| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 4, Number 2, June 2015, pages 232-234
Subtle Presentation of Bilateral Ovarian Dermoid Cysts With Unilateral Torsion: A Case Report
Ankita Ramana, c, Geeta Sinhaa, Anjana Sinhaa, Suraj Pratapb
aDepartment of Obstetrics & Gynaecology, Patna Medical College & Hospital, India
bDepartment of Pediatrics, Mahavir Cancer Institute, Patna, India
cCorresponding Author: Ankita Raman, Patna Medical College and Hospital (PMCH), Ashok Rajpath, Patna, Bihar 800004, India
Manuscript accepted for publication June 11, 2015
Short title: Bilateral Ovarian Dermoid Cysts
doi: http://dx.doi.org/10.14740/jcgo334w
| Abstract | ▴Top |
Majority of non-physiological tumors seen in pregnancy are mature cystic teratomas, also known as dermoid cysts. Their discovery in pregnant women poses a vexing problem as there are no established guidelines for their management and multiple factors need to be considered to decide the appropriate strategy. We are reporting a case of bilateral ovarian dermoid cysts in a pregnant woman who presented towards the end of her third trimester and was managed by careful observation until the day of elective cesarean section and bilateral cystectomy. During surgery the team was surprised to discover a torsed dermoid cyst. The striking features of this case were the subtlety of clinical presentation and the absence of typical signs associated with ovarian torsion.
Keywords: Dermoid cyst; Teratoma; Torsion
| Introduction | ▴Top |
Ovarian masses are among the known complications encountered during pregnancy. It is estimated that 1 in every 1,000 pregnant women undergoes surgical exploration for an adnexal mass. Most of the ovarian masses discovered in pregnancy are either functional cysts or benign cysts. The commonly encountered corpora lutea are often diagnosed accidentally on physical or routine ultrasound examinations. They are rarely more than 5 cm in diameter, generally unilocular and almost always unilateral. Although malignant ovarian neoplasms are the fourth most common cause of death from cancer in women, their incidence in pregnant women is much lower. About 5% of the adnexal masses diagnosed in pregnancy are malignant compared with 15-20% in the non-pregnant population [1]. This is likely due to the younger age of pregnant women. Benign cystadenomas and mature cystic teratomas (dermoids) constitute the majority of ovarian tumors diagnosed in pregnancy. Dermoid cysts account for up to 40% of ovarian tumors and their association with pregnancy has been increasingly reported in the past few decades [2].
Here we present the case of a primi-gravida patient from India who presented in her third trimester with mild abdominal pain. Her medical records showed that she was diagnosed with a left ovarian cyst about 2 years ago and she had decided not to undergo any surgical intervention despite gynecologist’s recommendations. The Obstetric team at Patna Medical College & Hospital admitted the patient for further imaging and decided to follow her conservatively until the time of delivery.
| Case Report | ▴Top |
A 27-year-old female belonging to the middle socio-economic class presented with mild abdominal pain in the 34th week of pregnancy. She described her pain as intermittent, dull, aching in nature, 4-5/10 in intensity, poorly localized to lower abdomen which was aggravated by exertion. No nausea, vomiting and fever were reported. She denied dysuria, dyspareunia, constipation or diarrhea. About 2 years ago she was diagnosed with a small sized simple cyst of the left adnexa. The gynecologist had recommended a laparoscopy assisted cystectomy which the patient refused due to her reservations with surgical procedures. She was therefore managed conservatively using hormonal contraceptive pills and serial ultrasound studies were done to monitor the evolution of cyst. She reported that one of the ultrasound studies had suggested that there was a mild reduction in the size of the cyst initially. However the most recent imaging, an MRI done 6 months ago, had shown a complex left ovarian cyst measuring 8.5 × 9.7 × 10.7 cm, presumably a dermoid, a small complex right ovarian cyst and a gravid uterus.
Since the patient presented to us with an advanced pregnancy we decided to admit her and monitor for signs of ovarian torsion, cyst rupture, fetal distress and other potential complications until the time of delivery. After weighing the benefits of delaying delivery till term with the risks of ovarian torsion and fetal distress a cesarean section was planned in the 38th week of pregnancy. Her hospital stay was uneventful and the results of her serial physical and ultrasound examinations were consistently reassuring. The delivery of a healthy male baby was followed by left sided oophorectomy and right sided cystectomy. During surgery it was discovered that the left ovarian dermoid was torsed by one full turn and was slightly dusky in appearance (Fig. 1). The left dermoid was approximately 12 cm in largest dimension while the right ovary had a smaller dermoid cyst (measuring 3.8 cm in largest dimension) and some normal ovarian tissue which was preserved.
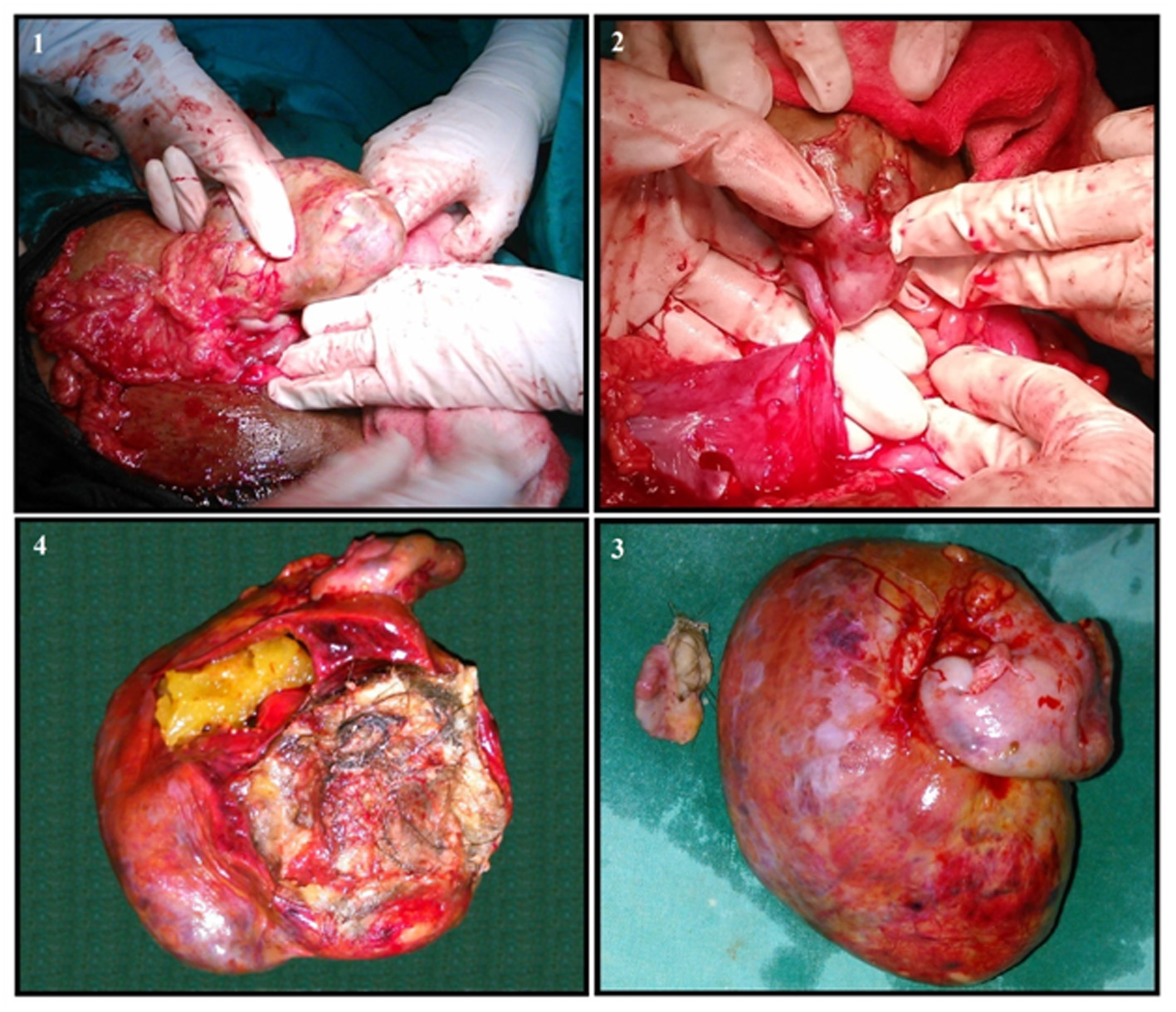 Click for large image | Figure 1. (1) Left ovarian dermoid cyst seen during surgery. (2) Torsion is better visible in this view after clearing the overlying tissues. (3) Both dermoids kept side by side for comparison. (4) Dissected left ovarian dermoid. |
| Discussion | ▴Top |
Mature cystic teratomas (dermoids) are believed to originate from the primordial germ cells and are commonly detected in the second and third decades of life in women. The most common complication of a mature cystic teratoma is ovarian torsion. Factors that are believed to increase the risk of torsion include moderate weight and high fat content of the cyst. The pain associated with torsion is usually localized and, depending on the degree of vascular occlusion, can be very severe. The discovery of a dermoid cyst in pregnancy poses a vexing problem for the obstetrician who has to balance the risks of surgery and the risks of a persistent adnexal mass. There is no agreement about the best management of an adnexal mass in pregnant women. Characteristic features that favor a wait-watch approach include small size (< 5 cm), simple in nature (based on ultrasound studies) and early diagnosis (< 16 weeks gestation) [3, 4]. Some references suggest that ovarian dermoid cysts less than 6 cm are not expected to grow or cause complications during pregnancy and hence can be managed conservatively [5].
Similarly there seems to be a consensus that larger cysts (> 10 cm) are prone to complications and should be surgically removed if diagnosed early in the pregnancy. One group recommended that all cysts larger than 8 cm should be removed, as should smaller cysts that are multilocular, thick walled or semi-solid [6]. Dermoids with sizes 6 - 10 cm and/or which are diagnosed later in the pregnancy continue to be a surgical dilemma. Some authors recommend elective removal of any adenexal mass larger than 6 cm that persists beyond 16 weeks gestation, due to the increased risk of surgical emergencies [7]. Another study found that patients who underwent laparotomy after 23rd week had a significantly higher incidence of adverse pregnancy outcomes when compared to those who were operated early in pregnancy [1].
This patient presented quite late in her pregnancy and the team felt that watchful monitoring in the hospital until delivery would be the most appropriate approach. Since she never complained of any worsening of pain and her physical examinations showed no acute changes, it is difficult to establish exactly when the torsion of her left dermoid cyst occurred. Fortunately the cyst was excised before it became necrotic or secondarily infected, which would have complicated the pregnancy further. This case emphasizes the importance of being highly vigilant with pregnant patients having moderate to large size dermoid cysts as complications like torsion can develop even without overt symptoms. To sum up we would like to reiterate that there are no established guidelines for management of moderate to large sized ovarian cysts that are diagnosed late in the pregnancy and hence the approach should be individualized based on severity of symptoms, fetal well being, patients’ understanding of the risks and the accessibility of medical care in case of an emergency.
Acknowledgement
We would like to thank Dr. Arti Kumari, Dr. Wasima Arshi and Dr. Vinita Kumari for their valuable inputs as well as the nurses and residents working in the Obstetric Ward of our hospital.
| References | ▴Top |
- Whitecar MP, Turner S, Higby MK. Adnexal masses in pregnancy: a review of 130 cases undergoing surgical management. Am J Obstet Gynecol. 1999;181(1):19-24.
doi - Koonings PP, Campbell K, Mishell DR, Jr., Grimes DA. Relative frequency of primary ovarian neoplasms: a 10-year review. Obstet Gynecol. 1989;74(6):921-926.
pubmed - Mazze RI, Kallen B. Reproductive outcome after anesthesia and operation during pregnancy: a registry study of 5405 cases. Am J Obstet Gynecol. 1989;161(5):1178-1185.
doi - Whiteside JL, Keup HL. Laparoscopic management of the ovarian mass: a practical approach. Clin Obstet Gynecol. 2009;52(3):327-334.
doi pubmed - Caspi B, Levi R, Appelman Z, Rabinerson D, Goldman G, Hagay Z. Conservative management of ovarian cystic teratoma during pregnancy and labor. Am J Obstet Gynecol. 2000;182(3):503-505.
doi pubmed - Hogston P, Lilford RJ. Ultrasound study of ovarian cysts in pregnancy: prevalence and significance. Br J Obstet Gynaecol. 1986;93(6):625-628.
doi pubmed - Hamilton CA, Harris J, Ellison M. Cystic teratoma. Emedicine (http://www.emedicine.com/med/topic2248.htm). 2006.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
