| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 1, Number 2-3, June 2012, pages 46-48
Necrotizing Fasciitis Following Hysterectomy: A Case Report
Murat Apia, Hakan Aytana, Cevdet Adlguzela, Hakan Nazika, b, Raziye Narina, Ahmet Kalea
aDepartment of Obstetrics and Gynecology, Adana Numune Education and Research Hospital, Adana, Turkey
bCorresponding author: Hakan Nazik
Manuscript accepted for publication February 14, 2012
Short title: Necrotizing Fasciitis Following Hysterectomy
doi: https://doi.org/10.4021/jcgo4w
| Abstract | ▴Top |
Necrotizing fasciitis is a life-threatening, rapidly progressive bacterial infection that involves the subcutaneous tissues and fascias. A 45 years old obese, nulligravid woman who had diabetes mellitus, hyperlipidemia and coronary artery disease was hysterectomized for leiomyoma and abnormal uterine bleeding. Following the operation in the 6th postoperative day necrotizing fasciitis developed and skin, subcutaneous tissues, and fascia were excised widely. After excision, the intestines were packaged with Bogota Bag and the abdomen was left open. The patient was followed with antibiotics, daily wound dressing, and re-debridement when necessary. In postoperative 35th day the patient was discharged from the hospital. In gynecology necrotizing fasciitis is rare and a successfully managed case is presented.
Keywords: Necrotizing fasciitis; Bogota bag; Debridement
| Introduction | ▴Top |
Necrotizing fasciitis is a rare infection in gynecology. Its usual clinical presentation is a rapid progression of a wound infection and a postoperative soft tissue infection that does not respond to therapy. The disease is typically characterized by a rapidly progressive bacterial infection that involves the subcutaneous tissues and fascias, but not the underlying muscles. Dehydration, septic shock, disseminated intravascular coagulation, multi-organ failure and systemic toxicity are the clinical presentations. Hemolytic streptococci, gram positive micro-organisms, coliforms and anaerobes as well as other many organisms have roles in the etiology [1]. Skin involvement is the initial sign with erythema and local temperature rise. Afterwards edema develops and the infection spreads to the adjacent tissues. Micro-vascular thrombosis in the subcutaneous tissues and consequently ischemia of the skin, results in development of cyanosis and necrosis respectively. In addition during physical examination or X-ray studies subcutaneous gas formation may also be detected. Successful treatment of necrotizing fasciitis includes early diagnosis, administration of wide spectrum antibiotics and supportive therapies, surgical debridement and re-debridement when necessary [1, 2]. Hyperbaric oxygen therapy may also be useful especially in patients who have anaerobic micro-organisms [2]. In the present study a case of necrotizing fasciitis that developed after hysterectomy is presented.
| Case Report | ▴Top |
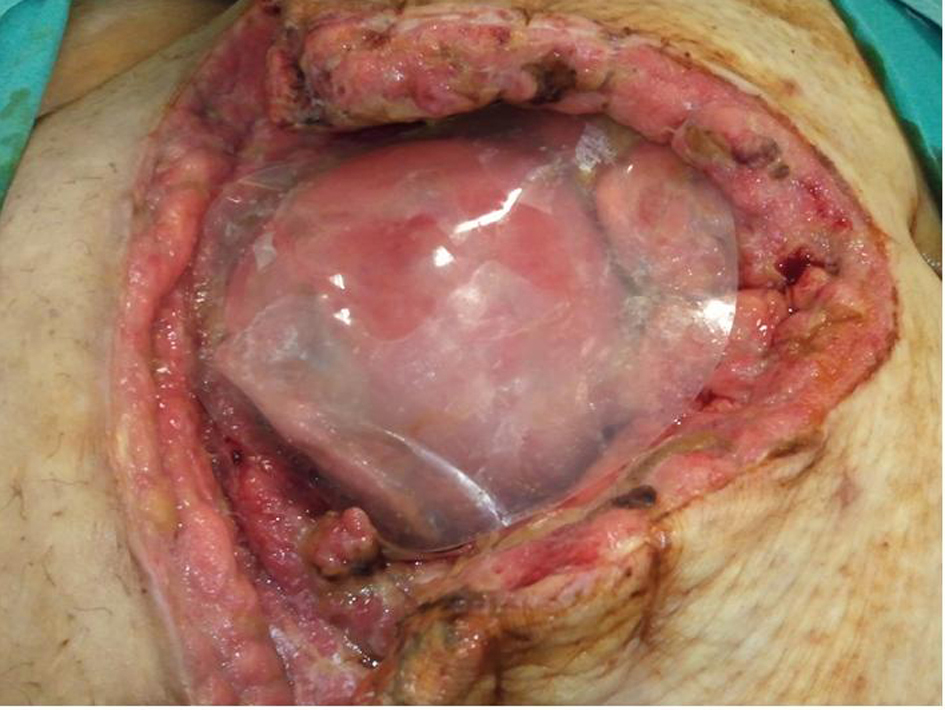
A 45 years-old nulligravid woman was admitted with the complaints of hypermenorrhea and menorrhagia. In her pelvic and sonographic examinations a myomatous uterus of 8 × 7 × 6 cm in size was detected. Total abdominal hysterectomy was planned with the indications of leiomyoma and abnormal uterine bleeding. From her medical history it was learned that she had diabetes mellitus (DM), hyperlipidemia (HL) and coronary artery disease and was not using any mediation for any of these diseases. Her laboratory examination was as follows: hemoglobin: 14.4 g/dl, hematocrit: 42.4%, white blood cell count: 7500/ml, platelets: 250,000 /ml, glucose: 130 mg/dl, blood urea nitrogen: 30 mg/dl, creatinine: 0.8 mg/dl, ALT: 19 IU/L, AST: 19 IU/L, sodium: 135.7 mmol/L, potassium: 4.76 mmol/L. Her coagulation parameters were within the normal limits. A serous leakage from her skin incision was detected in the 5th postoperative day. Antibiotic treatment of gentamycin 3 × 80 mg and clindamycin 3 × 900 mg was initiated. In the 6th postoperative day leakage from the incision started to become purulent and foul smelling. A specimen was sent to microbiology for culture; in which 10 days after the results reported proteus microbialis. In the 6th postoperative day between the incision and the umbilicus, 10 cm from the incision at two different regions, skin necrosis and hyperemic demarcation lines of 2 × 2 cm in sizes on the skin were detected and immediately the patient was operated with a general surgeon. In the operation during exploration it was seen that the infection did not spread into intra-peritoneal cavity. Widespread necrosis, bullous formations, small subcutaneous abscesses and wide supurative infected lesion with foul smelling was seen. The patient was diagnosed to have necrotizing fasciitis and skin, subcutaneous tissues, and fascia were excised widely (Fig. 1). The specimen was sent to pathologic examination and reported to be necrotic exudate, abscess formation, pannunculitis adipose tissue. After wide excision the intestines were packaged with Bogota bag so that the abdomen was left open because of the possibility of development of compartment syndrome (Fig. 2). Metronidazole 3 × 500 mg and piperacilline - tazobactam 4 × 4.5 g were initiated postoperatively. The wound was dressed daily. In postoperative 11th day the retention sutures were cut and the Bogota bag was changed. Necrotic regions were excised again and the skin and the subcutaneous tissues were sutured so that in the middle 2 to 3 cm region was left open (Fig. 3). In the same day in order to shorten the healing process and to get rid of the leakage from the wound, with an apparatus that generates negative pressure debris and the pus of the wound was tried to be collected but after two days because of patient discomfort this procedure was terminated. In postoperative 26th day Bogota bag was taken out and dehiscence was present only in a small part of the wound. Antibiotic treatment and wound dressing were continued for 25 days. In postoperative 35th day the wound was almost closed and the patient was discharged from the hospital with the recommendation of continuing wound dressing at home. During her follow-ups after 10 days from the discharge, the wound was found to be healed completely. In the postoperative 5th month the patient was still surviving a normal life.
 Click for large image | Figure 1. Debridement of the necrotic tissue, skin, subcutaneous tissue and fascia. |
 Click for large image | Figure 2. Application of Bogota Bag after wide debridement. |
 Click for large image | Figure 3. Abdominal incision that could be partly closed on postoperative 11th day. |
| Discussion | ▴Top |
Necrotizing fasciitis is a pathology caused by anaerobic bacteria alone or more commonly in combination with aerobic bacteria. It has a high mortality and morbidity rate if not treated early [3]. It is very rare and involves skin, subcutaneous tissue and fascia and typically does not involve the muscle layer. It progresses rapidly and causes necrosis. It is necessary to differentiate this infection from gas gangrene which is caused by Clostridium perfringens. The bacteria that are commonly seen in necrotizing fasciitis that develops after hysterectomy may be variable. In 90% of the cases beta hemolytic streptococci, and coagulase positive staphylococci alone or in combination are seen. In 10% of the cases the etiologic agents are gram negative enteric pathogens [4].
Although more commonly seen in lower extremities, groin regions, perineum and abdominal wall, necrotizing fasciitis can be seen in other parts of the body [3]. Surgery of any kind or trauma may precipitate the process. Any trauma that interferes with skin integrity, small incisions, burns, injections, animal bites and blunt traumas may all play a predisposal factor [5]. In literature there are cases of necrotizing fasciitis that was caused by S. Aureus after injection [6]. In the present case after hysterectomy a soft tissue infection without gas formation that started in the incision line and spread to skin, subcutaneous tissues and fascias was presented.
Diabetes mellitus, hypertension, cirrhosis, obesity, immune suppression, malignancy, chronic diseases, advanced age (> 50), malnutrition, peripheral vascular disease, alcoholism, chemotherapy corticotherapy, radiotherapy, Cushing disease are all risk factors for necrotizing fasciitis. In literature there are cases of necrotizing fasciitis that developed after hysterectomies without any risk factors [7-10]. In the present case diabetes mellitus, hypertension, coronary artery disease and obesity were the risk factors.
Clinical signs are primarily important in the diagnosis of necrotizing fasciitis. A seroangineous discharge with foul smelling, presence of necrotic fascia in gray color should remind this infection. Microbiologic culture and gram staining studies should be carried out. In addition in cases where needed, the definitive diagnosis can be made with radiologic studies such as computed tomography or magnetic resonance imaging or surgical exploration [8, 10, 11]. The diagnosis was confirmed with culture of the exudate and surgical exploration in the present case.
Mortality is high in necrotizing fasciitis; may be as high as 76% in cases without appropriate treatment [12]. Early diagnosis, wide surgical excision, administration of wide spectrum systemic antibiotics until culture results are obtained, are all important in the treatment. Excisions can be repeated and the wound must be left open. A 24-hour delay in surgical treatment may result in 35 to 40% increase in the mortality rate [13]. Fluid and electrolyte balance must be provided and patient must be followed-up for anemia and thrombocytopenia.
In this case surgical excision was done and the wound was left open. Debridement was continued with wound dressing daily. Antibiotic treatment was continued until systemic signs ceased. Fluid and electrolyte balance was provided and the patient was discharged from the hospital after 35 days with cure.
In conclusion care must be given to antisepsis in order to prevent development of the disease, appropriate prophylactic antibiotics must be administrated when needed, foreign material must be carried out during the operation, disease must be diagnosed early and appropriate medical and surgical treatment must be initiated.
| References | ▴Top |
- Umbert IJ, Winkelmann RK, Oliver GF, Peters MS. Necrotizing fasciitis: a clinical, microbiologic, and histopathologic study of 14 patients. J Am Acad Dermatol. 1989;20(5 Pt 1):774-781.
pubmed doi - Riseman JA, Zamboni WA, Curtis A, Graham DR, Konrad HR, Ross DS. Hyperbaric oxygen therapy for necrotizing fasciitis reduces mortality and the need for debridements. Surgery. 1990;108(5):847-850.
pubmed - Hacıbektaşoğlu A. Gazlı gangrene ve diğer anaerob deri ve yumuşak doku enfeksiyonları. Topçu A, Söyletir G, Doğanay M. İnfeksiyon hastalıkları. Nobel Tıp Kitapevleri Ltd. Şti. 1996, 790-794.
- Leoper DJ, Al Hadi S. Cerrahi enfeksiyonlar. In: İskender Sayek. Temel Cerrahi 1991, 149.
- Stevens DL. Invasive group A streptococcus infections. Clin Infect Dis. 1992;14(1):2-11.
pubmed doi - Regev A, Weinberger M, Fishman M, Samra Z, Pitlik SD. Necrotizing fasciitis caused by Staphylococcus aureus. Eur J Clin Microbiol Infect Dis. 1998;17(2):101-103.
pubmed - Martinez Velasco IG, Plascencia Valadez V, Salinas Trevino J, Sanchez Gutierrez J, Tirado Saldivar A. [Post-cesarean necrotizing fasciitis. Bacterial synergism, or mixed infection of the soft tissues?]. Ginecol Obstet Mex. 1996;64:58-63.
pubmed - Goepfert AR, Guinn DA, Andrews WW, Hauth JC. Necrotizing fasciitis after cesarean delivery. Obstet Gynecol. 1997;89(3):409-412.
pubmed doi - Mathews MS, Raman A, Nair A. Nosocomial zygomycotic post-surgical necrotizing fasciitis in a healthy adult caused by Apophysomyces elegans in south India. J Med Vet Mycol. 1997;35(1):61-63.
pubmed doi - Tarlan N, Demirkol T, Bakır Ç. Sezaryen sonrası gelişen nekrotizan fasiitis olgu sunumu. Klinik Bilimler Doktor 2001, 7:261-3.
- Çelik Ç, Baba A, Çiçek N, Dikici N, Çapar M, Akyürek C. Bir olgu sunumu nekrotizan fasciitis. Klinik Bilimler Doktor 2001, 7:860-3.
- Hackett SP, Stevens DL. Superantigens associated with staphylococcal and streptococcal toxic shock syndrome are potent inducers of tumor necrosis factor-beta synthesis. J Infect Dis. 1993;168(1):232-235.
pubmed doi - Lille ST, Sato TT, Engrav LH, Foy H, Jurkovich GJ. Necrotizing soft tissue infections: obstacles in diagnosis. J Am Coll Surg. 1996;182(1):7-11.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
