| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 5, Number 2, June 2016, pages 74-76
Maternal Heart Rate Mistaken for the Fetal Heart Rate During Delivery
Shunji Suzukia, b, Yuuri Sensua, Mayumi Uedaa
aDepartment of Obstetrics and Gynecology, Japanese Red Cross Katsushika Maternity Hospital, Tokyo, Japan
bCorresponding Author: Shunji Suzuki, Department of Obstetrics and Gynecology, Japanese Red Cross Katsushika Maternity Hospital, 5-11-12 Tateishi, Katsushika-ku, Tokyo 124-0012, Japan
Manuscript accepted for publication April 14, 2016
Short title: Maternal Heart Rate Mistaken for Fetal’s
doi: http://dx.doi.org/10.14740/jcgo402e
| Abstract | ▴Top |
Misidentification of fetal and maternal heart rate is not an acceptable mistake. We present here a case of maternal heart rate mistaken for the fetal heart rate during delivery in our hospital. In this case, the neonatal short outcomes were very poor contrary to the prediction based on the findings of heart rate tracings.
Keywords: Maternal heart rate; Fetal heart rate; Misidentification
| Introduction | ▴Top |
Misidentification of fetal and maternal heart rate is not an acceptable mistake. We present here a case of maternal heart rate mistaken for the fetal heart rate during delivery in our hospital.
| Case Report | ▴Top |
A 28-year-old woman, gravida 1, para 0, whose antenatal care had been uneventful, was admitted to our hospital with the onset of labor pains at 37 weeks’ gestation. At admission, her heart rate was 88 bpm.
During the first stage of delivery, fetal heart rate tracings showed reassuring patterns as shown in Figure 1A. The baseline of the fetal heart rate was 130 - 140 bpm.
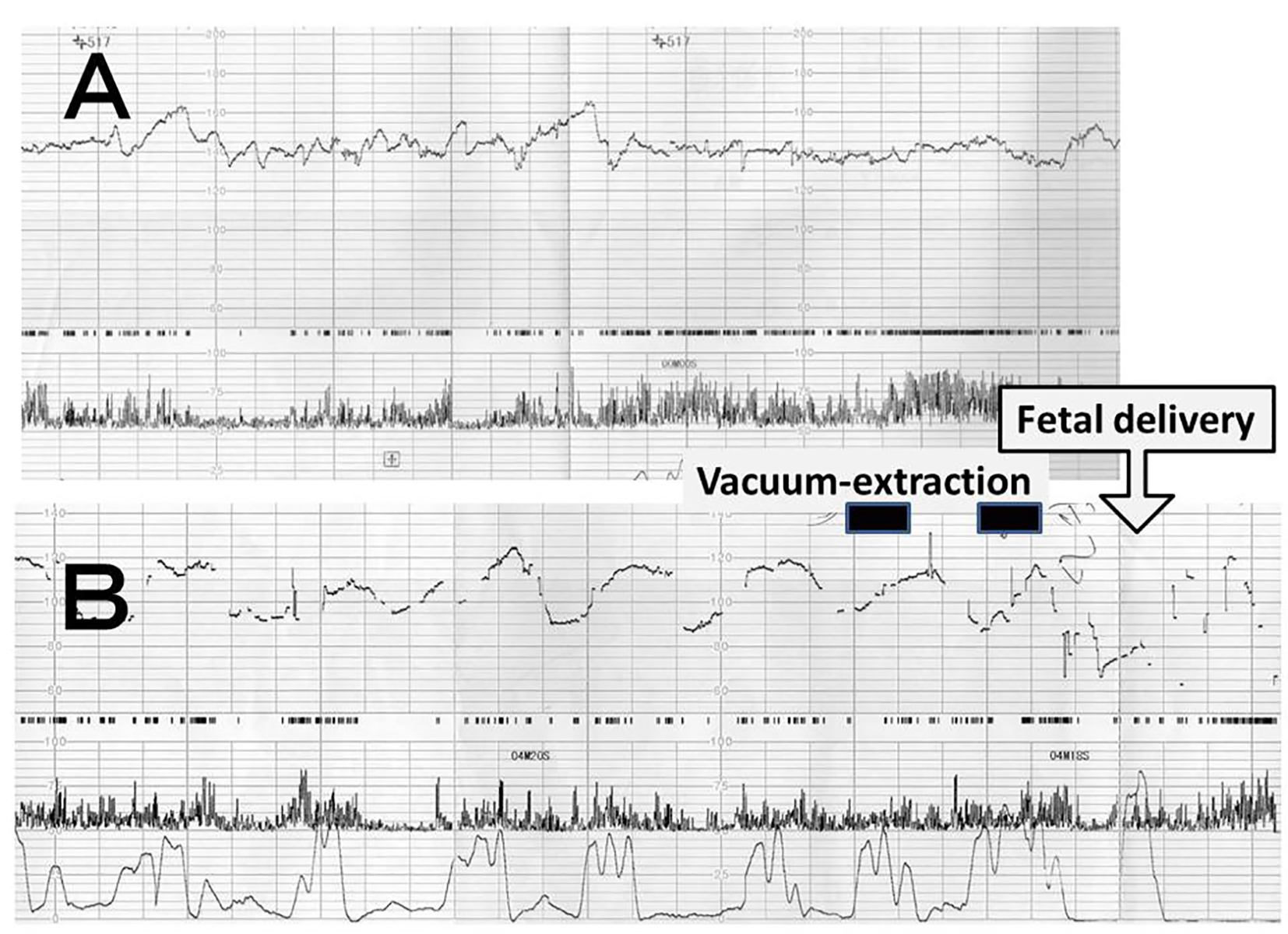 Click for large image | Figure 1. (A) Fetal heart rate tracings showing reassuring patterns during the first stage of delivery at 37 weeks’ gestation and (B) heart rate tracings showing the baseline of 110 - 120 bpm with variability and the presence of recurrent mild variable decelerations. Closed squares show the periods of vacuum-extraction. |
She was transported to the delivery room when the cervix was fully dilated. During the second stage of delivery, fetal heart rate tracings seemed to be the baseline of 110 - 120 bpm with variability and the presence of recurrent mild variable decelerations as shown in Figure 1B. Vacuum-extraction was selected due to the occiput posterior position of the fetal head. During the two-time extractions shown with the closed squares in Figure 1B, the heart rate increased to 110 bpm. The neonate was a male weighing 2,696 g (appropriate for gestational age) with heart rate of less than 100 bpm and no spontaneous respiration requiring neonatal cardiopulmonary resuscitation with artificial respiration. The umbilical arterial pH was 6.776. After the fetal delivery, the heart beats were able to be detected at the same position of the maternal abdomen.
The neonate was admitted to the neonatal intensive care unit due to the respiratory and circulatory distress. Fortunately, he has now grown to a healthy boy of 1.5 years old without any problems.
| Discussion | ▴Top |
In the current case, the neonatal short outcomes were very poor contrary to the prediction based on the findings of fetal heart rate tracings. In this case, the same heart beats were able to be detected at the same position after the fetal delivery. Therefore, the recorded heart beats were estimated to be derived from the mother. During the delivery, the baseline of maternal heart rate usually increases because her sympathetic is stimulated by anxiety and labor pains and cardiac output increases associated with the increased venous return. In addition, it further increases at the time of uterine contraction during the second stage of delivery, while it returns during the intermittent periods of uterine contraction [1, 2]. On the other hand, the fetal heart rate bradycardia caused by the negative pressure of the vacuum apparatus associated with the reflection of the vagus nerve stimulation which returns to normal after instrument disconnection is usually observed during vacuum-extraction [3]. In this case, the increased heart rate from 80 - 90 to 120 bpm was observed during vacuum-extraction in the fetal heart rate tracings. In this case, therefore, the maternal heart beats might be mistaken for the fetal heart beats.
Figure 2 shows the heart rate tracings of our recent case that we recorded both fetal (the open arrow) and maternal heart rates (the closed arrow) during the normal delivery at 39 weeks’ gestation. As shown in these figures, the maternal heart rate sometimes increases to the levels of fetal heart rate during the second stage of delivery. In such cases, it may be difficult to distinguish fetal heart rates from maternal heart rates.
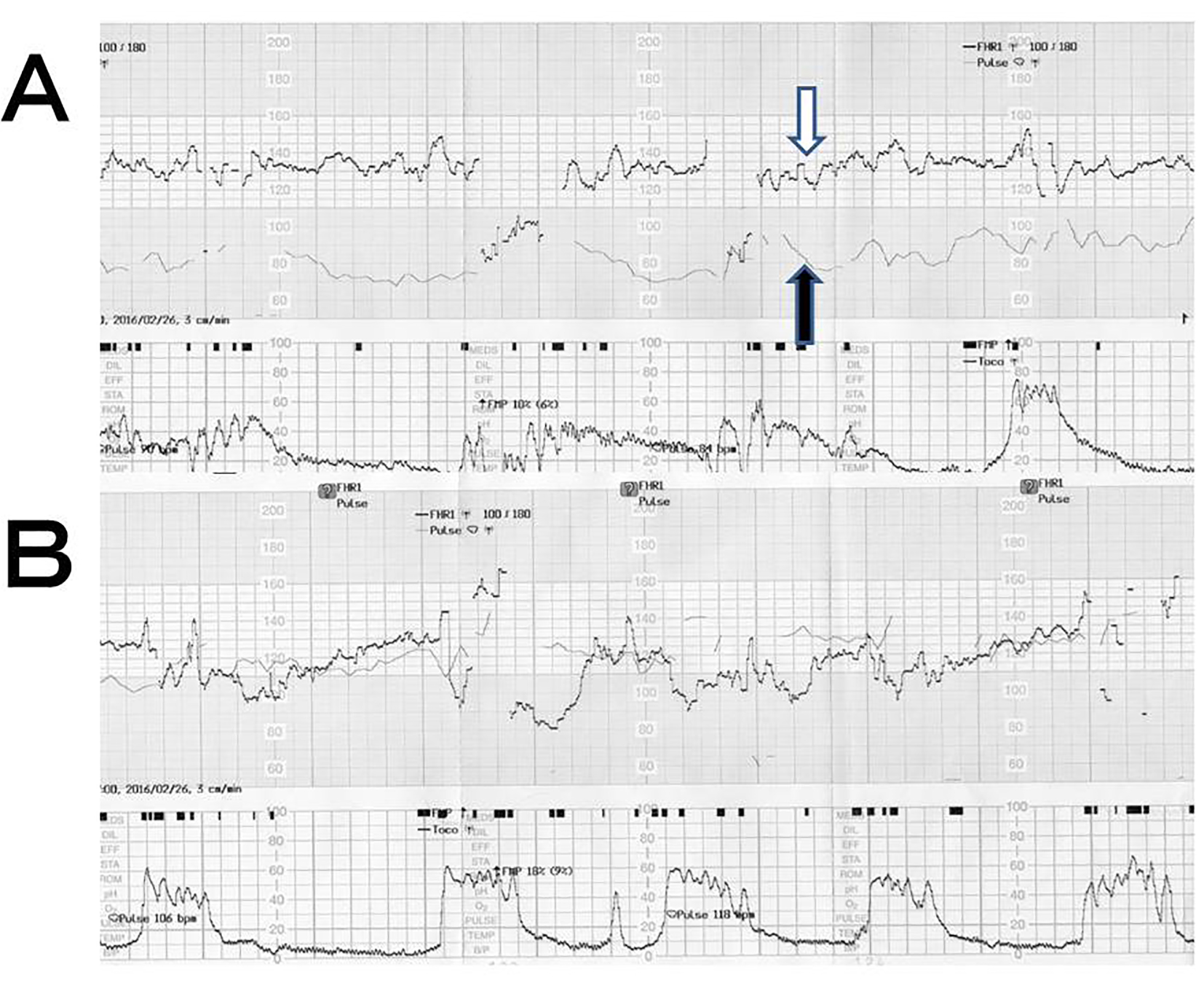 Click for large image | Figure 2. Fetal and maternal heart rate tracings during (A) first stage and (B) second stage of normal delivery at 39 weeks’ gestation. Open arrow shows the fetal heart rate, while closed arrow shows the maternal heart rate. |
Conclusion
To prevent these rudimentary mistakes, the discrimination of fetal and maternal heart beats should be borne in mind during labor.
Grant Support
This study received no funding.
Conflicts of Interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
| References | ▴Top |
- Sherman DJ, Frenkel E, Kurzweil Y, Padua A, Arieli S, Bahar M. Characteristics of maternal heart rate patterns during labor and delivery. Obstet Gynecol. 2002;99(4):542-547.
doi - Sohnchen N, Melzer K, Tejada BM, Jastrow-Meyer N, Othenin-Girard V, Irion O, Boulvain M, et al. Maternal heart rate changes during labour. Eur J Obstet Gynecol Reprod Biol. 2011;158(2):173-178.
doi pubmed - Apuzzio JJ, Pelosi MA, Ganesh VV. Fetal heart bradycardia associated with the vacuum extractor. A case report. J Reprod Med. 1984;29(7):496-497.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
