| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 4, Number 4, December 2015, pages 316-319
Embolization for Postpartum Hemorrhage Due to Uterine Arteriovenous Malformation: A Case Report
Prakash Mehtaa, Monali Pawarb, c
aDepartment of Maternal and Fetal Medicine, Bhagwan Mahaveer Jain Hospital, Millers Road, Bangalore 560052, India
bDepartment of Obstetrics and Gynaecology, Bhagwan Mahaveer Jain Hospital, Millers Road, Bangalore 560052, India
cCorresponding Author: Monali Pawar, Department of Obstetrics and Gynaecology, Bhagwan Mahaveer Jain Hospital, Millers Road, Bangalore 560052, India
Manuscript accepted for publication October 21, 2015
Short title: PPH due to uterine AV malformation
doi: http://dx.doi.org/10.14740/jcgo366w
| Abstract | ▴Top |
Postpartum hemorrhage (PPH) is one of the leading causes of maternal morbidity and mortality. Its prompt recognition and management is life-saving. Hysterectomy can be avoided by using the conservative methods. Uterine artery embolization is a safe and effective procedure and can be life-saving. We have discussed a similar case which was managed successfully with uterine artery embolization.
Keywords: AV malformation; Postpartum hemorrhage; Uterine artery embolization
| Introduction | ▴Top |
Maternal deaths all over the world can be attributed to a triad comprising of obstetrical hemorrhage, hypertension and sepsis. Postpartum hemorrhage (PPH), which is seen in 18% of births, is one of the major causes of maternal morbidity and mortality. One of the rare causes of PPH can be uterine arteriovenous (AV) malformation. A uterine AV malformation results from formation of multiple AV fistulous communications within the uterus without an intervening capillary network. The size of these vessels and its presentation can vary considerably.
| Case Report | ▴Top |
A 28-year-old primigravida underwent an uneventful cesarean delivery for non-progress of labor and fetal distress and delivered a live male baby of 3.5 kg. Two hours after surgery, patient had bout of bleeding of nearly 1,000 mL, which was managed with uterotonics and uterine packing for 12 h. Two units of packed cells were transfused. After 12 h, pack was removed and no fresh bleeding was noted.
The patient had a second episode of bleeding again after 18 h. On examination, vitals remained stable and uterus was well contracted. One liter of clots was removed from the vagina. Uterotonics were given and patient was referred to our institution.
Patient was admitted to ICU, and stabilized. Four units of packed cells were transfused. Ultrasound showed possible retained products, and scan-guided evacuation under anesthesia was done. Decidua along with a few small clots was obtained. No active bleeding was noted during the process. On fourth day, patient again had bleeding, PV ultrasonography done showed a uterus measuring 129 × 95 × 68 mm size and a well-defined lesion in the fundus was noted with multiple cystic areas within. Color Doppler showed multiple arterial and venous vascularity (Fig. 1). A diagnosis of uterine AV malformation was made and because of repeated bouts of heavy bleeding per vagina, patient was taken up for uterine artery embolization. Under local sedation (Rt) femoral approach, 5F sheath and 5F Robertson uterine catheter was used. Selective catheterization of left and right uterine artery was done and embolized with PVA particles 700 μm size.
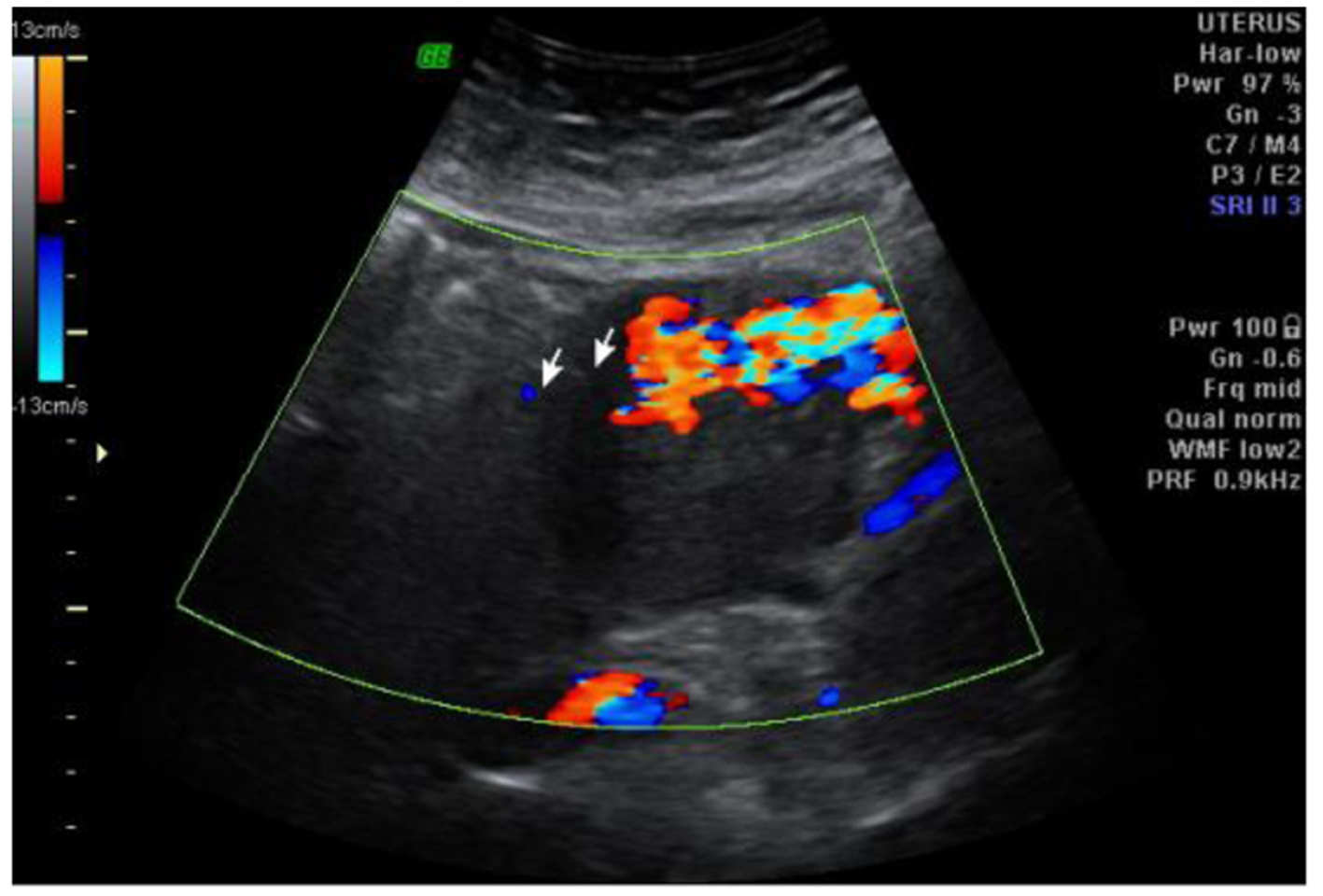 Click for large image | Figure 1. Scan and Doppler showing uterine AV fistula. |
Post-procedure angiography showed reduction of flow in both uterine arteries (Fig. 2). Repeat scan done 24 h later showed no evidence of AV malformation and postpartum involuting uterus (Fig. 3). Patient did not have any further episodes of bleeding.
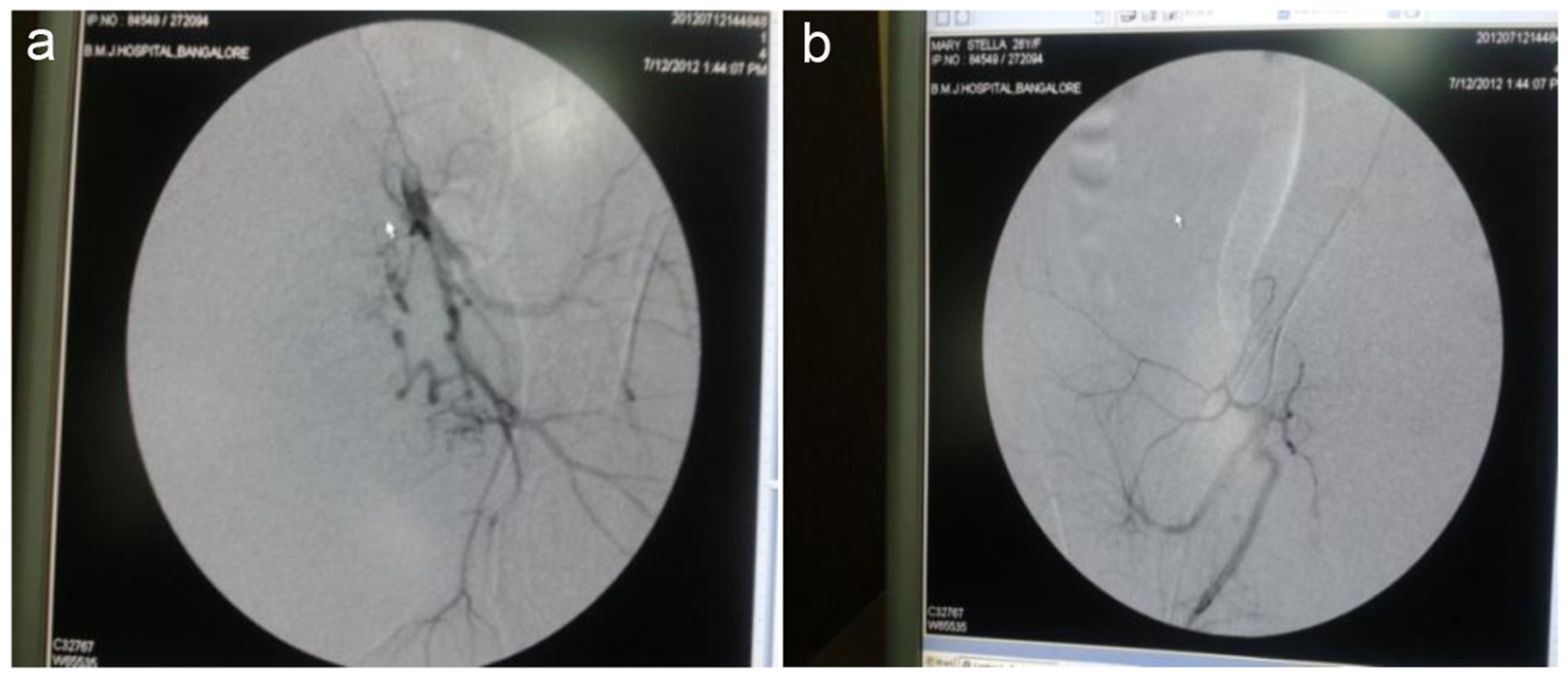 Click for large image | Figure 2. Uterine artery embolization done: (a) prior to embolization; (b) post-embolization. |
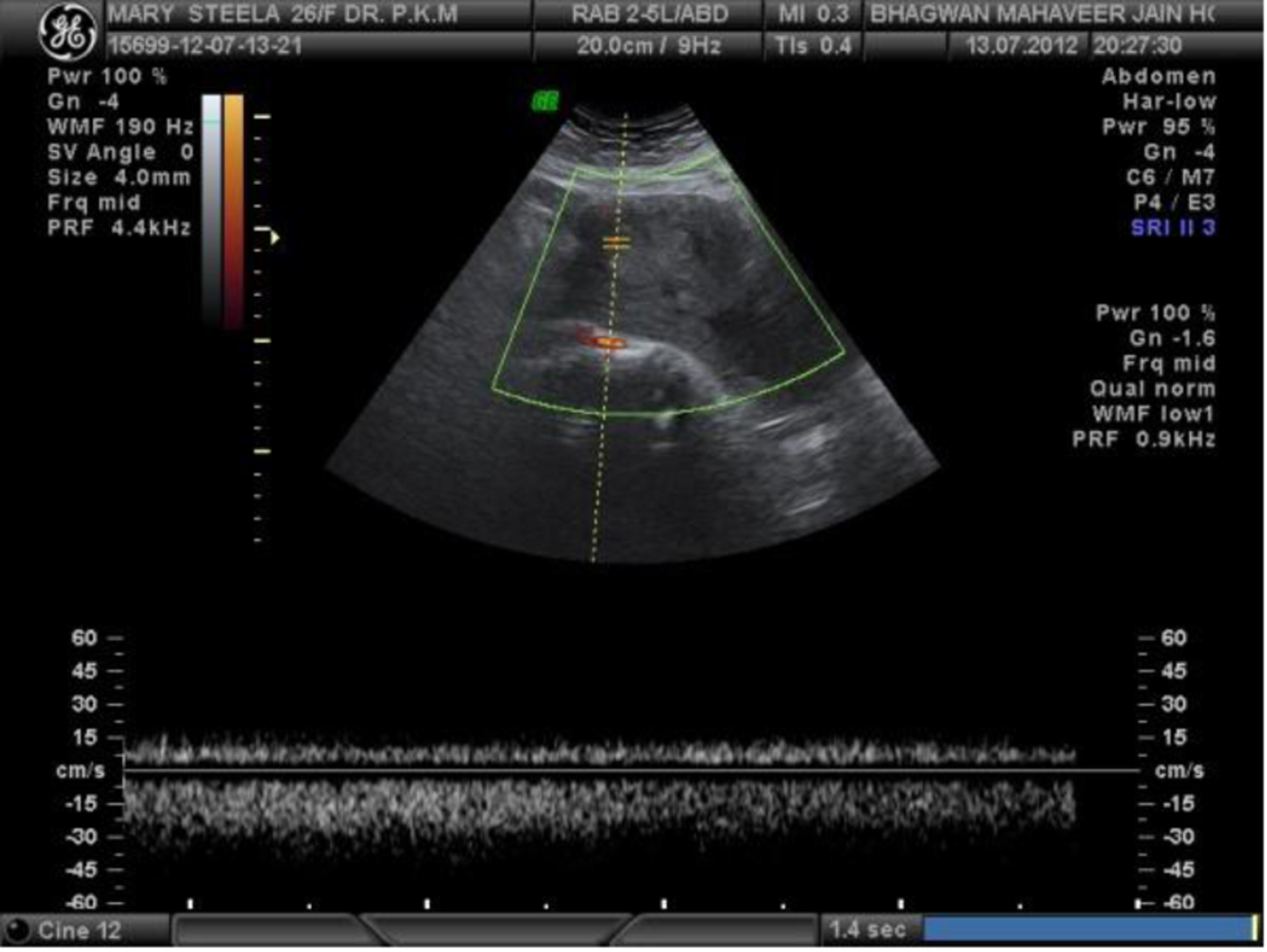 Click for large image | Figure 3. Repeat scan and Doppler showing involuting uterus with normal Doppler. |
| Discussion | ▴Top |
Uterine AV malformations first described by Dubreil and Loubat in 1926 [1] can be congenital or acquired. Congenital uterine AV malformations tend to have multiple feeding arteries, a central nidus (a tangle of vessels with histologic characteristics of both arteries and veins), and numerous large draining veins [2]. Acquired or traumatic uterine AV malformations represent multiple small AV fistulas between intramural arterial branches and the myometrial venous plexus [3]. They typically represent a single artery joining a simple vein. Acquired uterine AV malformations are commonly seen with spontaneous or therapeutic abortion, multiple pregnancies, previous dilation and curettage and/or cesarean section [4, 5].
AV malformation on grayscale ultrasound can have variable manifestations such as in homogenous areas or tubular spaces in the myometrium, prominent parametrial vessels or endometrial or cervical mass-like region [6]. Color Doppler done for confirmation over these serpiginous/tubular anechoic structures within the myometrium has a low resistance (RI: 0.2 - 0.5) and a high velocity flow pattern. MRI can also be used for diagnosis. Multiple serpentine flow-related signal voids are typically seen in the uterine wall, endometrial cavity, and parametrium on T1- and T2-weighted images. Contrast-enhanced dynamic MR angiography can depict complex serpentine abnormal vessels that enhance as intensely as normal vessels and show early venous return [4]. Transcatheter arterial embolization for treatment of AV fistulas is quite promising. Previously gelfoam was used for embolization as the 3- to 5-week duration of occlusion is sufficient to prevent further hemorrhage while permitting slow development of collateral vessels and thus preventing ischemia [7]. More recent studies have suggested PVA particles [8] or glue (N-butyl-cyanoacrylate) [9] as agents of choice. There is no study on the embolic agent that shows a statistically different clinical outcome.
Bleeding presumably occurs when the vessels erode or abut the endometrium becoming exposed in the process. The pattern of bleeding is usually intermittent and torrential, and sometimes significant enough to require multiple blood transfusions.
Management of these cases varies from conservative management to surgery. Fleming et al reported six cases of AV malformation. All of their patients underwent total abdominal hysterectomies for life-threatening hemorrhage. Wiebe and Switzer reported seven cases of AV malformations diagnosed by color Doppler sonography, and subsequently managed the cases conservatively [10, 11]. They reported 100% spontaneous resolution.
More recently, uterine AV malformations have been treated successfully by intra-arterial embolization with particulate matter in various surgical hemorrhagic conditions. Substances for embolization used singly or in combination include gel foam, microfibrillar collagen, isobutyl cyanoacrylate, and steel coil spring occluders.
Pregnancy following conservative medical management of AV malformation and even after successful embolization, although rare has been reported in literature [12-14].
The question of why some patients respond to conservative management while others require surgical intervention needs to be addressed. Choice of management is probably dictated by the site and size of the lesion. Large lesions involving the subendometrial tissue usually require surgical intervention while others respond to conservative management.
| References | ▴Top |
- Dubreil G, Loubat E. Aneurysmecirsoide de l'uterus. Ann AnatPathol. 1926;3:697-718.
- Kwon JH, Kim GS. Obstetric iatrogenic arterial injuries of the uterus: diagnosis with US and treatment with transcatheter arterial embolization. Radiographics. 2002;22(1):35-46.
doi pubmed - Cura M, Martinez N, Cura A, Dalsaso TJ, Elmerhi F. Arteriovenous malformations of the uterus. Acta Radiol. 2009;50(7):823-829.
doi pubmed - Nagayama M, Watanabe Y, Okumura A, Amoh Y, Nakashita S, Dodo Y. Fast MR imaging in obstetrics. Radiographics. 2002;22(3):563-580; discussion 580-562.
- Grivell RM, Reid KM, Mellor A. Uterine arteriovenous malformations: a review of the current literature. Obstet Gynecol Surv. 2005;60(11):761-767.
doi pubmed - Huang MW, Muradali D, Thurston WA, Burns PN, Wilson SR. Uterine arteriovenous malformations: gray-scale and Doppler US features with MR imaging correlation. Radiology. 1998;206(1):115-123.
doi pubmed - Vedantham S, Goodwin SC, McLucas B, Mohr G. Uterine artery embolization: an underused method of controlling pelvic hemorrhage. Am J Obstet Gynecol. 1997;176(4):938-948.
doi - Lim AK, Agarwal R, Seckl MJ, Newlands ES, Barrett NK, Mitchell AW. Embolization of bleeding residual uterine vascular malformations in patients with treated gestational trophoblastic tumors. Radiology. 2002;222(3):640-644.
doi pubmed - Ghai S, Rajan DK, Asch MR, Muradali D, Simons ME, TerBrugge KG. Efficacy of embolization in traumatic uterine vascular malformations. J Vasc Interv Radiol. 2003;14(11):1401-1408.
doi pubmed - Timmerman D, Van den Bosch T, Peeraer K, Debrouwere E, Van Schoubroeck D, Stockx L, Spitz B. Vascular malformations in the uterus: ultrasonographic diagnosis and conservative management. Eur J Obstet Gynecol Reprod Biol. 2000;92(1):171-178.
doi - Flynn MK, Levine D. The noninvasive diagnosis and management of a uterine arteriovenous malformation. Obstet Gynecol. 1996;88(4 Pt 2):650-652.
doi - Beller U, Rosen RJ, Beckman EM, Markoff G, Berenstein A. Congenital arteriovenous malformation of the female pelvis: a gynecologic perspective. Am J Obstet Gynecol. 1988;159(5):1153-1160.
doi - Goldberg RP, Flynn MK. Pregnancy after medical management of a uterine arteriovenous malformation. A case report. J Reprod Med. 2000;45(11):961-963.
pubmed - Chow TW, Nwosu EC, Gould DA, Richmond DH. Pregnancy following successful embolisation of a uterine vascular malformation. Br J Obstet Gynaecol. 1995;102(2):166-168.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
