| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 1, Number 4-5, October 2012, pages 76-78
Cavernous Sinus-Orbital Vein Thrombosis due to Infection and Thrombophilia
Ali Jaffrya, David Ermakb, Aiesha Ahmedb, c
aDepartment of Obstetrics & Gynecology, Penn State College of Medicine, 500 University Drive, Hershey, PA 17033, USA
bDepartment of Neurology, Hershey Medical Center, Penn State College of Medicine, EC037, 30 Hope Drive, Hershey, PA 17033, USA
cCorresponding author: Aiesha Ahmed
Manuscript accepted for publication June 8, 2012
Short title: Cavernous Sinus-Orbital Vein Thrombosis
doi: https://doi.org/10.4021/jcgo33w
| Abstract | ▴Top |
We present a patient with cavernous sinus-orbital vein thrombosis while highlighting the causes, risk factors and diagnostic modalities. The onset was acute while she was in labor. She was off of anticoagulation, had history of deep vein thrombosis and recent sinus infection which were thought to be the etiological factors.
Keywords: Thrombosis; Pregnancy; Ptosis.
| Introduction | ▴Top |
The cavernous sinuses and their connections are devoid of valves, consequently bidirectional spread of infection and thrombi can occur throughout this network. Cavernous sinus thrombosis can be septic or aseptic. Etiology determines treatment with antibiotic or anticoagulants.
| Case Report | ▴Top |
A 19-year-old female at 41 weeks of gestation presented to Labor and Delivery ward in labor. While in the hospital, she developed left jaw pain associated with toothache. This was followed by inability to open her left eye along with swelling of the left side of the face and eye. She also started complaining of tingling sensation over the left side of her face. Within the next 2 hours, she complained of pain with left eye movements and sensitivity to light. She also noticed blurry vision out of the left eye. She had been complaining of stuffy nose a day prior to the onset of the above symptoms. Her past medical history was significant for left lower extremity DVT diagnosed during her 11th week of gestation. She was started on low-molecular weight heparin therapy with enoxaparin up until 36th week of pregnancy when she was switched to subcutaneous heparin in preparation for her delivery. Her last dose of subcutaneous heparin was 12 hours prior to the onset of above complains. Her medications in addition to the anticoagulants mentioned above included iron supplements. Her family history revealed that her mother carried the diagnosis of Factor V Leiden deficiency and had been on indefinite Coumadin therapy. She was unaware of details that prompted the diagnosis for her mother. Her social history was remarkable for smoking 1/2 pack per day in the past which she quit 6 month ago. Her exam showed blood pressure of 131/60, pulse of 114 and temperature of 36.5 °C. She was awake and alert. Her speech was normal. Left conjunctival injection was noted. There was left-sided ptosis with an inability to open the eye with periorbital edema. Her visual fields were full. The pupils were equal and reactive. Her extraocular movements were normal in the right eye. However, she had difficulty with abduction of the left eye. Facial sensation was decreased in the V2 and V3 distributions on the left. Rest of the cranial nerve and sensory exam were normal. Motor examination showed normal tone and full strength throughout. Reflexes were 2+ throughout. Babinski sign was mute. No dysmetria was noted. Labwork showed normal complete metabolic panel and CBC except for WBC of 15.36. Her PTT was 29 and INR was 0.99. MRI brain showed inflammatory changes in the left orbit, ethmoid and maxillary sinus mucosa, representing sinusitis/orbital cellulitis with superior ophthalmic vein thrombosis and early cavernous sinus thrombosis. She had unremarkable intracranial MRA (Fig. 1). No evidence of dural venous thrombosis was noted on MRV. She was empirically started on vancomycin, cefepime and metronidazole. She was delivered via C-section due to failed induction and was started on anticoagulation (heparin drip) 6 hours after the C-section. Her symptoms improved significantly within 12 hours of starting the anticoagulation.
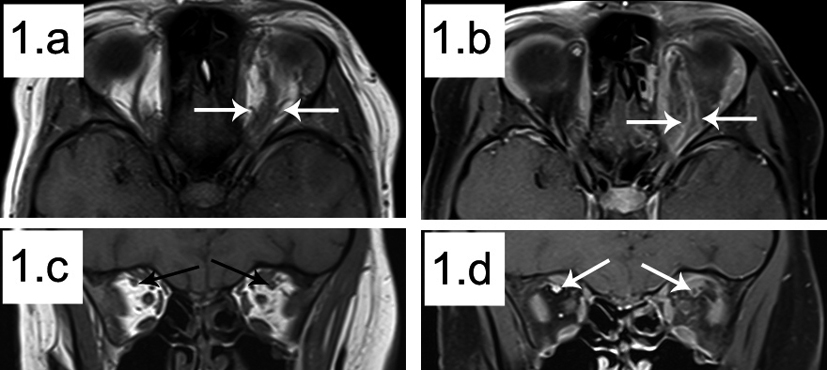 Click for large image | Figure 1. Coronal and Axial MRI images. a: Axial T1 showing irregularity and dilation of the left superior ophthalmic vein compared to the right (outlined by white arrows); b: Axial T1 fat sat post contrast showing thrombus in situ in the left superior ophthalmic vein (outlined by white arrows); c: Coronal T1 showing an enlarged left superior ophthalmic vein compared to the right (white arrows); d: Coronal T1 fat sat post contrast showing thrombus in situ in the left superior ophthalmic vein compared to normal contrast flow on the right (white arrows). |
| Discussion | ▴Top |
The cavernous sinuses are dural venous sinuses. The oculomotor nerve, trochlear nerve, ophthalmic and maxillary divisions of the trigeminal nerves lie within its lateral wall, and the abducent nerve and the internal carotid artery lie within its lumen.
Septic cavernous sinus thrombosis (CST) describes a thrombophlebitic process affecting the cavernous sinus that has an infective etiology. This condition is usually caused by facial infections, paranasal sinusitis, otogenic, odontogenic, pharyngeal and distant sources of sepsis. Once septic CST develops, emphasis rests on the prompt institution of parental antibiotics as well as surgery for concurrent closed-space infections. Anticoagulation can be used safely as an adjunct to antibiotic [1].
The aseptic cases of CST can be seen in debilitated patients (marasmic phlebothrombosis) at the extremes of age, with the etiologic factors being anemia, hypercoagulability, dehydration, hypotension allowing stagnation of blood, carotid aneurysms, surgical treatment of trigeminal neuralgia. Also, aseptic thrombosis of the posterior part of the ophthalmic vein and of the cavernous sinus has been described secondary to compression or obstruction by malignant tumors of the skull base or nasopharynx. The increase in incidence of thromboembolism is also supported by studies that have shown that patients taking estrogens or combined oral contraceptives have increased platelet aggregation, accelerated blood clotting, altered blood concentrations of some clotting factors, and altered fibrinolytic activity related to decrease in antithrombin III. Pregnancy, puerperium, and oral contraceptive pill have prominent associations with dural sinus thrombosis [2].
The incidence of cerebrovascular diseases during pregnancy or puerperium is 11%. Cerebrovascular diseases are more frequent in puerperium than during pregnancy, being 1.8:1. The most common causes are coagulation disorders, cardio embolism and eclampsia, whereas etiology remains undetermined in 35% of the cases [3].The inherited thrombophilias are the leading cause of maternal thromboembolism and are associated with an increased risk of certain adverse pregnancy outcomes including second- and third-trimester fetal loss. All patients with a history of prior venous thrombotic events and those with these characteristic adverse pregnancy events should be evaluated for thrombophilias. The most common, clinically significant, inherited thrombophilias are heterozygosity for the factor V Leiden and prothrombin G20210A mutations [4].
Conflict of Interests
The authors have no conflict of interest and observed ethical adherence.
Grant Support and Financial Disclosure
None.
| References | ▴Top |
- Bhatia K, Jones NS. Septic cavernous sinus thrombosis secondary to sinusitis: are anticoagulants indicated? A review of the literature. J Laryngol Otol. 2002;116(9):667-676.
pubmed doi - Lai PF, Cusimano MD. The spectrum of cavernous sinus and orbital venous thrombosis: a case and a review. Skull Base Surg. 1996;6(1):53-59.
pubmed doi - Pervulov M, Gojnic M, Jovanovic D. Cerebrovascular diseases during pregnancy and puerperium. J Matern Fetal Neonatal Med. 2009;22(1):51-58.
pubmed doi - Lockwood CJ. Inherited thrombophilias in pregnant patients: detection and treatment paradigm. Obstet Gynecol. 2002;99(2):333-341.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
