| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Original Article
Volume 4, Number 3, September 2015, pages 265-270
Medical Treatment of Spontaneous Abortion in the First Trimester
Estefania Ruiperez Pachecoa, b, Miriam de la Puente Yaguea, Nuria Izquierdo Mendeza, Eloy Asenjo de la Fuentea, Miguel Angel Herraiz Martinez y Jose Antonio Vidart Aragona
aDepartment of Obstetrics and Gynecology, Hospital Clinico San Carlos, School of Medicine, Complutense University of Madrid, Madrid, Spain
bCorresponding Author: Estefania Ruiperez Pacheco, St/Santiago de Compostela, Nº: 92, 5ºC, Madrid 28035, Spain
Manuscript accepted for publication June 11, 2015
Short title: Medical Treatment of Spontaneous Abortion
doi: http://dx.doi.org/10.14740/jcgo335w
| Abstract | ▴Top |
Background: The objective was to evaluate the efficacy of medical treatment with misoprostol in spontaneous abortion in the first trimester. The other objectives were to determine the incidence of side effects and complications and identify causes that may motivate medical treatment failure, and to establish the degree of acceptance and patient satisfaction. A cost-effectiveness study was performed.
Methods: It was longitudinal, observational, prospective, descriptive and analytic research. We evaluated 680 patients diagnosed with spontaneous abortion of the first trimester, in the period between June 2009 and December 2011 at the Hospital Clinico San Carlos. It was developed a protocol for the administration of medical treatment with misoprostol for those patients who accepted, compared with classic surgery.
Results: The success of medical treatment was 81.85%, it was effective in 89.21% of accomplished incomplete abortion, in the 79.52% of deferred abortion and in the 78.46% of anembryonic gestation. There were minor side effects in the 33.59% of patients, declaring satisfaction in 84.99% of patients. With regard to cost study, there was a patient savings €960.54.
Conclusions: The success of medical treatment in our study was high, with effective approximately eight out of 10 patients. Misoprostol is highly accepted by patients, declaring most satisfied. The incidence of minor side effects is low, and were well tolerated, so their presence does not seem to restrict the application of such treatment. Its use helps to reduce healthcare costs.
Keywords: Spontaneous abortion; Medical treatment; Curettage
| Introduction | ▴Top |
Since the 19th century classic treatment is surgical abortion or also called curettage evacuator. It is not the only possible treatment, since drugs can also be used to evacuate the uterine cavity, what is known as a medical treatment.
Objectives
The main objective of our study was to evaluate the efficacy of medical treatment with misoprostol in spontaneous abortion in the first trimester of pregnancy (deferred abortion, accomplished incomplete abortion and anembryonic gestation).
Secondary objectives of the work were to establish the degree of acceptability and satisfaction of patients, to determine the incidence of side effects and complications of such treatment, to identify the causes that can produce the failure of treatment with misoprostol and perform a cost/efficacy study of medical treatment.
| Materials and Methods | ▴Top |
The study is longitudinal, observational, prospective, descriptive and analytical.
The target population of the study consisted of all patients diagnosed with first trimester spontaneous abortion (deferred abortion, accomplished incomplete abortion and anembryonic gestation) who have attended the Department of Gynecology and Obstetrics, University Hospital Clinico San Carlos (HCSC), and receiving medical or surgical treatment, in the period between June 2009 and December 2011, inclusive (study period: 30 months).
In order to apply the therapeutic option of medical treatment, abortions had to meet a number of sonographic criteria: in the case of incomplete abortions the cut-off point of 15 mm endometrial line has been set, the deferred abortions must have a Cephalus-spinal length (CSL) < 30 mm, and the anembryonic gestations have to have a gestational sac ≥ 20 mm with abdominal probe and 18 mm with vaginal probe.
In addition to the above ultrasound criteria and, being singleton pregnancies, the candidates for medical treatment also have to have less than 13 weeks amenorrhea and in the analytical control we have to objectify a hemoglobin ≥ 10g/dL, must comply with ambulatory surgery criteria, should have no allergy or hypersensitivity to the drug, previous diseases that contraindicate its use (mainly asthma or glaucoma) or coagulopathies.
Completed all the steps above, 800 μg (4 c) of misoprostol are placed vaginally, after exploration and annotation of the characteristics of pain, bleeding and collar state. Subsequently, the patient is told scheduled analgesia (paracetamol alternating with dexketoprofen 1 g/8 h vo vo 25 mg) and quoted at 7 days for control. In this control, protocol to follow is to request blood count with coagulation. The patient is explored to assess the bleeding, and the cervical and vaginal ultrasound is done to check the uterine evacuation. The attitude to follow will be conditioned by the uterine evacuation. Endometrial line < 15 mm: abortion is considered complete, and therefore, successful treatment; endometrial line > 15 mm or presence of gestational sac: it is considered that medical treatment has failed. The patient is given the possibility of evacuating surgical scraping or re-treatment with another 4 pills of misoprostol, after verification of normality of analytics. If the patient chooses curettage, it will not be scheduled for another dose of prostaglandin pre-operative cervical ripening, unless the gestational sac was full. If the content is between 15 mm and 20 mm, and is not suggestive of vascular blood clots ergot can be administered. Surgical treatment was applied in patients in whom medical therapy is contraindicated, in deferred abortions in > 30 mm CSL, or in case of refusal of medical treatment.
With the size of patients with first-trimester abortion (680), we have assumed a confidence level of 95% and a maximum error of 5% for the estimation of the main parameters.
The study was designed in 2008, and developed a protocol for the administration of medical treatment, which was reviewed and accepted by the Ethics Committee, validating the informed consent that is given to patients who wish to enter the study and the use of misoprostol as compassionate use. It was also developed a satisfaction survey.
With respect to the variables of the study, they were divided into independent and dependent.
The statistical evaluation of the results was performed using descriptive statistics and analytical tests or inferential test. In descriptive statistics, the study of qualitative variables was performed using percentages and frequency distribution. And the study of quantitative variables was performed by determining the mean and standard deviation.
To test the possible relationships between two or more variables and intensity of the relationship, inferential statistics or analytical is applied. For this we have applied the Student’s t-test when comparing two independent groups of variables that follow a normal distribution. If normality is not met, it performs the hypothesis test using the non-parametric Mann Whitney.
When comparing more than two groups of a quantitative variable, the analysis of variance has applied, when the variable followed a normal distribution. Failure to meet normality and/or homoscedasticity Kruskal Wallis non-parametric test was used. In the case of the relationship between two qualitative variables, contingency tables are used for description and Chi-square test of independence as homogeneity.
It has been considered the existence of statistical significance to that with P ≤ 0.05, establishing the confidence interval (CI) at 95%.
Data analysis was performed using the statistical software Stata (Data Analysis and Statistical Software), Version 11.
| Results | ▴Top |
With regard to the descriptive analysis of the behavior of the 680 patients diagnosed with first-trimester abortion, 599 received medical treatment, and 81 underwent curettage evacuator. In these 81 patients who underwent curettage, 61 refused medical treatment and the other 20 could not be applied due to medical contraindications (Fig. 1).
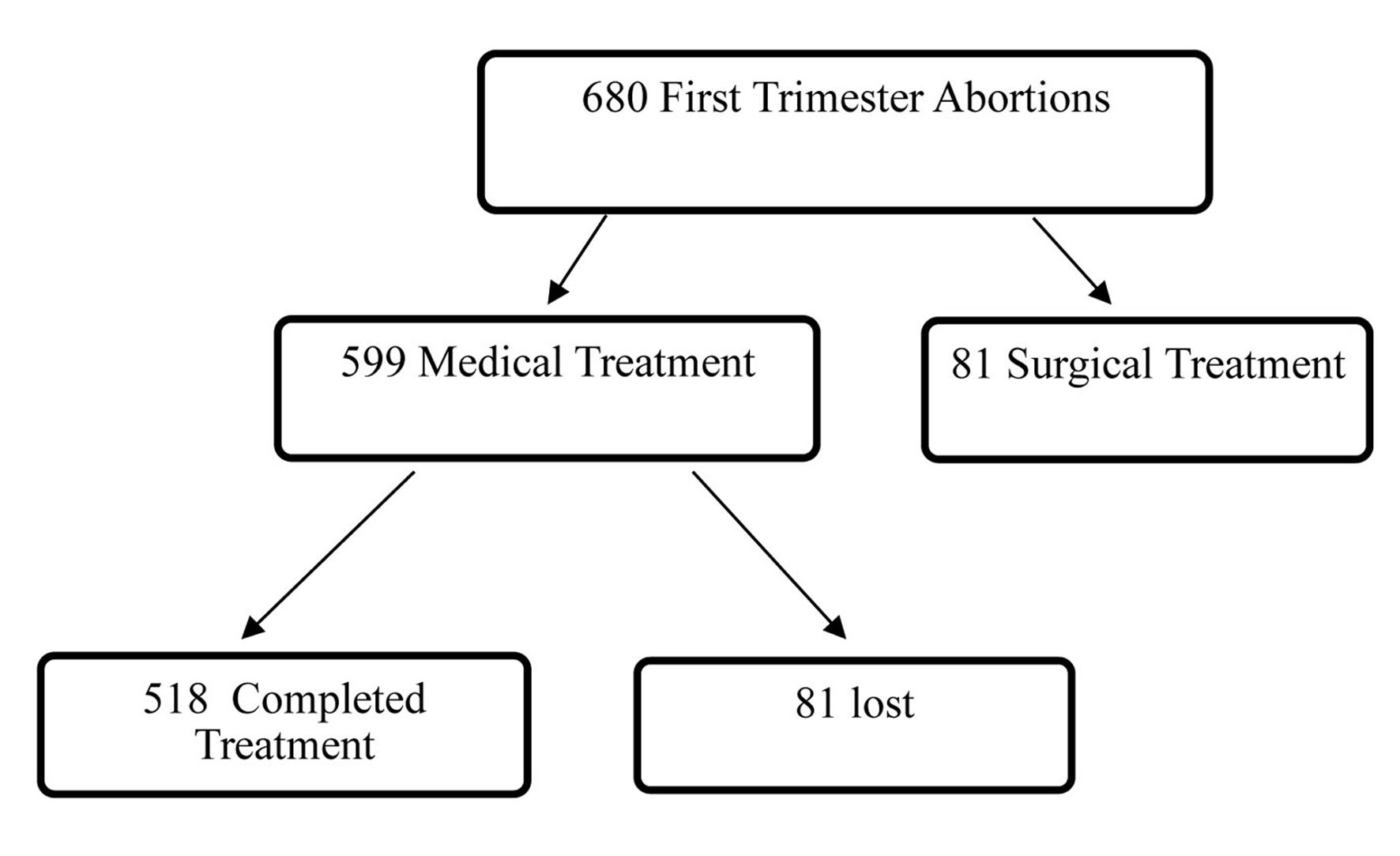 Click for large image | Figure 1. Treatment management algorithm of first trimester spontaneous abortion. |
Of the 518 patients who completed treatment, 371 hits were obtained, representing a 71.62% success rate. Seventy-two patients agreed to a retreat and 70 opted for curettage. Of the 72 retreats, 53 were successful, objectifying a success rate of 73.61% (Fig. 2). That is, overall medical treatment was successful in 424 of 518 patients, representing a success rate of 81.85%.
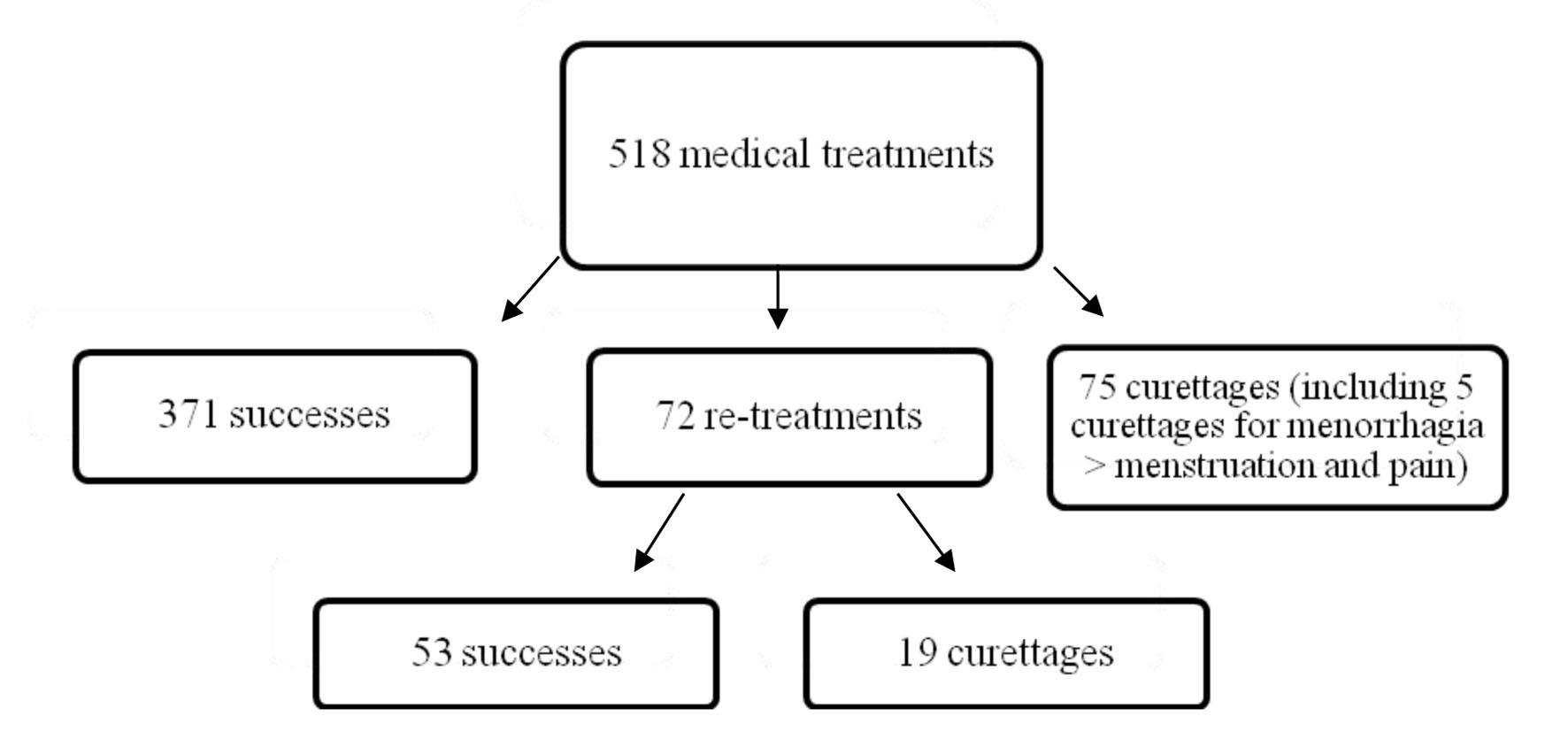 Click for large image | Figure 2. Descriptive analysis of therapeutic conduct. |
Side effects were recorded in 33.59% of patients, the most frequent were chills and vomiting second. As complications, four chorionic polyps were diagnosed. Transfusion was performed in one patient 10 days after being discharged following successful treatment. It also made four more metrorrhagia urgent curettage to rule the day after treatment administration and another by intense pain that would not budge after intravenous analgesia.
In Table 1 we can see that the success of medical treatment was higher in patients who had no previous cesarean or voluntary interruptions, in whom the exploration of the first day had pain and bleeding, which reported having continuous bleeding with application of misoprostol in patients taking scheduled analgesia and those who do not go to the emergency room. With regard to satisfaction, 84.99% of patients undergoing medical treatment feel satisfied.
 Click to view | Table 1. Bivariate Inferential Analysis Base on the Success of Medical Treatment |
The patients who present at the first visit accomplished incomplete abortion ultrasound diagnosis has revealed an increased success of medical treatment, 89.21%, followed by deferred abortions, 79.52% and anembryonic gestations,78.46%, with P = 0.030.
We found statistically significant relationship between the numerical value of the action taken in the ultrasound examination in the case of accomplished incomplete abortion and effectiveness of medical treatment, P = 0.007.
With respect to the cost study, since the expected average cost of curettage is €1,360 per patient and medical treatment including re-treatment and extra visits is €399.46 per patient, it is a saving of €960.54 per patient. If we only consider the patients in whom medical treatment is successful, there is a saving of €496,253.
In Figure 3 we can objectify since medical treatment was introduced in 2009, there has been a significant reduction in the number of curettages, which has resulted in significant savings in health care costs. Specifically, it reduced the need for curettage by 81.85%. In a sensitivity analysis, the percentage of patients requiring curettage after the first dose of misoprostol was 28.4% and after a retreat of 26.4%.
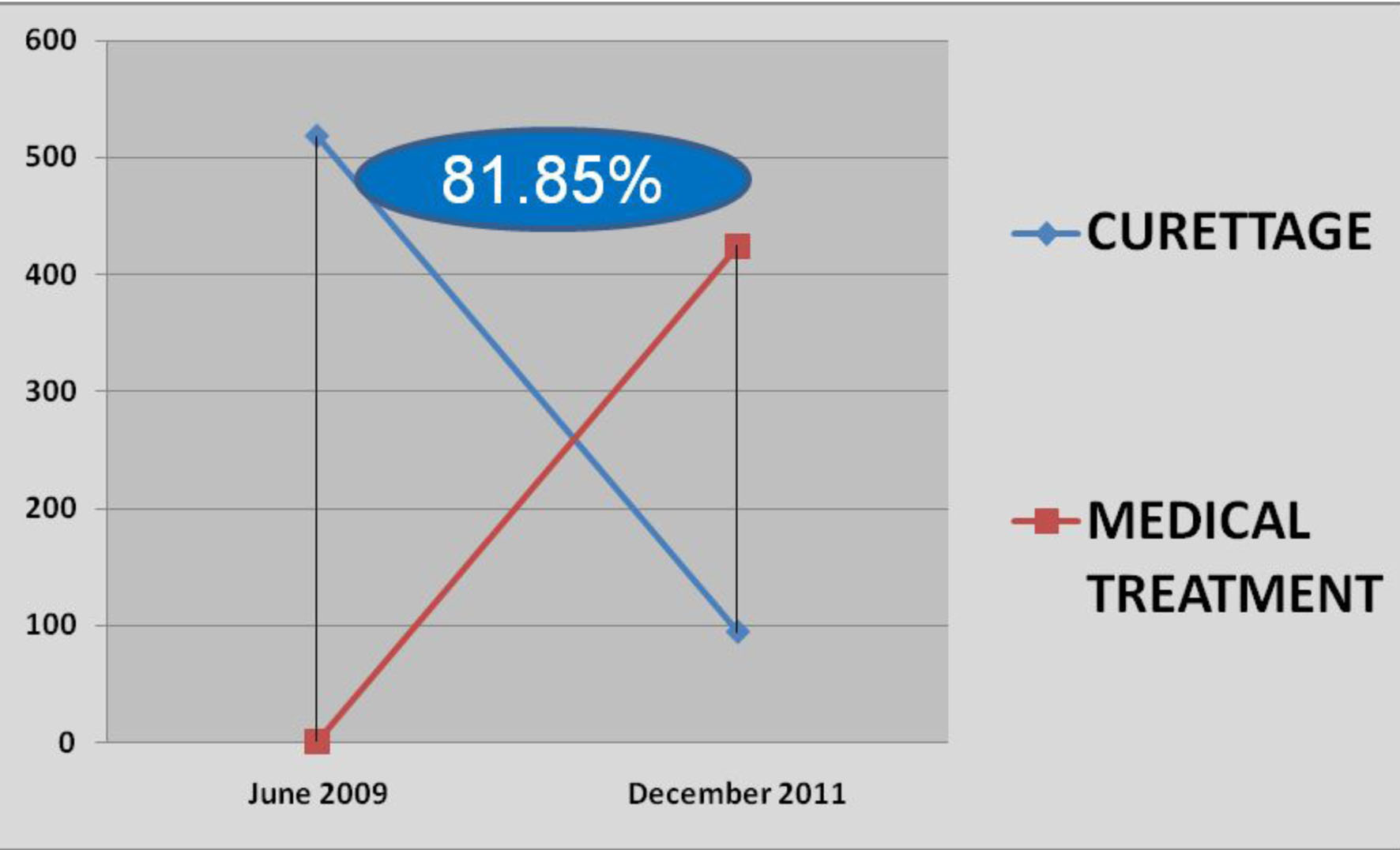 Click for large image | Figure 3. Decrease in the number of curettages. |
Therefore, half the average cost of medical treatment with extra visits to the emergency room, and including the five curettages performed before completing medical treatment (one for pain did not subside with metrorrhagia analgesia and four more than a menstruation), the average cost would be €399.46 per patient, thus reducing cost of medical treatment in conjunction with surgery would be 71%.
| Discussion | ▴Top |
After a detailed analysis of the variables discussed, in our work we found statistically significant relationship with the success of medical treatment for: previous cesarean section: the patients without previous cesarean respond better to misoprostol; voluntary interruptions: there is a statistically significant trend to success in patients without previous voluntary interruptions; types of abortions: they have objectified statistically significant differences between the different types of abortions, and treatment success was higher in patients with incomplete abortion, followed by deferred abortions, and the success rate being lower in the anembryonic gestation.
These results agree with those of the randomized trial of Zhang et al [1], which shows that the patients with anembryonic gestation have a success rate of medical treatment lower than other subtypes of spontaneous abortions.
Seeking greater efficiency, we have chosen for the via vaginal misoprostol administration; however, it has been to say that the consensus is almost unanimous, and this has been found in the literature that the vaginal route has clinical efficacy greater than the mouth.
The dose of misoprostol established in our protocol was 800 μg, this dose may be repeated 1 week in case of failure. We have relied on a review of studies of misoprostol in the treatment of accomplished incomplete abortion showing efficacy variable rate with a range of doses ranging from 400 - 1,200 μg. The highest dose tested was 600 μg. But it was observed that 800 μg repeated regimes showed a success rate slightly above [2-4].
For the incomplete abortions the proposed dose by OMS [1, 5, 6] is 600 μg vo as it has proven to be the smallest effective dose, with results almost as efficient as an aspiration curettage, with the same indication. But for deferred abortion [1, 7, 8], it has been observed that by increasing the dose to 800 μg and using the vaginal route the success rate improves.
In the protocol HCSC has decided to apply the same pattern (800 μg single dose, may repeat 1 week in case of failure, vaginally) in all cases of spontaneous abortion without distinction between incomplete or retained to facilitate training and implementation of treatment in our country, which is under heavy workload, to which is added the increase of the side effects caused by this higher dose (800 μg versus 600 μg), it is not valuable to look at the results of the existing literature.
One of the main problems of published trials on medical treatment is the definition of success. Studies of medical treatment, with success rates often exceeding 95%, do not consider endometrial thickness in its definition: what they have seen is that in patients in whom the gestational sac disappears, they may not require intervention. For this reason it may explain the high rate of success. Reynolds et al [9] also established the absence of gestational sac on trans-vaginal ultrasound as a success criterion for defining, documenting that is associated with higher rates of success in the short and long term, as well as mild and self-limiting symptoms in the days following treatment.
Creinin et al [10] argue that you cannot establish a direct relationship between endometrial thickness and whether or not curettage in patients with spontaneous abortion treated with misoprostol, which should be the clinical signs and symptoms rather than endometrial thickness to determine therapeutic decisions.
In other studies [1, 11], it is confirmed that most patients with endometrial thickness < 30 mm after medical treatment, have complete removal of the remains spontaneously and smoothly.
Regarding the effectiveness of medical treatment, there have been many studies using a variety of dosages, routes of administration and timeouts. In published studies, the success rate of misoprostol ranges from 13% (De George 1995 using 400 μg orally with observation time of 12 h and a sample size of 50 patients) to 100% (in the study of Ngai in 2001 using 400 μg vaginally, with an observation time of 15 days, 59 patients), with an average of approximate 92%. One example is Tang’s study in 2006, using 600 μg subl for 7 days, and 180 patients. In our study we have obtained a success rate of medical treatment of 81.85%, being the study with more patients, except Chung, 1999, with 635 patients, in which success was minor, as only 51%, and in which 400 μg vo used with an observation time of 24 h.
The success rates increase when the waiting time is up to 7 - 10 days and seem not to improve while continuing to wait until the 14th or 15th day. For this reason, we recommend a range of 7 - 10 days before evaluating the success of medical treatment and considering evacuating curettage option for residual intrauterine, and this criterion has been used in our protocol.
With respect to the efficacy of medical treatment, and comparing with the literature review, commenting that our study is the only one that includes a larger sample size using 800 μg vaginally PGE1 and showing an efficiency of 81.85%.
Side effects are more common in studies that used the oral route, probably because the peak plasma concentration of orally, is 1.6 times higher compared with vaginally. If we compare the side effects of our study with those of 2001 and Creinin Demetroulis 1997, using the same dose and route of administration as ours, in the study of Creinin incidence of diarrhea is 38%, while in the Demetroulis study and ours are not registered. However, in Demetroulis study we observed a rate of 10% hemorrhage, in ours of 0.7% and that of Creinin not recorded. Regarding blood loss, in our study the estimated difference of hemoglobin levels from baseline to end of treatment shows little relevance to blood loss (difference in mean hemoglobin 0.8 g/dL), which are in line with the results of other authors, who reported a mean hemoglobin decrease of 0.7 and 0.5 g/dL.
In our study, medical treatment is highly accepted by patients, and only 61 patients refused medical treatment versus 599, a finding consistent with the registered literature [12-14].
With regard to the psychological impact, in our study it has been observed less impairment in mood in the medical treatment group and found no statistically significant difference in the rate of satisfaction among both groups. These results are similar to research conducted in Hong Kong by Chung et al [15] who evaluated the psychological impact and patient satisfaction with medical treatment versus curettage.
The cost analysis showed that the direct cost per patient in the misoprostol group was less than that in the surgical group (€399.46 versus €1,360), with a difference of €960.54.
The strong impact on direct costs of therapy with misoprostol will be conditioned primarily by the need or not to complete treatment with a surgical technique. If medical treatment fails, direct costs are not decreased, but are increased by €85.72. If the second medical treatment fails, expenses increased by €172.44. Therefore, the need for surgical evacuation after failure of medical treatment is the main determinant of the cost of treatment. Similar results are found in studies of Graciosi, Doyle and Petrou [16-18].
The alternative medical treatment of spontaneous abortion in the first trimester is less expensive, producing a saving of €960.54 per patient treated. Therefore, we can say that our economic evaluation shows that medical treatment with misoprostol reduces the need for curettage and is a therapy that reduces the cost of managing the premature interruption of the first quarter.
There are 13 studies [1, 5, 6, 13, 14, 19-26] comparing medical treatment with curettage. The average success rate of misoprostol was 92% and 98% for curettage. In our study we observed a success rate of 81.85% and 97.5% respectively (two re-curettages by persistence of residues).
In our study, patients who choose medical treatment highlight the main advantage avoiding surgery, noting that the biggest drawback is bleeding; however, in the curettage group patients highlight the comfort and advantage, and the disadvantage that it is an invasive method. These results agree with those of Shwekerela, Bique and Graziosi [14, 20, 27], which show that patients prefer medical treatment to surgery, and it shows that patients with spontaneous abortion opt for medical treatment, even when their priority is the resolution of the process, they choose curettage [28].
In conclusion, we could say that in view of the efficiency and lower costs of management of first trimester spontaneous abortion with misoprostol, we believe that medical treatment could become the first choice of treatment, decreasing the burden on care facilities.
| References | ▴Top |
- Zhang J, Gilles JM, Barnhart K, Creinin MD, Westhoff C, Frederick MM. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. N Engl J Med. 2005;353(8):761-769.
doi pubmed - Creinin MD, Moyer R, Guido R. Misoprostol for medical evacuation of early pregnancy failure. Obstet Gynecol. 1997;89(5 Pt 1):768-772.
doi - Wood SL, Brain PH. Obstet Gynecol. 2002;100(1):175.
doi - Blum J, Winikoff B, Gemzell-Danielsson K, Ho PC, Schiavon R, Weeks A. Treatment of incomplete abortion and miscarriage with misoprostol. Int J Gynaecol Obstet. 2007;99(Suppl 2):S186-189.
doi pubmed - Trinder J, Brocklehurst P, Porter R, Read M, Vyas S, Smith L. Management of miscarriage: expectant, medical, or surgical? Results of randomised controlled trial (miscarriage treatment (MIST) trial). BMJ. 2006;332(7552):1235-1240.
doi pubmed - Weeks A, Alia G, Blum J, Winikoff B, Ekwaru P, Durocher J, Mirembe F. A randomized trial of misoprostol compared with manual vacuum aspiration for incomplete abortion. Obstet Gynecol. 2005;106(3):540-547.
doi pubmed - Tand OS, Lau WNT, Ng EHY, Lee SWH, Ho PC. Human Reprod. 2003;18:176-181.
doi - Phupong V, Taneepanichskul S, Kriengsinyot R, Sriyirojana N, Blanchard K, Winikoff B. Comparative study between single dose 600 microg and repeated dose of oral misoprostol for treatment of incomplete abortion. Contraception. 2004;70(4):307-311.
doi pubmed - Reynolds A, Ayres-de-Campos D, Costa MA, Montenegro N. How should success be defined when attempting medical resolution of first-trimester missed abortion? Eur J Obstet Gynecol Reprod Biol. 2005;118(1):71-76.
doi pubmed - Creinin MD, Harwood B, Guido RS, Fox MC, Zhang J. Endometrial thickness after misoprostol use for early pregnancy failure. Int J Gynaecol Obstet. 2004;86(1):22-26.
doi pubmed - Creinin MD, Huang X, Westhoff C, Barnhart K, Gilles JM, Zhang J. Factors related to successful misoprostol treatment for early pregnancy failure. Obstet Gynecol. 2006;107(4):901-907.
doi pubmed - Tang OS, Ho PC. The pharmacokinetics and different regimens of misoprostol in early first-trimester medical abortion. Contraception. 2006;74(1):26-30.
doi pubmed - Dao B, Blum J, Thieba B, Raghavan S, Ouedraego M, Lankoande J, Winikoff B. Is misoprostol a safe, effective and acceptable alternative to manual vacuum aspiration for postabortion care? Results from a randomised trial in Burkina Faso, West Africa. BJOG. 2007;114(11):1368-1375.
doi pubmed - Bique C, Usta M, Debora B, Chong E, Westheimer E, Winikoff B. International Journal of Gynaecology & Obstetrics. 2007;98:222-226.
doi pubmed - Lee DT CL, Haines CJ, Chung TK. American Journal of Obstetrics & Gynecology. 2001;185:953-958.
doi pubmed - Graziosi GC, van der Steeg JW, Reuwer PH, Drogtrop AP, Bruinse HW, Mol BW. Economic evaluation of misoprostol in the treatment of early pregnancy failure compared to curettage after an expectant management. Hum Reprod. 2005;20(4):1067-1071.
doi pubmed - Doyle NM, Jimenez-Flores J and Ramin MR. Obstet Gynecol. 2004;103(4):65.
- Petrou S, Trinder J, Brocklehurst P, Smith L. Economic evaluation of alternative management methods of first-trimester miscarriage based on results from the MIST trial. BJOG. 2006;113(8):879-889.
doi pubmed - Demetroulis C, Saridogan E, Kunde D, Naftalin AA. A prospective randomized control trial comparing medical and surgical treatment for early pregnancy failure. Hum Reprod. 2001;16(2):365-369.
doi pubmed - Shwekerela B, Kalumuna R, Kipingili R, Mashaka N, Westheimer E, Clark W, Winikoff B. Misoprostol for treatment of incomplete abortion at the regional hospital level: results from Tanzania. BJOG. 2007;114(11):1363-1367.
doi pubmed - de Jonge ET, Makin JD, Manefeldt E, De Wet GH, Pattinson RC. Randomised clinical trial of medical evacuation and surgical curettage for incomplete miscarriage. BMJ. 1995;311(7006):662.
doi pubmed - Moodliar S, Bagratee JS, Moodley J. International Journal of Gynaecology & Obstetrics. 2005;91:21-26.
doi pubmed - Shelley JM, Healy D, Grover S. Australian & New Zeland Journal of Obstetrics & Gynaecology. 2005;45:122-127.
doi pubmed - Chung T, Leung P, Cheung LP, Haines C, Chang AM. A medical approach to management of spontaneous abortion using misoprostol. Extending misoprostol treatment to a maximum of 48 hours can further improve evacuation of retained products of conception in spontaneous abortion. Acta Obstet Gynecol Scand. 1997;76(3):248-251.
pubmed - Sahin HG, Sahin HA, Kocer M. Randomized outpatient clinical trial of medical evacuation and surgical curettage in incomplete miscarriage. Eur J Contracept Reprod Health Care. 2001;6(3):141-144.
doi pubmed - Gronlund L, Gronlund AL, Clevin L, Andersen B, Palmgren N, Lidegaard O. Spontaneous abortion: expectant management, medical treatment or surgical evacuation. Acta Obstet Gynecol Scand. 2002;81(8):781-782.
doi pubmed - Graziosi GC, Bruinse HW, Reuwer PJ, Mol BW. Women's preferences for misoprostol in case of early pregnancy failure. Eur J Obstet Gynecol Reprod Biol. 2006;124(2):184-186.
doi pubmed - El-Refaey H, Templeton A. Unsuccessful treatment of missed abortion. Br J Obstet Gynaecol. 1998;105(5):567-568.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
