| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 5, Number 4, December 2016, pages 129-130
Laparoscopic Cerclage in a Patient of Cervical Incompetence
Sonali Tawdea, b, Himanshu Bavishia, Falguni Bavishia, Parth Bavishia
aBavishi Fertility Institute, Next to Adani CNG & Gajarawala Flats, Paldi Cross Roads, Paldi, Ahmedabad-7, Gujarat, India
bCorresponding Author: Sonali Tawde, B wing, 202, Asha Nagar, Phase 2, Nirmal Group, Near Saidham Mandir, P.K. Road, Mulund West, Mumbai 400080, Maharashtra, India
Manuscript accepted for publication November 04, 2016
Short title: Laparoscopic Cerclage
doi: https://doi.org/10.14740/jcgo415w
| Abstract | ▴Top |
Cervical incompetence may be due to obstetric or gynecological or congenital causes. The laparoscopic cerclage is highly recommended for previous failed vaginal cerclage and is superior to laparotomy approach in terms of low morbidity and faster recovery. In this case report, we tried to evaluate obstetric outcome of preconceptional laparoscopic cerclage in a patient of cervical incompetence. A 31-year-old lady presented with primary infertility. She had two first-trimester and two second-trimester abortions. Vaginal cerclage was done in subsequent pregnancy by MacDonald’s method, which failed to prolong pregnancy. Hence, preconceptional laparoscopic cerclage was done with Mersilene tape. Main outcome was neonatal survival and prolongation of gestation. The lady successfully completed 36 weeks and delivered a baby weighing 2.94 kg, by elective LSCS without any complications. Preconceptional laparoscopic cerclage proved to be safe and effective, resulting in favorable obstetric outcome in this lady having cervical incompetence and bad obstetric history.
Keywords: Cervical; Abortion; Incompetence; Laparoscopic; Cerclage
| Introduction | ▴Top |
Cervical incompetence is known to occur in 1% of all pregnancies, and recur in 30% of cases. It typically presents in second trimester of pregnancy as pelvic pressure and painless cervical dilatation in the absence of uterine activity. Cervical incompetence is a complex phenomenon with multiple underlying etiologies. It can be due to previous obstetric or gynecological trauma, congenital weakness or shortness. Cerclage can be done vaginally, which is conventional surgery, or abdominally, which can be either laparoscopic or laparotomy approach.
Transabdominal approach was first described by Benson and Durfee in 1965, and indication was extended by Novy in 1982, for failed vaginal cerclage in previous pregnancy.
| Case Report | ▴Top |
The aim of this case study was to evaluate obstetric outcome of preconceptional laparoscopic cerclage in a patient of cervical incompetence. A 31-year-old lady, married since 14 years, presented with primary infertility. She was obese with typical signs and symptoms of polycystic ovarian syndrome. She conceived four times, with IVF-ICSI treatment. In her first pregnancy, she had single gestation, but aborted at 16 weeks. Second time she conceived, it was twin gestation, but resulted in missed abortion at 8 weeks. In her third pregnancy, MacDonald’s vaginal cerclage was done at 13 weeks i/v/o previous h/o second trimester miscarriage and transvaginal scan suggestive of short cervix. NT scan and dual marker test were done and confirmed normal before cerclage. She was advised rest, tocolytics, but in spite of all the precautions, she aborted at 18 - 19 weeks. The fourth pregnancy was a blighted ovum at 7 weeks.
Pre-pregnancy laparoscopic cerclage was planned for her i/v/o failed vaginal cerclage with cervical incompetence and bad obstetric history. Meresilene tape was introduced, 1.5 cm superior and 1 cm lateral to insertion of uterosacral ligaments, medial to uterine vessels and ureter (Fig. 1). The tape was fixed to anterior aspect of cervix, intracorporeal six knots were taken (Fig. 2), and ends of the knot were secured with 2-0 vicryl. Then closure of uterovesical fold was done. The posterior aspect of tape, in UV fold was confirmed (Fig. 3). Intraoperative blood loss was very minimal, and patient was discharged next day.
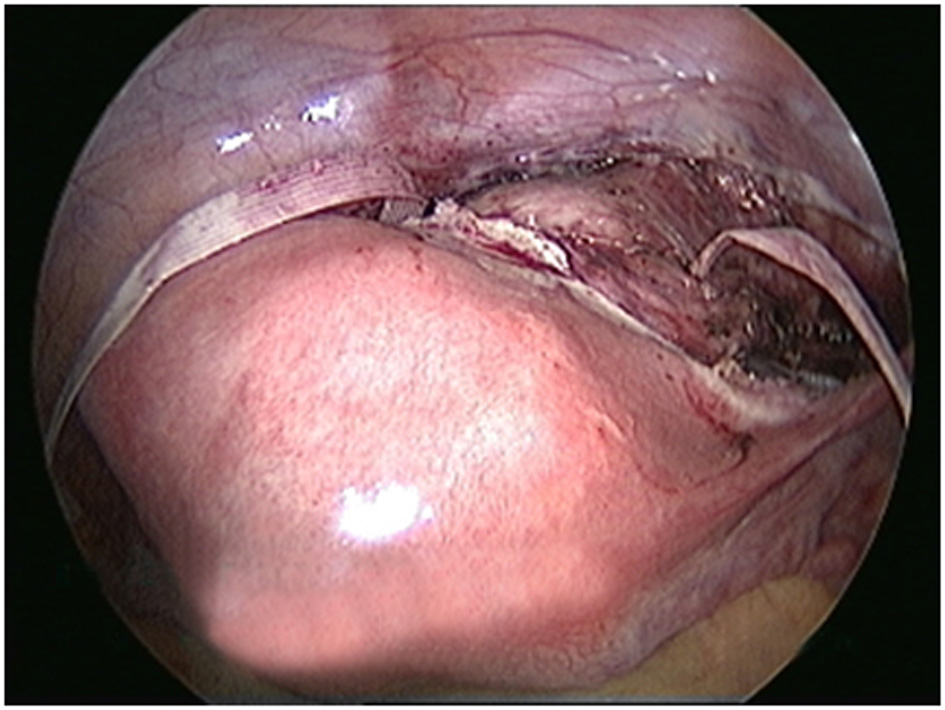 Click for large image | Figure 1. The site of insertion of Mersilene tape. |
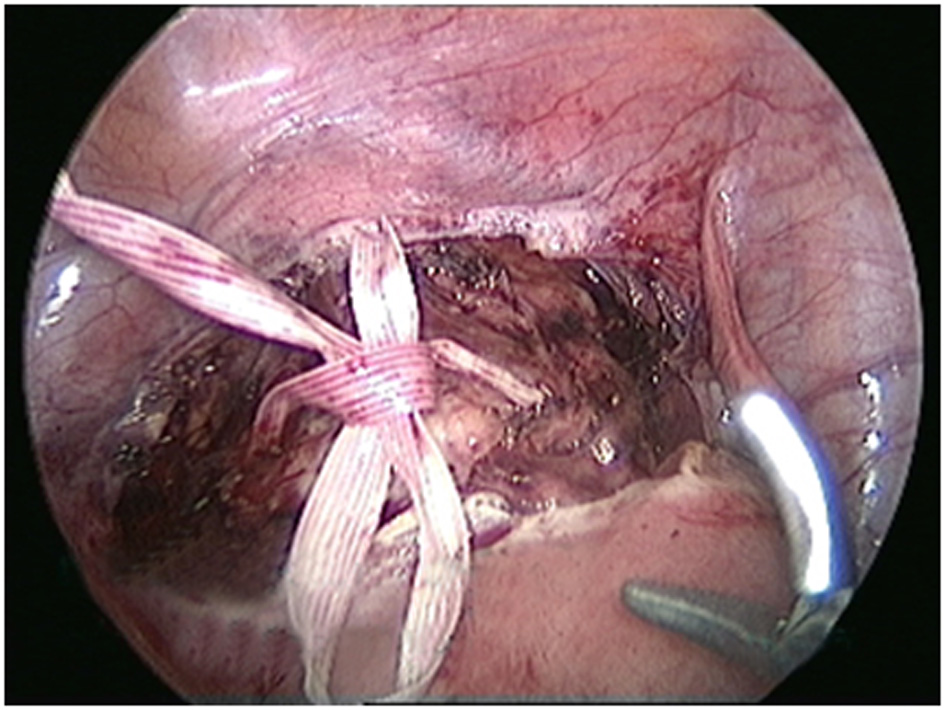 Click for large image | Figure 2. Intracorporeal knot tying. |
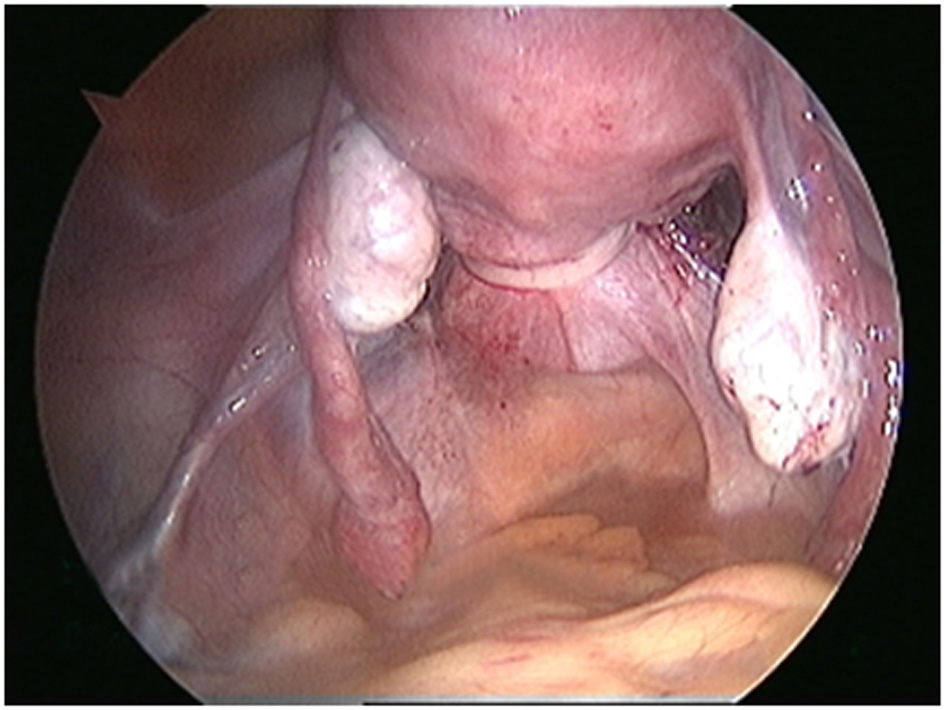 Click for large image | Figure 3. Posterior aspect of tape, UV fold. |
Main outcome of prolongation of pregnancy and neonatal survival was to be assessed. She conceived in next IVF-ICSI cycle again. In this pregnancy, her antenatal period was uneventful, and she successfully completed 36 weeks of gestation. She delivered, by elective cesarean section, a baby with birth weight of 2.94 kg without any intraoperative or postoperative complications. The tape was left in situ, and precaution was taken to mark lower segment horizontal incision slightly above the usual site, so that the tape was not disturbed, as the lady was interested in future fertility.
| Discussion | ▴Top |
With proper selection of patients and good operative skills, preconceptional cerclage proved safe and effective, resulting in favorable obstetric outcome in this patient with cervical incompetence and bad obstetric history. Laproscopic approach favors comparably with traditional laparotomy approach and should be integrated in clinical practice whenever possible [1]. Preconceptional cerclage is more practical.
Advantages of this procedure are less morbidity, faster recovery, being anatomically more accurate, no foreign body in vagina which can act as nidus for infection, reduced incidence of premature rupture of membranes, being possible in patients with cervico-vaginal fistulas, and less incidence of slippage and adhesions. Firm nature of non-pregnant cervix helps surgeon to avoid injury to adjacent vessels.
The disadvantages are laparoscopy is a major procedure as compared to vaginal cerclage, and also one needs a cesarean section after cerclage. Failure of laparoscopic cerclage and chorioamnionitis occurred more often when placed during pregnancy. But timing of cerclage does not influence the gestational age at delivery.
Most comprehensive systematic review of literature by Burger and coworkers [2] compared 135 laparoscopy procedures with 1116 transabdominal cerclage procedures. They concluded that interval laparoscopy approach is better than one performed during pregnancy. Ades et al [3] in one of the most recent studies (April 15) found that the perinatal survival was 95.8% with mean gestational age at delivery of 35.8 weeks, and 83% women delivered > 34 weeks gestation. He has performed 150 laparoscopic cerclage procedures with 12 being done during pregnancy and 138 before pregnancy, and most pregnancies were uneventful. In a study by Luo et al [4], they compared laproscopic vs. vaginal cerclage and observed that fetal salvage rate was 92.3% and no adverse effects were encountered. Mean gestational age in laparoscopy group was 36.4 weeks and it was 17.4 weeks longer than their previous pregnancy age, significantly higher than obtained by vaginal cerclage.
Vaginal cerclage is being done for those at risk of preterm labor or in those with short cervix on USG, but there are various theories and supportive studies, indicating its role in only selective group of patients and not in all. The laparoscopic preconceptional cerclage holds promise for patients of cervical incompetence, especially when vaginal cerclage fails to prolong pregnancy. Skilled surgeon and right selection of patients are the key to this noble procedure. We need controlled trials for this surgery to support its role in large number of patients before coming to definitive conclusion, but it is surely a promising step in this era of keyhole surgeries.
| References | ▴Top |
- Wendy I, Whittle Sukhbir Singh, Lisa Allen. Laparoscopic cervicoisthmic circlage. AM J Obstet Gynaecol. 2009.
- Burger NB, Brolmann HA,Einarsson Ji. Effctiveness of abdominal circlage placed via laparoscopy or laparotomy, systematic review. J Minim Invasive Gynaecol. 2011.
- Alex Ades, Kim C, Dobromilsky. Transabdominal Cervical Circlage, Laproscopy Vs. Laparotomy. J Minim Invasive Gynaecol. 2015.
- Lu Luo, Shugin Chen, Hongye Jiang. Eur J Obstet Gynaecol Reprod Biol. 2014.
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
