| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 5, Number 1, March 2016, pages 45-49
Endoscopy Management of Endometrial Ossification Associated With Secondary Infertility: A Case Report and Review of Literature
Gninlgninrin Apollinaire Horoa, c, Kacou Edele Akaa, Aboulaye Toureb, Abdoul Koffia, Konan Senia, Mamourou Konea
aFelix Houphouet Boigny University, Gynaecology Obstetrics Department, Teaching Hospital of Yopougon, Abidjan, Cote d’Ivoire
bFelix Houphouet Boigny University, Imaging Department, Teaching Hospital of Yopougon, Abidjan, Cote d’Ivoire
cCorresponding Author: Gninlgninrin Apollinaire Horo, Felix Houphouet Boigny University, Gynaecology Obstetrics Department, Teaching Hospital of Yopougon, Abidjan, Cote d’Ivoire
Manuscript accepted for publication February 04, 2016
Short title: Endoscopy and Osseous Metaplasia
doi: http://dx.doi.org/10.14740/jcgo385w
| Abstract | ▴Top |
The osseous metaplasia of the endometrium is a rare disease. It is very often discovered incidentally during the balance sheet infertility in women. The lesion is suspected in an ultrasound, a hysterosalpingography or a hysteroscanner. However, the diagnosis and treatment are done with hysteroscopy. It is either secondary to an abortion with persistence of fetal bone or due to a true osseous metaplasia of endometrial tissue. We report a case of a patient diagnosed with bone metaplasia in hysteroscanner and treated with hysteroscopy. The patient contracted a spontaneous pregnancy 12 months later, which resulted in the birth of a living child weighing 3,000 g.
Keywords: Osseous metaplasia; Infertility; Hysteroscopy; Hysteroscanner
| Introduction | ▴Top |
The endometrium osteoid metaplasia also called endometrial ossification or intrauterine ectopic bone is a rare disease. Its etiology and pathogenesis are controversial [1, 2]. The ossification of fetal bones has for a long time been retained as the most plausible hypothesis, suggesting an endochondral ossification. It occurs after therapeutic spontaneous abortions. This transformation of mesenchymal tissue in bone tissue is produced as a response to inflammation and repair process induced by abortion [3]. However, some cases of endometrial ossification have been reported after abortion at a very early stage of pregnancy or without a history of pregnancy, suggesting a metaplasia of stromal mature cells of endometrium [4]. Bone metaplasia is very often associated with infertility and endoscopy has an important role in its diagnosis and its surgical management [5].
We report a case of a patient at 28 years old who had a metaplasia with endometrial ossification associated with secondary infertility.
| Case Report | ▴Top |
A 28-year-old woman with secondary infertility was admitted to our infertility unit. Her obstetric history was marked by two clandestine abortions followed by uterine curettage for pregnancies of 15 weeks of amenorrhea. These endo-uterine maneuvers were practiced 11 and 9 years ago, respectively. She had presented in 2012 an irregular menstrual cycle (spaniomenorrhea) and a transvaginal ultrasound highlighted a uterine synechia, for which surgical treatment was performed.
The examination of the patient was normal. Transvaginal ultrasound suggested a hyper-echogenic image for a recurrence of uterine synechia. In the diagnostic strategy to investigate uterine cavity and tubal patency, a hysteroscanner without injection was performed. It revealed endometrial calcification of 22.3 mm in major axis evoking an osteoid metaplasia (Fig. 1). After injection, we noted normal size of uterine with regular contours. The cervical-isthmus parade was normal. The fallopian tubes were permeable (Fig. 2). The hysteroscopy diagnosis meanwhile highlighted an empty uterine cavity with a subsequent endometrial hypertrophy with a white coral plate approximately 2 cm in length (Fig. 3).
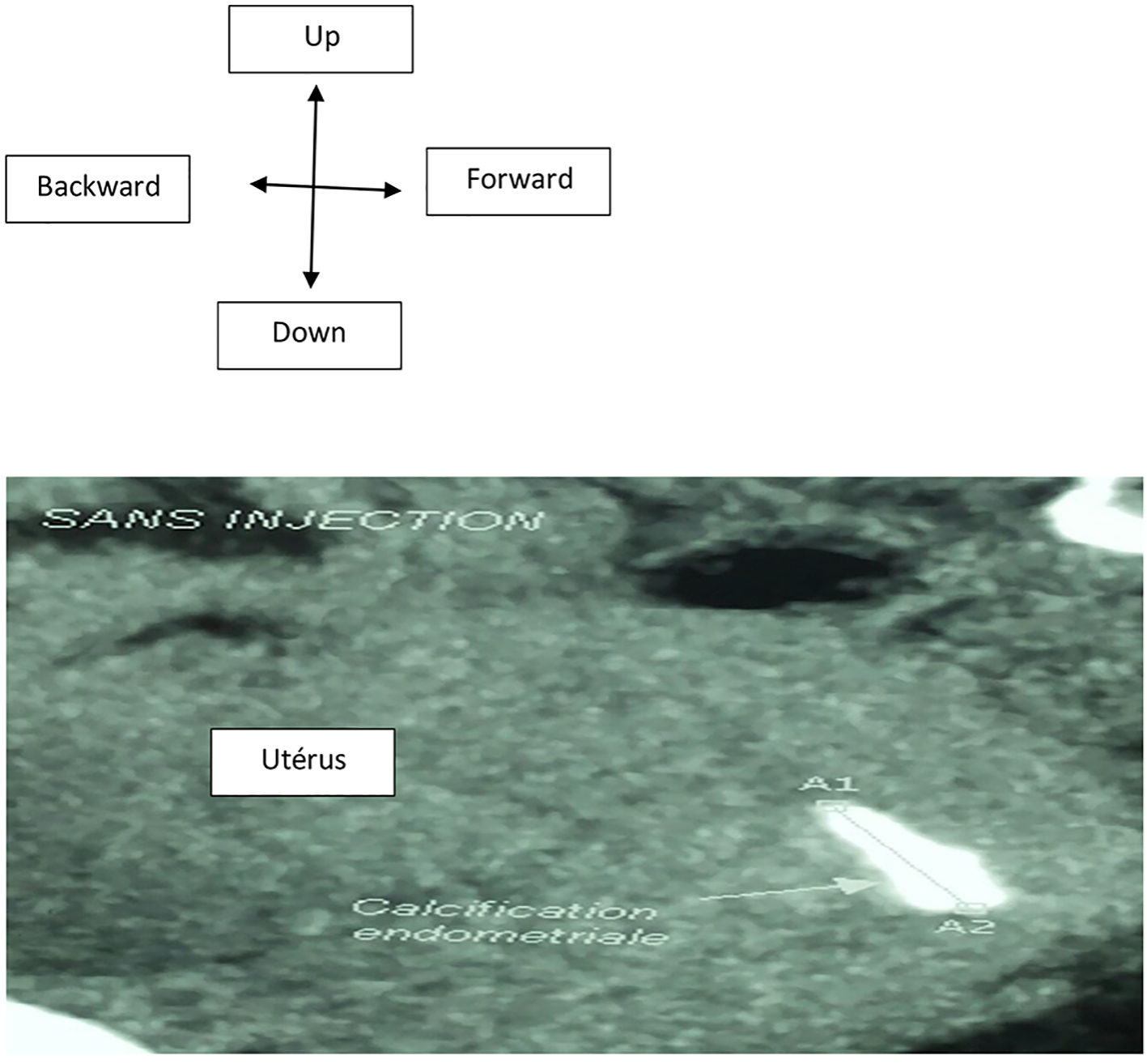 Click for large image | Figure 1. Hysteroscanner axial cup: before injection of the contrast agent, spontaneous hyperdensity within the endometrium about 22.3 mm diameter. |
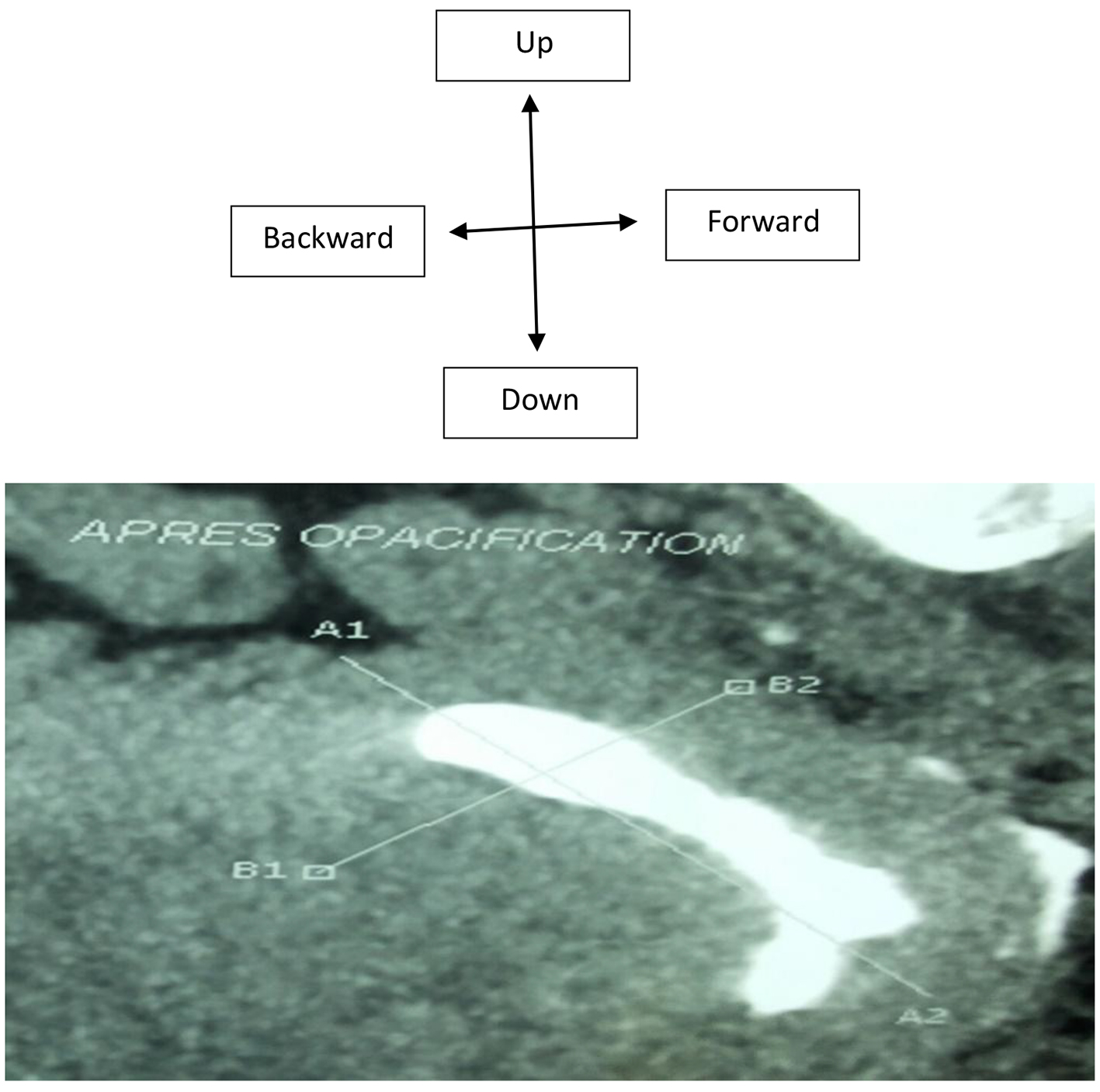 Click for large image | Figure 2. Hysteroscanner coronal reconstruction after injection of the contrast agent. The uterine cavity was made opaque and the hyperdensity within it was flooded. |
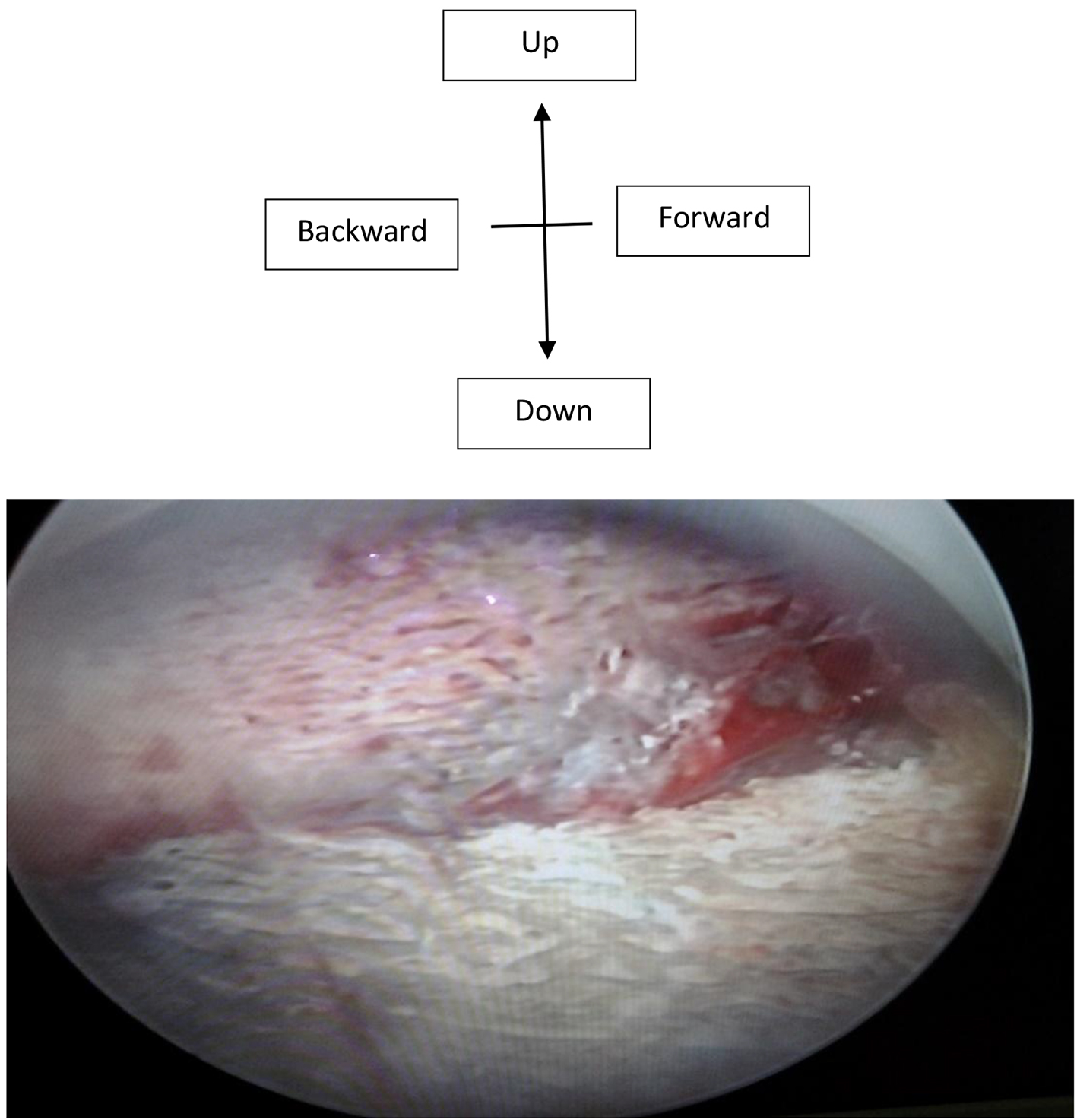 Click for large image | Figure 3. Hysteroscopy diagnoses highlighting posterior endometrium hypertrophy like white coral about 2 cm in length. |
Surgery
The lesion was successfully treated by resection of bone tissue without any complications (Fig. 4). The diagnosis and operative hysteroscopy were performed in the same operative time under general anesthesia; uterine cavity was distended with mannitol solution under 100 mm Hg pressure. Histological examination showed a chronic nonspecific endometritis with a dystrophic calcification.
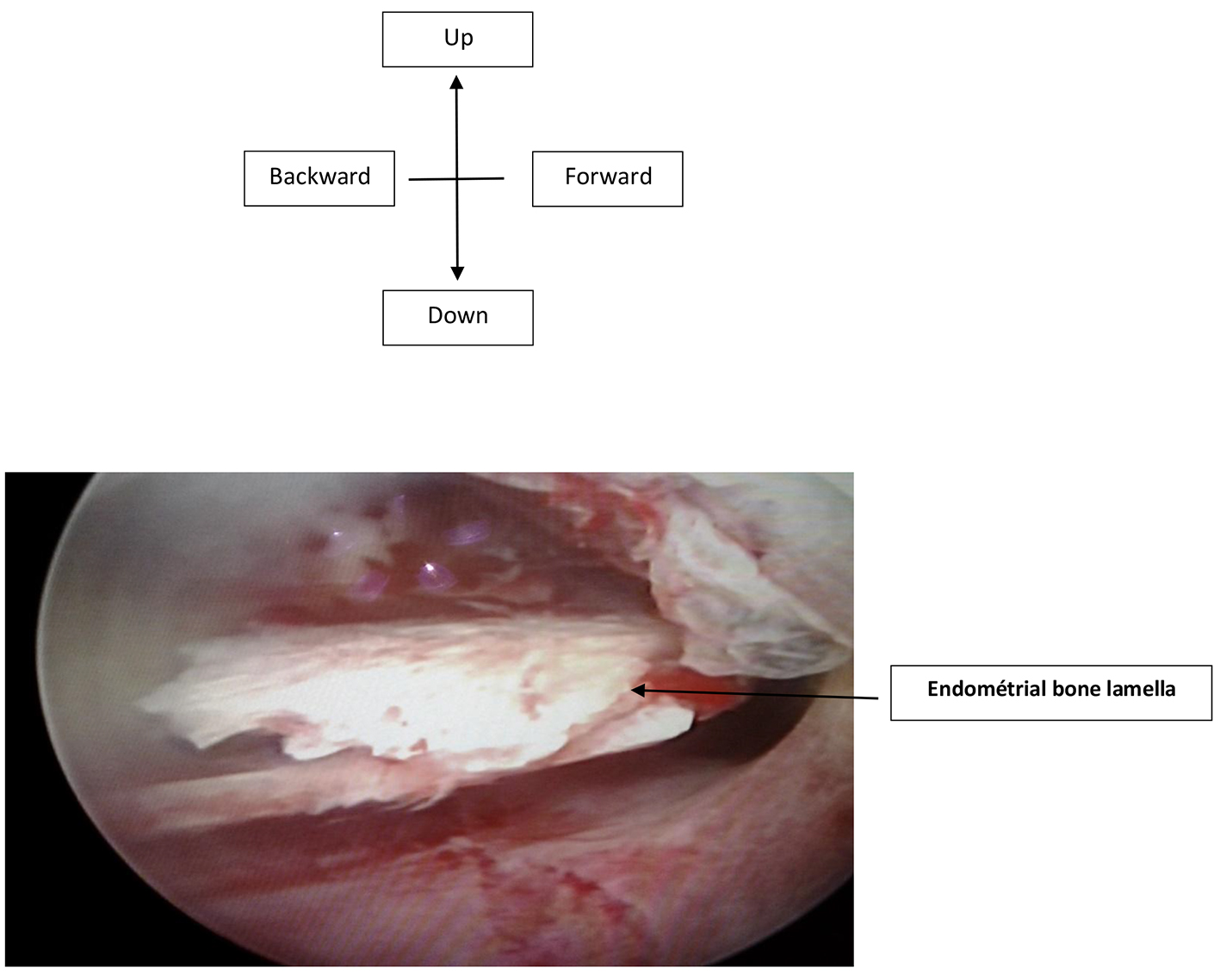 Click for large image | Figure 4. Hysteroscopy with endometrial bone tissue in uterine cavity. |
Postoperative follow-up
A second-look hysteroscopy was scheduled after 2 months to assess the surgical outcome.
| Discussion | ▴Top |
Several theories have been developed to explain the atypical endometrial transformation into bone tissue. Thaler in 1923 [4] blamed fetal bone tissue because ossification of the endometrium is often secondary to an abortion episode. Continued and strong estrogenic stimulation of the endometrium as well as retention of fetal bone promotes secondarily osteogenesis in the surrounding endometrium according to Newton and Abel [6]. The ossification of the endometrium would result in a real bone metaplasia after the comparative analysis of two DNA genotypes of ossified tissue and a woman was diagnosed infertile. This theory was demonstrated by Cayuela et al in 2009 [2].
Many authors propose different explanations which can be summarized into two main groups [7]. 1) Either by the persistence of embryonic bones which continue to develop after uterine curettage or by the appearance of bone tissue that is a result of the persistent inflammation of remains non-bone necrotics of embryonic tissue. Some sources of chronic inflammation that occurs from embryonic tissue retained after abortion in the first quarter like the chronic nonspecific endometritis. This inflammation acts as a promoter of secondary bone formation from bone non-embryonic tissues [8]. This assumption would correspond to our case in whom two curettages were done in her obstetrical history and an advanced age of pregnancy. 2) Either by induction of osteogenesis by the own stem cells, causing the bone differentiation of pluripotent endometrial cells. Chronic endometritis also stimulates the proliferation of mesenchymal cells that have the inherent property of metaplasia of differentiating into osteoblasts or chondroblasts.
Other etiologic mechanisms have been mentioned as heterotopia, dystrophic calcifications, ossification of endometritis post-abortive, metastatic calcification, metaplasia in tissue healing, and extended estrogen therapy after abortion as well as metabolic disorders such as hypercalcemia, hyperphosphatemia, and hypervitaminosis D [1]. However, the effective participation of these pathogenic mechanisms to metaplastic transformation remains hypothetical [9].
Furthermore, for most authors, the time interval between the previous abortion and the detection of endometrial ossification varies from 8 weeks to 15 years [2]. In our case, this interval between abortion and diagnosis varies from 9 to 11 years. The uterine bleeding, dysmenorrhea, vaginal discharge, and the pelvialgies are all symptoms that show bone metaplasia outside secondary infertility [10]. This secondary motive was foreground in our observation, associated with cycle disorders. These nonspecific symptoms can often wander the diagnosis and this diagnosis was delayed sometimes overlooked.
On the imaging plane, the differential diagnosis (ultrasound, hysterosalpingography or hysteroscanner) should be done with intrauterine devices (IUDs), intrauterine foreign body, uterine fibroids submucosal calcified and uterine synechia. Our patient was treated for a synechia which was probably an ossification of the endometrium.
Most authors describe the hysteroscopy as the gold standard for the diagnosis of endometrial pathology such as osteoid metaplasia. It has a dual diagnostic and therapeutic interest. Acharya et al [3] have been the first to perform endoscopic resection in a carrier woman of bone metaplasia. Over the years, the excision technique has improved to reduce the complications while and after surgical act. Given the limited access to hysteroscopy and the cost of intervention in our countries with limited resources, hysteroscanner is an alternative in the exploration of bone metaplasia of the endometrium.
Apart from other causes of infertility, the majority of studies done show the possibility of spontaneous pregnancy after hysteroscopic resection of bone fragments.
Conclusion
Endometrium osteoid metaplasia is a rare pathology, which is often the result of an abortion and a source of menstrual disorders and infertility. The diagnosis and the treatment are based on the uterine endoscopy; however, in low setting countries, hysteroscanner keeps a special place in the exploration of the uterine cavity in case of secondary infertility.
| References | ▴Top |
- Umashankar T, Patted S, Handigund R. Endometrial osseous metaplasia: Clinicopathological study of a case and literature review. J Hum Reprod Sci. 2010;3(2):102-104.
doi pubmed - Cayuela E, Perez-Medina T, Vilanova J, Alejo M, Canadas P. True osseous metaplasia of the endometrium: the bone is not from a fetus. Fertil Steril. 2009;91(4):1293 e1291-1294.
- Acharya U, Pinion SB, Parkin DE, Hamilton MP. Osseous metaplasia of the endometrium treated by hysteroscopic resection. Br J Obstet Gynaecol. 1993;100(4):391-392.
doi pubmed - Thaler H. Uberlebendes fotales knorpelgewebe in der uterushohel nach abortus. Zentralbl Gynakol. 1923;46:1784-1787.
- Lainas T, Zorzovilis I, Petsas G, Alexopoulou E, Lainas G, Ioakimidis T. Osseous metaplasia: case report and review. Fertil Steril. 2004;82(5):1433-1435.
doi pubmed - Newton CW, 3rd, Abell MR. Iatrogenic fetal implants. Obstet Gynecol. 1972;40(5):686-691.
pubmed - Singh P, Kapur K, Singla S, Naz N. Endometrial osseous metaplasia and mature bone formation with extramedullary hematopoiesis. J Hum Reprod Sci. 2011;4(1):56-57.
doi pubmed - Marcus SF, Bhattacharya J, Williams G, Brinsden P, Hamou J. Endometrial ossification: a cause of secondary infertility. Report of two cases. Am J Obstet Gynecol. 1994;170(5 Pt 1):1381-1383.
doi - Torne A, Jou P, Pagano R, Sanchez I, Ordi J, Vanrell JA. Endometrial ossification successfully treated by hysteroscopic resection. Eur J Obstet Gynecol Reprod Biol. 1996;66(1):75-77.
doi - Pace S, Torcia F, Palazzetti PL, Piazze JJ, Cipriano L, Pachi A. Successful diagnostic and surgical hysteroscopy for endometrial ossification. Clin Exp Obstet Gynecol. 2001;28(1):24-25.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
