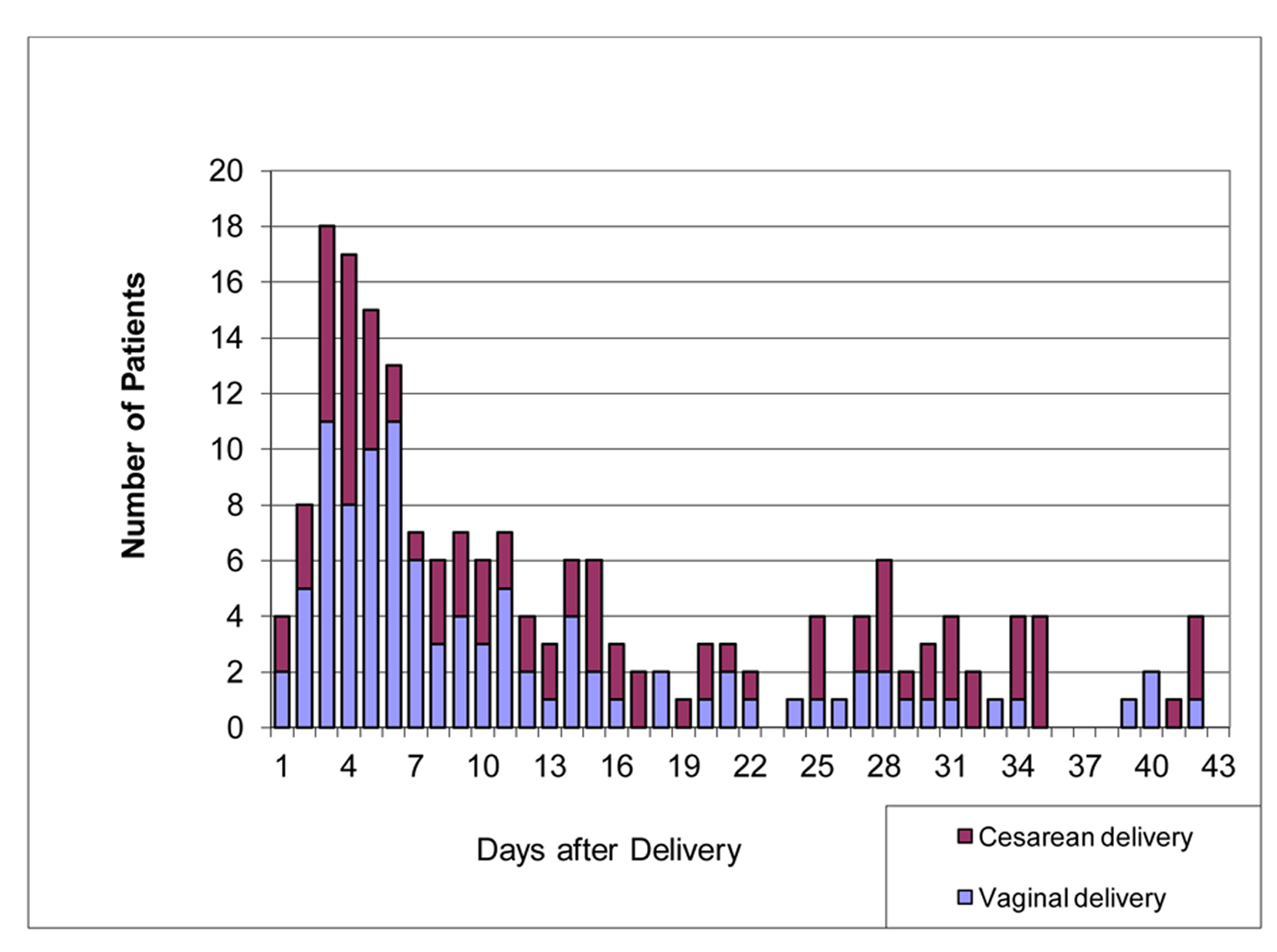 Click for large image | Figure 1. Distribution of ED visits. |
| Discussion | ▴Top |
The goal of the ACO is coordinated care that ensures that patients get the right care at the right time efficiently and safely. To date, most of the ACO focus is on the Medicare patient with chronic disease. The challenge is to improve care and decrease the collective spending. We believe that the same analysis should be applied to obstetrical services.
Postpartum ED utilization rates may be used as a measure of both efficiency and safety of obstetrical practice. At our institution, the majority of the patients who presented to the ED had a cesarean delivery. Our population was similar to those described by Clark et al [4]. The majority of diagnoses were wound complication and urinary tract infection. Wound complications rarely occur in vaginal deliveries. As cesarean delivery rates climb so does ED utilization. Clark et al [4] reported a cesarean delivery rate of 36% was associated with an ED utilization rate of 6.2%. Madlon-Kay and DeFor [3] reported a cesarean delivery rate of 15% was associated with an ED utilization rate of 3%. Lower cesarean delivery rates result in lower ED use postpartum.
Obstetricians should strive to have the lowest possible, safest rate of cesarean delivery. A cesarean delivery rate of 0% is neither safe nor feasible. The American College of Obstetricians and Gynecologists (ACOG) offers evidence-based guidelines to safely achieve a lower cesarean delivery rate [5].
Obstetricians partnering with health coaches and health navigators should be able to direct patients to the highest efficiency safest care alternative. Patients need appropriate care in safe and familiar surroundings rather than reflexively going to the ED. There may be a role for post-cesarean delivery counselors or patient health coaches to address patient concerns in order to avoid unnecessary ED visits. ACO practices should be encouraged to provide extended hours of care and make provision for walk-in patients.
Participating obstetricians in the ACOs should design the clinical standards and quality measures to optimize care of pregnant patients so that safe vaginal delivery is promoted. Physicians who can safely lower their cesarean delivery rates have low ED utilization, and low readmission rates should be rewarded with higher reimbursement.
| References | ▴Top |
- Niska R, Bhuiya F, Xu J. National hospital ambulatory Medical care survery: 2007 emergency department summary. National health statistics reports; no 26. Hyattsville, MD: National Center for Health Statistics; 2010.
- Valdya A. 8 Statistics on the average cost per ED visit. 2013. ASC Communications retrieved on July 16, 2014 from http://www.beackerhospitalreview.com/finance/8-statistics-on-the-average-cost-per-ed-visit.html.
- Madlon-Kay DJ, DeFor TA. Maternal postpartum health care utilization and the effect of Minnesota early discharge legislation. J Am Board Fam Pract. 2005;18(4):307-311.
doi pubmed - Clark SL, Belfort MA, Dildy GA, Englebright J, Meints L, Meyers JA, Frye DK, et al. Emergency department use during the postpartum period: implications for current management of the puerperium. Am J Obstet Gynecol. 2010;203(1):38 e31-36.
- Safe prevention of primary cesarean delivery. American College of Obstetricians and Gynecologists. Society for Maternal-fetal Medicine. Obstetric Care Consensus 2014. No. 1.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
