| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 6, Number 3-4, October 2017, pages 75-78
Tubal Migration of Intrauterine Device: A Report of a Rare Case of Trauma-Induced Migration Leading to Acute Abdomen
Dominique A. Badra, d, Saadia M. Cheikhb, Jihad M. Al Hassanb, Mohamad K. Ramadana, c
aDepartment of Obstetrics and Gynecology, Lebanese University, Beirut, Lebanon
bDepartment of Obstetrics and Gynecology, Zahraa University Hospital, Beirut, Lebanon
cDepartment of Obstetrics and Gynecology, Makassed General Hospital, Beirut, Lebanon
dCorresponding Author: Dominique A. Badr, OBGYN Department, Lebanese University, Beirut, Lebanon
Manuscript submitted June 20, 2017, accepted August 21, 2017
Short title: Trauma-Induced Tubal Migration of IUD
doi: https://doi.org/10.14740/jcgo453w
| Abstract | ▴Top |
Intrauterine devices (IUDs) are the most commonly used reversible contraceptive methods. They are a highly effective and safe tool of contraception but might carry some uncommon complications including device migration. Trauma-induced trans-tubal migration has not been reported before. We encountered a 26-year-old woman who presented to the emergency department (ED) with left iliac fossa pain, 1 day following a fall-down trauma. She had a history of uneventful IUD insertion 3 months prior to presentation. In the ED, a standing KUB showed an extra-uterine intra-abdominal IUD. At laparoscopy, the IUD was found protruding through the isthmic part of the fallopian tube. Trauma to patients wearing IUDs should prompt fellow gynecologists to check the location of the device within 24 - 48 h. Recognition of this rare yet serious complication can be of benefit in the differential diagnosis of patients presenting to the ED with acute abdomen.
Keywords: Intrauterine device; Tubal migration; Acute abdomen; Laparoscopy
| Introduction | ▴Top |
Intrauterine device (IUD) is a highly effective method of reversible contraception [1]. Although it carries an acceptable safety record, some complications may arise during its insertion or its long-term use. Intra-abdominal IUD migration following uterine perforation at insertion is a rare complication [2]. Spontaneous trans-tubal migration is even rarer. This type of migration was not reported following trauma. Herein, we report a case of trans-tubal migration of a copper T380A IUD and perforation of the tubal isthmus following a fall-down trauma.
| Case Report | ▴Top |
A 26-year-old G3P3A0L3 previously healthy woman presented to the emergency department (ED) because of moderate left iliac fossa pain, 1 day following a fall-down of the stairs. The pain was not associated with nausea, vomiting, vaginal bleeding or any other symptom. On physical examination, her vital signs were within normal ranges, and her abdomen was soft and non-distended. A localized left iliac fossa tenderness was noted without rebound tenderness. Vaginal examination was not performed. Basic laboratory tests showed normal urine analysis and hemogram. Pregnancy test was negative. Facing this clinical picture, the ED physician elected to perform a standing KUB that showed an IUD in the left iliac fossa (Fig. 1). The patient was then asked about the history of the IUD insertion. She stated that a copper IUD was inserted 3 months earlier by a trained gynecologist, 4 weeks postpartum. At routine follow-up 1 month post-insertion, a pelvic ultrasound showed properly placed IUD. After initial assessment in the ED, the patient was transferred to our service. CT scan of the pelvis with intravenous and oral contrast was done and confirmed the presence of the IUD in the left adnexa (Fig. 2). During diagnostic laparoscopy, we found that the IUD had perforated the left fallopian tube at the level of its isthmus creating an acute inflammatory response and adhesions of the omentum around it (Fig. 3). The gross appearance of the tube was otherwise normal, and no hydro- or pyosalpinx was seen. Using monopolar electrocautery, we lysed the adhesions and removed the IUD. The tubal perforation was left open. The patient was discharged on day 1 postoperatively. She was seen 1 month later in the clinic and her physical examination was unremarkable.
 Click for large image | Figure 1. Abdominal X-ray showing the intrauterine device in the left iliac fossa (white arrow). |
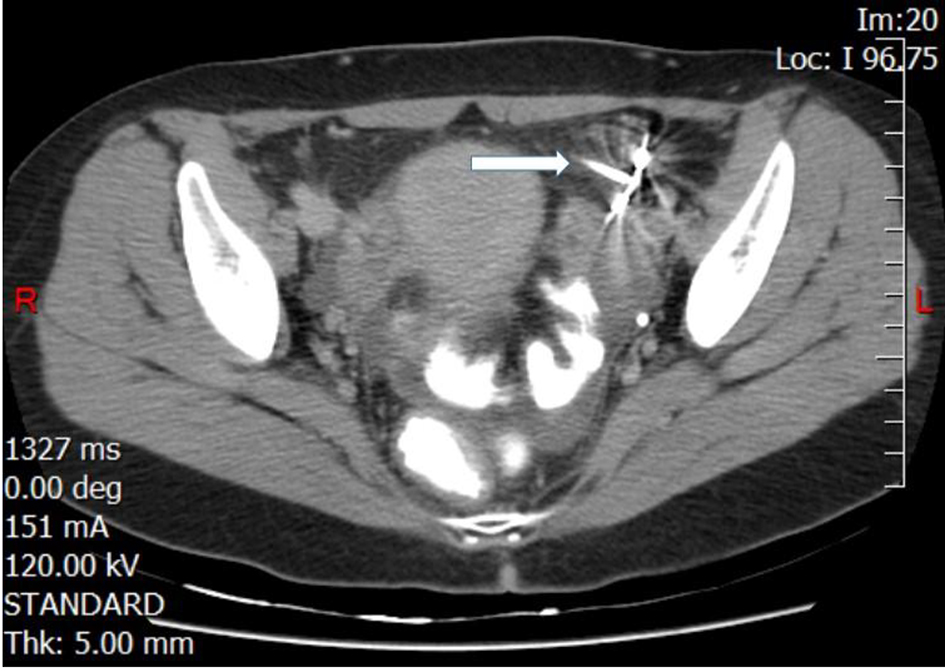 Click for large image | Figure 2. CT scan of the pelvis with intravenous and oral contrast localizing the intrauterine device in the left adnexa (white arrow). |
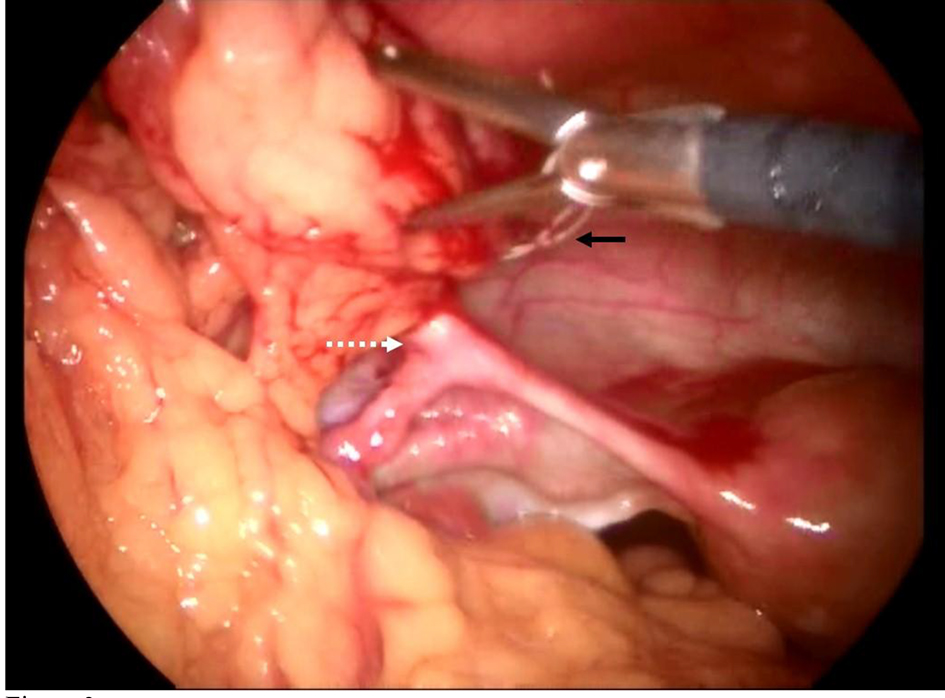 Click for large image | Figure 3. Laparoscopic view of the intra-abdominal IUD. The IUD perforates the isthmus of the left fallopian tube (white dashed arrow) creating adhesions of the omentum around it. The IUD thread is shown behind the laparoscopic clamp (black rigid arrow). |
| Discussion | ▴Top |
Contraceptive methods are widely used by female patients for birth control. No single method can suit all women. Age, personal history, socio-economic status and other factors play an important role in the selection of the most suitable contraceptive tool. Among others, IUD is an effective non-surgical long-acting reversible contraceptive method with a pregnancy rate of less than 1 in 100 women per year [1]. Although it is highly safe, it may lead to some undesirable side effects ranging from menorrhagia, infection, expulsion, to the rare faulty insertion leading to uterine perforation [3].
Uterine perforation following IUD insertion is rare and accounts for 0.1% of cases [2, 4]. The perforation may be either complete if the IUD was found outside the uterus or partial when only a part of it has penetrated the myometrium. Following complete perforation, the IUD can migrate to different intra-abdominal structures such as the omentum, bowels, peritoneal cavity and bladder among others. Presenting signs and symptoms include missing thread, abnormal uterine bleeding, abdominal pain and pregnancy [5].
Instead of directly perforating the myometrium, the IUD can rarely reach the abdominal cavity after migrating via the fallopian tubes [3, 6-11].
We conducted a literature search on MEDLINE database between 1976 and 2017 for articles reporting similar cases. All articles published with English abstracts were included. The search terms were: “intrauterine device” AND “trans-tubal migration”. The lists of references of these articles were also reviewed. In total we could find seven [3, 6-11] cases of trans-tubal IUD migration (Table 1), and none was due to trauma.
 Click to view | Table 1. Characteristics of the Seven Cases of Trans-Tubal Migration of Intrauterine Device Found in Literature Since 1976 |
After reviewing the text of the aforementioned cases, we could not identify a common pattern related to the timing, method of insertion or the type of IUD. The exact mechanism of spontaneous trans-tubal migration remains obscure. Previous studies assumed that either the IUD was placed in the uterine cornua close to the tubal ostium at the time of insertion [9], or it was displaced toward the ostium due to the profound involution of the myometrium during the postpartum and lactation period [2]. However, in our patient the migration was not spontaneous. The IUD was in place as shown on pelvic ultrasound during routine follow-up, 1 month post-insertion. The single inciting event preceding migration was the trauma sustained 1 day before presenting to the ED.
Following trauma, it is wise to check the IUD location during the first 24 - 48 h in women wearing IUDs, even if they are asymptomatic. Imaging studies are the cornerstone in patients with a missed IUD thread. A simple abdominal X-ray can easily discern expulsion from migration. An ultrasound, CT scan or MRI of the abdomen and pelvis can then map the exact location of the migrating IUD and identify any associated visceral complication [12].
When an IUD is found in the abdominal cavity, whether to remove it or not is controversial, especially if the patient is asymptomatic [13]. It would, however, be desirable to remove it because of the high incidence of adhesions’ formation that can afflict permanent infertility, possible visceral injury and subsequent acute abdominal pain if left in place. Laparoscopy can be used as a first-line treatment even in the presence of adhesions or visceral injury [14]. In two out of the seven cases reviewed, laparoscopy was used to remove the IUD but the chronicity of migration and the tubal infection resulted in tubal sacrifice in both patients. In our case, the tube was minimally harmed and tubal preservation was feasible after securing good hemostasis.
The IUD remains one of the safest and highly effective methods of contraception even if some complications occur during its use. Intra-abdominal IUD migration via the fallopian is an extremely rare complication. Trauma-induced trans-tubal migration was not reported before. Hence, it is advisable to check the IUD location in patients using this method of contraception, in the first 24 - 48 h following trauma.
Funding
No source of financial support was obtained for the report.
| References | ▴Top |
- Mansour D, Inki P, Gemzell-Danielsson K. Efficacy of contraceptive methods: A review of the literature. Eur J Contracept Reprod Health Care. 2010;15(1):4-16.
doi pubmed - Caliskan E, Ozturk N, Dilbaz BO, Dilbaz S. Analysis of risk factors associated with uterine perforation by intrauterine devices. Eur J Contracept Reprod Health Care. 2003;8(3):150-155.
doi pubmed - Nde-Ouedraogo NA, Tiemtore-Kambou BM, Ouattara B, Diallo O, Cisse R. Aspects radiographiques et echographiques d’une migration tubaire d’un dispositif intra uterin/Radiographic and ultrasonographics aspects of an intra-uterine device tubal migration. International Journal of Innovation and Applied Studies. 2016;18(3):904.
- Kaislasuo J, Suhonen S, Gissler M, Lahteenmaki P, Heikinheimo O. Intrauterine contraception: incidence and factors associated with uterine perforation--a population-based study. Hum Reprod. 2012;27(9):2658-2663.
doi pubmed - Kaislasuo J, Suhonen S, Gissler M, Lahteenmaki P, Heikinheimo O. Uterine perforation caused by intrauterine devices: clinical course and treatment. Hum Reprod. 2013;28(6):1546-1551.
doi pubmed - Gunaratne M. Tubal migration of a Lippes loop with subsequent intrauterine pregnancy. Contraception. 1976;14(3):285-289.
doi - Kim DS, Hwang YY, Kang KC, Park MI. Migration of the Lippes loop into the fallopian tube. Obstet Gynecol. 1982;60(3):393-394.
pubmed - Wikland M, Wilhelmsson L. A rare case of IUD expulsion through the fallopian tube. Acta Obstet Gynecol Scand. 1983;62(2):191-192.
doi pubmed - Sindos M, Pisal N, Setchell M, Singer A. Tubal migration: a rare complication of an intrauterine contraceptive device leading to formation of a hydrosalpinx. Am J Obstet Gynecol. 2003;188(4):1109-1110.
doi pubmed - Ozdemir S, Cihangir N, Gorkemli H, Emlik D. Pyosalpinx caused by the tubal migration of an intrauterine device--a case report. Eur J Contracept Reprod Health Care. 2008;13(3):320-322.
doi pubmed - Bharathi RS, Chakladar A, Kumari P. Mystery of the missing loop. Med J Armed Forces India. 2011;67(2):177-178.
doi - Boortz HE, Margolis DJ, Ragavendra N, Patel MK, Kadell BM. Migration of intrauterine devices: radiologic findings and implications for patient care. Radiographics. 2012;32(2):335-352.
doi pubmed - Markovitch O, Klein Z, Gidoni Y, Holzinger M, Beyth Y. Extrauterine mislocated IUD: is surgical removal mandatory? Contraception. 2002;66(2):105-108.
doi - Gill RS, Mok D, Hudson M, Shi X, Birch DW, Karmali S. Laparoscopic removal of an intra-abdominal intrauterine device: case and systematic review. Contraception. 2012;85(1):15-18.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
