| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Original Article
Volume 5, Number 3, September 2016, pages 77-80
Fertility History: Assessment of Performance and Quality Improvement
Karim Abdallaha, b, David J. Walkera
aRoyal United Hospitals Bath NHS Foundation Trust, Obstetrics & Gynaecology Department, Royal United Hospital, Combe Park, Bath, BA1 3NG, UK
bCorresponding Author: Karim Abdallah, Royal United Hospitals Bath NHS Foundation Trust, Obstetrics & Gynaecology Department, Royal United Hospital, Combe Park, Bath, BA1 3NG, UK
Manuscript accepted for publication August 25, 2016
Short title: Fertility History
doi: http://dx.doi.org/10.14740/jcgo411w
| Abstract | ▴Top |
Background: Many fertility clinics use their own standard history sheet. Currently, no standard history sheet is in use in our unit. This audit project aimed at assessing the quality of the history obtained from couples with sub-fertility without using a standard history sheet followed by designing and introducing a standardized history sheet and re-auditing the quality of the history obtained to assess if introducing a standardized history sheet into our unit will improve the quality of the service provided.
Methods: We started by designing a standardized history sheet which is simple, non-time consuming and contains all the basic information required at that very early stage of managing couples with sub-fertility. Data were collected from 50 notes retrospectively where we made sure that the notes included were for patients seen by different registrars at their first consultation. The standardized sheet was then introduced and all doctors were asked to use it for history taking during the first consultation with new couples seen in the clinic. Data were then collected from 50 notes where the standardized sheet was used.
Results: The quality of the history taken at the first consultation is inconsistent and variable. The quality may be improved if a simple form of standard history sheet is used by all doctors doing the fertility clinic.
Conclusion: History taking is a fundamental step in the management of sub-fertile couples. Couples complaining of sub-fertility will have their history taken during their first consultation at the reproductive medicine clinic. As the gynecology trainees running the clinic can be alternating, the quality of the history taken from these patients can vary. Obtaining accurate and complete information will help in making the management of those patients a smoother process with reducing the number of consultations and increasing patient satisfaction.
Keywords: Fertility; History; Standard
| Introduction | ▴Top |
Prevalence of sub-fertility is on the rise. One couple of every seven couples in the UK struggle with fertility problems and seek medical advice [1]. The management of couples with sub-fertility poses a challenge to healthcare professionals. Couples with sub-fertility are commonly anxious and stressed with the possible magnitude of their complaint and find it hard to go through the process of waiting for their consultation with fertility specialists with the subsequent waiting for results of investigations until finally formulating the necessary management plans.
As any other medical complaint, management of couples with sub-fertility starts with taking the relevant history from both partners. Hence, a defective history will impact on the waiting times until a management plan is formulated.
Because smaller fertility clinics are often run by doctors who may not necessarily be fertility experts, the history taking process may not be standardized, leading to defective and missing information. This will undoubtedly delay the management plans with subsequent increase in the number of consultations and waiting times.
Aim, objectives and standards
The audit aimed at assessment of the quality of the history taken from couples with sub-fertility during their first consultation at our fertility clinic. Many fertility clinics use a standard template for history taking during the first consultation with their patients. However, as that was not available at our unit we started by designing a simple and easy to follow history sheet that we used as the standard for conducting this audit. The history sheet was based on the necessary essential information that we need to know about couples with sub-fertility as outlined in the NICE guidance for management of couples with sub-fertility and was approved by the consultants running the fertility clinic.
| Methodology | ▴Top |
The audit was performed over a period of 12 weeks during which 50 patients’ case notes were reviewed. The data were collected and assessed against the newly designed standard history sheet. Care was taken to ensure that the reviewed case notes were for patients who were seen by a range of clinicians during their first consultation. Following data collection, the standard history sheet was introduced to the clinic and doctors were asked to use it for their first consultations with patients for a period of 12 weeks. Data were then collected and re-audited to close the loop and assess if introducing a standard history sheet will actually improve the quality of the taken history from patients at their first consultation.
| Results | ▴Top |
Table 1 shows the necessary questions included in the standard history sheet for the female partners and the number of patients who were asked those questions before and after the introduction of the standard sheet.
 Click to view | Table 1. The Standard Questions Included in the History Sheet and the Percentage of Female Patients Who Were Asked Those Questions Before and After the Introduction of the Standard Sheet |
Table 2 shows the necessary questions included in the standard history sheet for the male partners and the number of patients who were asked those questions before and after the introduction of the standard sheet.
 Click to view | Table 2. The Standard Questions Included in the History Sheet and the Percentage of Male Patients Who Were Asked Those Questions Before and After the Introduction of the Standard Sheet |
The audit showed that history taking during the first encounter with the patients at our unit was inconsistent and variable. That is thought to be directly related to the fact that patients do not necessarily get seen by the same doctors. In most of the cases, patients were asked the most important questions like menstrual history and history related to smoking and alcohol consumption. On the other hand, questions related to sexual dysfunctions, recreational drugs and family history seem to be missed by most doctors with less than 10% (Figs. 1 and 2) of patients asked those questions. None of the patients included in the audit was asked about her vaccination history. Rubella infection during pregnancy is associated with increased risk of fetal malformations and neonatal morbidity. It is recommended to advice women to get vaccinated against Rubella infection before pregnancy and to avoid getting pregnant during the first 3 months following the vaccination [2].
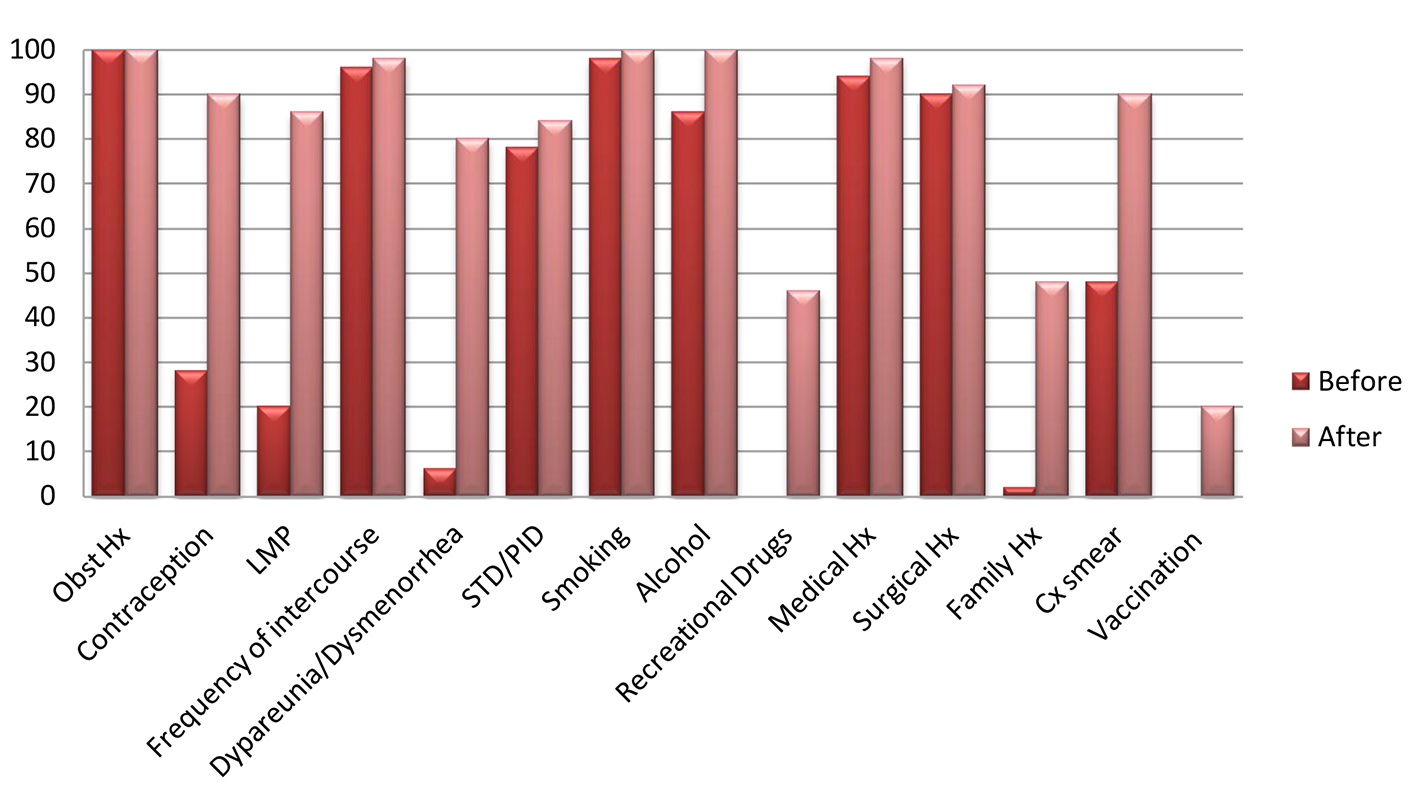 Click for large image | Figure 1. Transverse axis shows the necessary questions included in the standard history sheet for the female partners. Longitudinal axis shows the percentage of patients who were asked those questions before and after the introduction of the standard sheet. |
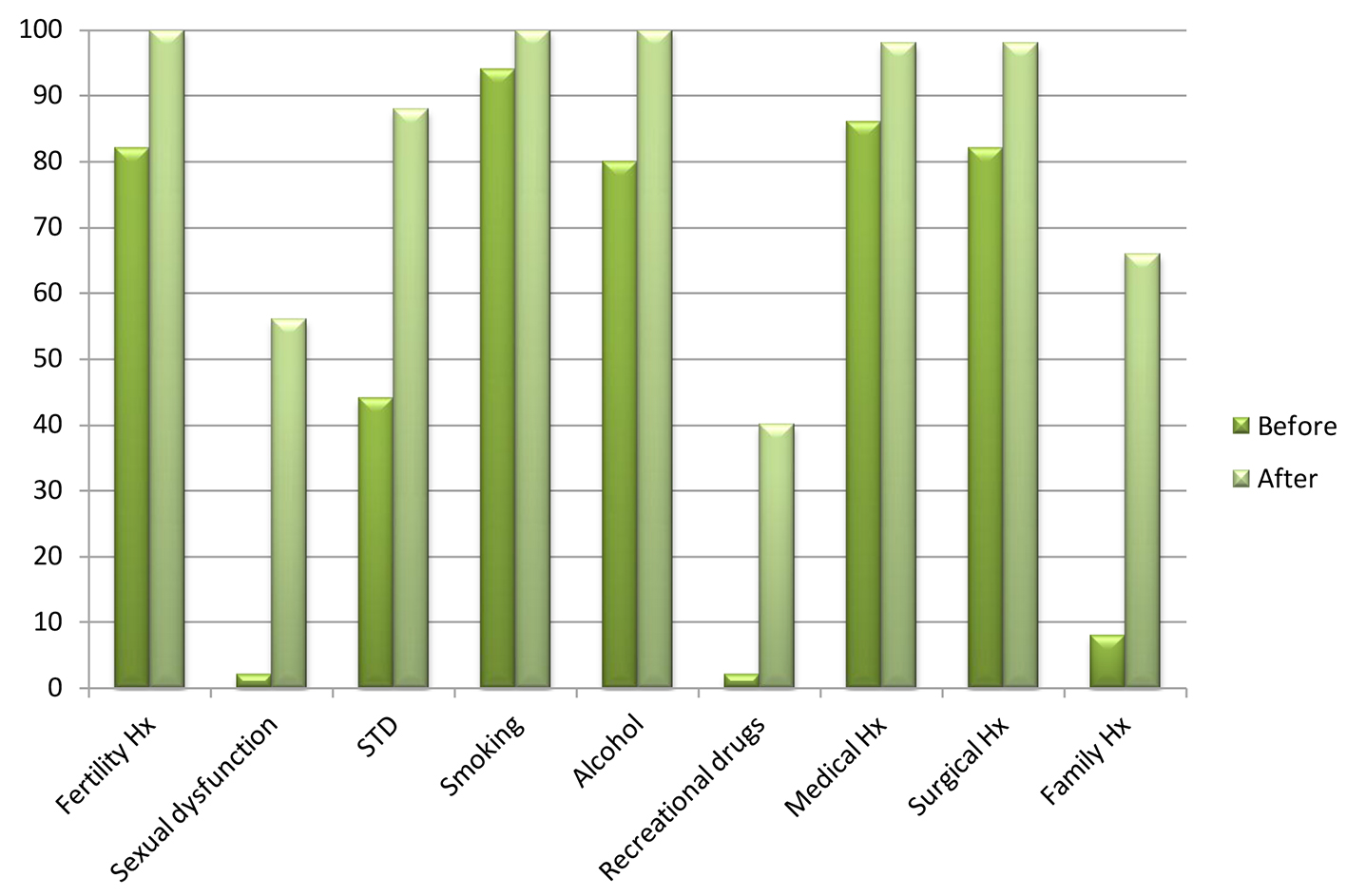 Click for large image | Figure 2. Transverse axis shows the necessary questions included in the standard history sheet for the male partners. Longitudinal axis shows the percentage of patients who were asked those questions before and after the introduction of the standard sheet. |
| Discussion | ▴Top |
Obstetric history (parity and mode of previous deliveries) helps to define the type of sub-fertility (primary/secondary) which is essential for treatment funding issues. All patients were asked about their obstetric history at the outset of the audit (Fig. 1). Contraceptive history gains its importance from the fact that some contraceptive measures are associated with delayed return of fertility (Depo injections) [3]. The percent of patients asked about their contraceptive history improved from 28% to 90% using the standard history sheet (Fig. 1). Menstrual history including regularity of the cycles and presence/absence of dysmenorrhea is essential for identifying underlying conditions such as endometriosis and PCOS [4]. The recommended frequency of intercourse is 2 - 3 times weekly especially around the expected time of ovulation, hence, the significance of asking about the frequency of sexual intercourse and presence or absence of sexual dysfunction [2]. Smoking, alcohol and using recreational drugs are known to reduce fertility for both males and females [2]. Also, smoking couples will not be granted funding for assisted reproduction (IVF/ICSI) if one or both partners have been smoking in the last 6 months before starting treatment [5]. Women are advised to be vaccinated against Rubella infection before embarking on a pregnancy and to delay pregnancy for at least 3 months following vaccination against rubella infection [2].
The couple needs to be asked about any history of sexually transmitted diseases or pelvic infections to assess tubal factors (vas deferens obstruction in males) of sub-fertility [6]. This has gone up from 78% to 84% for women (Fig. 1) and from 44% to 88% for men (Fig. 2) following the introduction of the standard sheet.
The overall finding of the audit was that history taking was undoubtedly inconsistent and the amount of information included was variable among doctors. The introduction of a standard history sheet has significantly improved the quality of the service we provide in our unit.
Recommendations
A copy of the standard history sheet will be added to the patient’s notes for the purpose of history taking during their first consultation.
The quality of the history taken will be assessed at 12 monthly intervals and the standard sheet will be modified as required.
| References | ▴Top |
- (1)NHS.uk. http://www.nhs.uk/chq/Pages/889.aspx?CategoryID=54.
- NICE Guidance February 2013; Assessment and treatment for people with fertility problems.
- NICE Guidance October 2005; Long Acting Reversible Contraception.
- RCOG Greentop guideline number 24; Endometriosis, investigation and management. October, 2006.
- (2)NHS.uk. http://www.nhs.uk/conditions/Infertility/Pages/Introduction.aspx.
- Stamatios Karavolos, Jane Stewart, Isaac Evbuomwan, Kevin McEleny, Ian Aird. TOG. 2013;15:1-9.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
