| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 7, Number 3-4, November 2018, pages 76-80
Preservation of Six Renal Arteries in Laparoscopic Para-Aortic Lymphadenectomy: A Case Report
Tsuyoshi Kondoa, b, Hiromasa Sasakia, Kohshiro Nakaoa, Shinya Hirabukia, Tsutomu Hoshibaa
aDepartment of Obstetrics and Gynecology, Ishikawa Prefectural Central Hospital, 2-1, Kuratsukihigashi, Kanazawa, Ishikawa 920-8530, Japan
bCorresponding Author: Tsuyoshi Kondo, Department of Obstetrics and Gynecology, Ishikawa Prefectural Central Hospital, 2-1, Kuratsukihigashi, Kanazawa, Ishikawa 920-8530, Japan
Manuscript submitted July 19, 2018, accepted October 5, 2018
Short title: Six Renal Arteries in Laparoscopy
doi: https://doi.org/10.14740/jcgo505w
| Abstract | ▴Top |
The presence of more than one renal artery has been commonly observed, and approximately 10% - 40% of examined cadavers have an accessory renal artery, which corresponds to each segmental artery. Thus, it is important to preserve these arteries during para-aortic lymphadenectomy via laparotomy. Here, we present a case involving a patient with ovarian cancer who underwent laparoscopic para-aortic lymphadenectomy with preservation of six renal arteries. Although two left renal arteries were observed through contrast CT, surgical findings revealed two right and four left renal arteries, including blood vessels, which were not identified preoperatively. Moreover, a subtype of the left renal vein was present. In previous reports on gynecological laparoscopic surgery, the maximum number of accessory renal arteries was two, which is a common finding. With regard to en bloc removal in laparoscopic para-aortic lymphadenectomy with renal vascular abnormalities, it is recommended to reduce the lymph nodes to the minimum size necessary to avoid tumor scattering, renovascular injury, and surgical field failure. Furthermore, it is difficult to diagnose renovascular abnormalities using only contrast CT preoperatively. Thus, in laparoscopic surgery, whereby the viewing direction of the operative field is fixed, the procedure should be performed with due consideration of the renovascular abnormalities.
Keywords: Accessory renal artery; Para-aortic lymphadenectomy; Laparoscopy
| Introduction | ▴Top |
The kidney is divided into five segments, namely, the apical, upper, middle, lower, and posterior segments. Each segmental artery supplies its corresponding segment of the kidney [1]. The presence of more than one renal artery has been commonly observed, and approximately 10-40% of examined cadavers have accessory renal arteries, which did not degenerate in the course of disease development [2]. Despite it being just an accessory renal artery, it corresponds to each segmental artery without anastomosis; thus, due caution should be observed when performing para-aortic lymphadenectomy via laparotomy to preserve these arteries [3]. In gynecological laparoscopic surgeries, the highest number of accessory renal arteries found upon examination was two, and there were no cases showing a greater number. Here, we report a case of laparoscopic para-aortic lymphadenectomy with preservation of six renal arteries and left renal vein subtypes.
| Case Report | ▴Top |
A 66-year-old Japanese female patient (gravidity 2, parity 2, age at menopause: 50 years) presented to our hospital with a chief complaint of abdominal distension. She underwent abdominal contrast CT, and iodine contrast agent allergy was noted. After additional examinations, she was diagnosed to have stage IIIC ovarian cancer. Four cycles of neoadjuvant chemotherapy were administered. After the chemotherapy, an interval debulking surgery was performed through laparoscopy as per patient’s request. Two left renal arteries were recognized during the initial contrast-enhanced CT, but because of iodine contrast agent allergy, no evaluation was performed by 3D CT angiography (3D-CTA) prior to surgery (Figs. 1, 2).
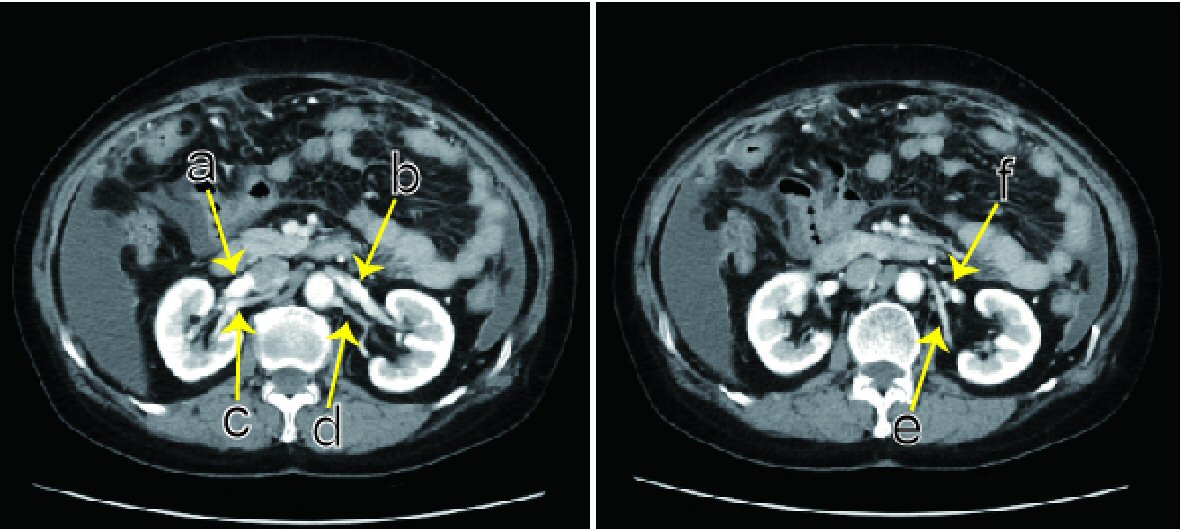 Click for large image | Figure 1. Abdominal contrast CT. Preoperatively, two left renal arteries are present (d, e). (a) Right renal vein. (b) The vein from the left kidney goes over an abdominal aorta, connecting at the point right before the abdominal aorta. (c) Right main renal artery. (d) Left main renal artery diverges to the apical and upper segmental arteries. (e) Left posterior segmental artery. (f) The left ovarian vein flows into the left renal vein. |
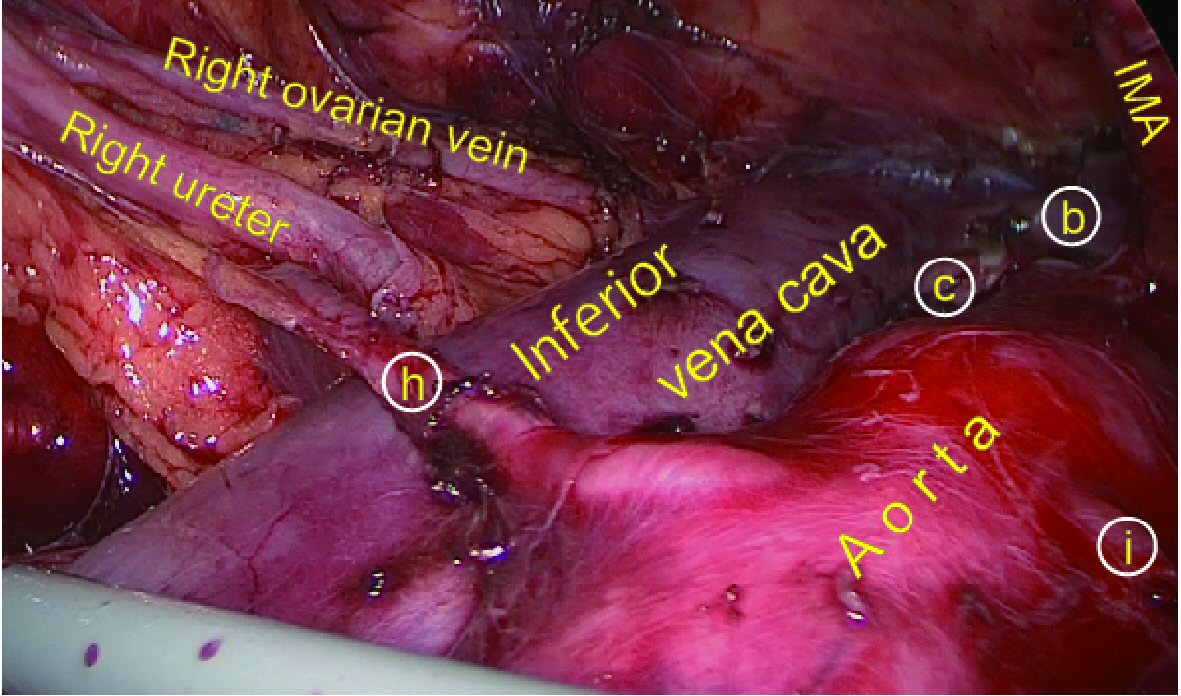
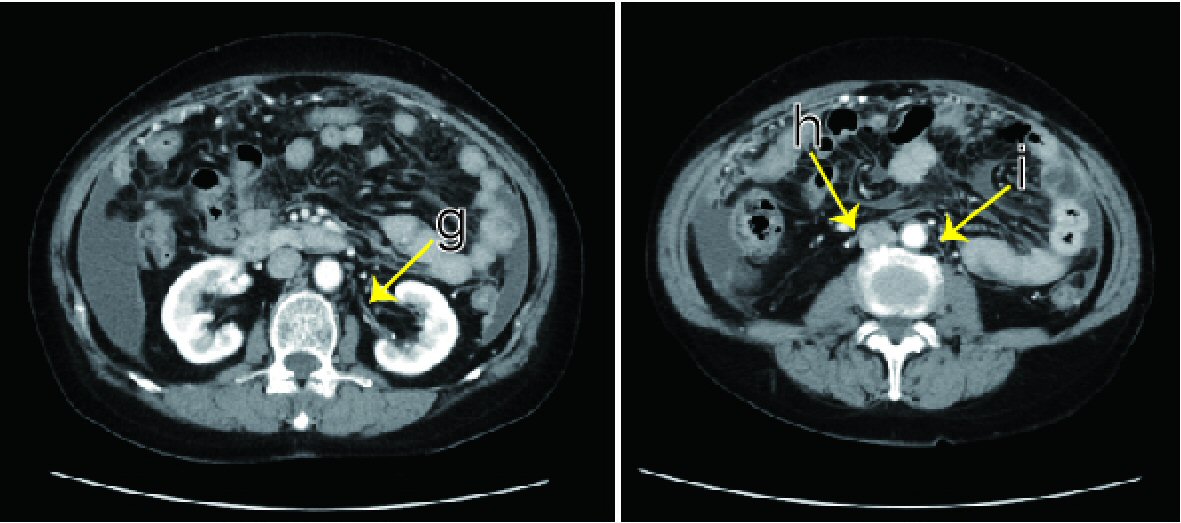 Click for large image | Figure 2. Abdominal contrast CT. The left middle segmental artery (g) and bilateral lower segmental artery (h, i) were not recognized preoperatively. The right lower segmental artery (h) goes over the front of the inferior vena cava. |
Surgical findings
The total intraoperative blood loss was 350 g (including lymph fluid), without blood transfusion requirement.
Although slight traces of peritoneal dissemination were observed, the uterine and ovarian structure appeared normal macroscopically. Para-aortic lymphadenectomy was performed under retroperitoneal endoscopy. There was no lymph node enlargement. Lymph nodes, including the vessel sheath and connective tissue, were carefully peeled from the blood vessel using suction and release forceps. After ensuring the absence of an accessory renal artery between the separated lymph node and blood vessels, the process of cutting with monopolar and a sealing device was finely repeated. In contrast with the normal anatomy (Fig. 3), it was confirmed that the four left and two right renal arteries were derived from the trunk of the aorta, including blood vessels that could not be identified prior to the surgery. In the first artery from the caudal side, the bilateral lower segmental artery was derived from the middle part of the aortic bifurcation and inferior mesenteric artery (IMA), and the right lower artery passes through the anterior surface of the inferior vena cava to the right lower pole. In the second left renal artery, the left middle segmental artery was derived from the abdominal aorta at the same height as the IMA. In the third and fourth arteries, the left main renal artery and left posterior segmental artery were derived just below the left renal vein. The right main renal artery was located on the dorsal side of the inferior vena cava at its normal position.
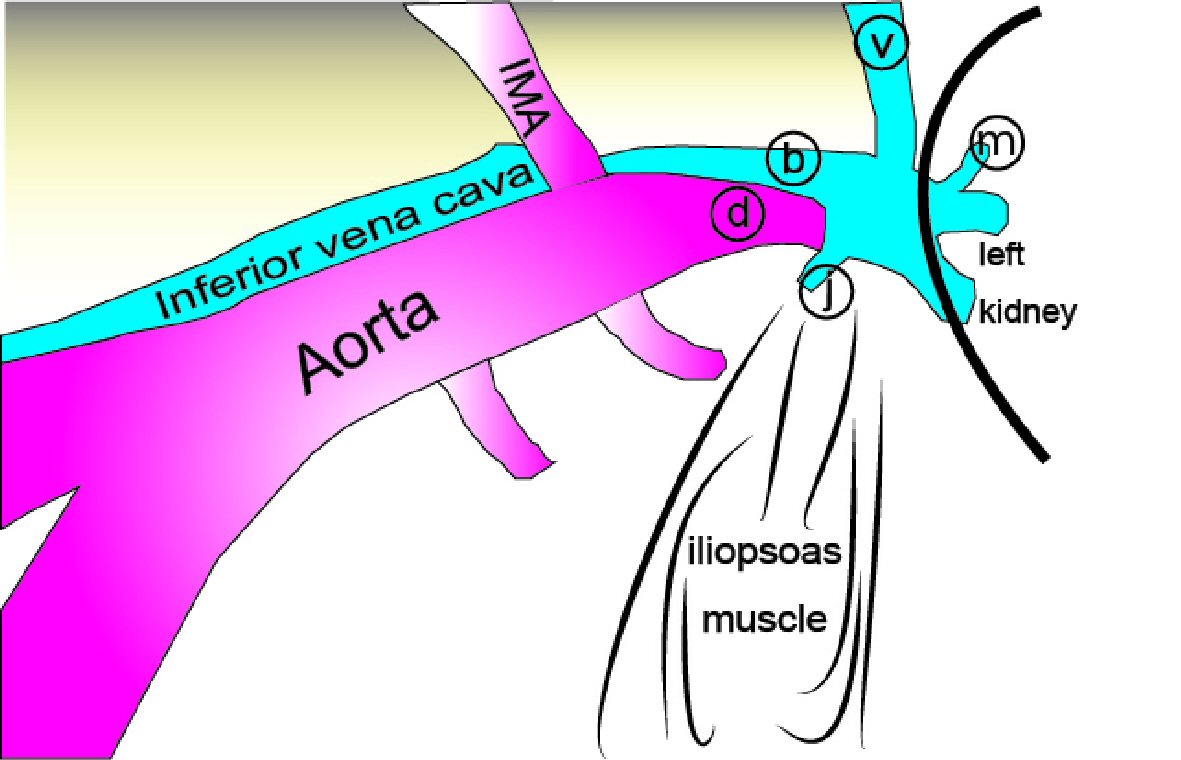 Click for large image | Figure 3. Normal anatomy under retroperitoneal endoscopy (left para-aortic lymphadenectomy). The left ovarian (v) and lumbar (j) veins flow into the left renal vein (b) and go over the aorta. Usually, it cannot be confirmed with the presence of fat tissues, but the left adrenal vein (m) also flows into the left renal vein. During surgery, the left ovarian vein, inferior mesenteric artery (IMA), and ureter are pushed up to the ventral side. (d) Left renal artery. |
The left renal vein was also found to be atypical, and three veins from the left kidney did not connect at the hilus renalis, the left ovarian vein flows through the middle vein, and the lumbar vein flows into the caudal vein. A cephalic vein densely fused with a central vein, forming the left renal vein truncus, and a caudal vein fused with it at the point right before it went over the aorta.
The left para-aortic lymph node was excluded from the en bloc resection, because the renal blood vessel structure was complicated. To prevent blood vessel damage during dissection, we divided the lumbar vein, which directs blood flow into the left renal vein, into two: the high and low para-aortic lymph nodes. We resected the right para-aortic lymph nodes while preserving all the renal arteries (Figs. 4, 5). Subsequently, laparoscopic pelvic lymphadenectomy, subtotal omentectomy, and peritoneal dissemination lesion biopsy were performed, followed by hysterectomy and bilateral oophorectomy, and optimal surgery was completed.
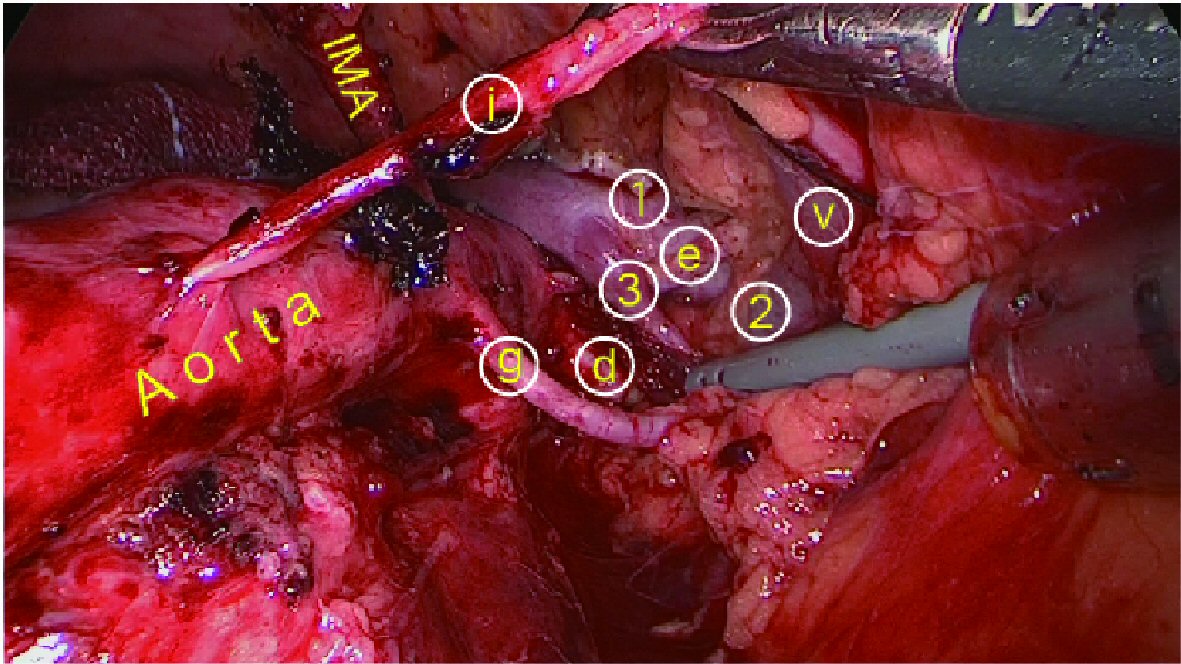 Click for large image | Figure 4. After left para-aortic lymphadenectomy under retroperitoneal endoscopy, three veins from the left kidney are present: (1) cephalic, (2) middle: a swollen left ovarian vein (v) flowing into the (3) caudal side (inflow lumbar vein cut). (d) Left main renal artery. (e) Left posterior segmental artery. (g) Left middle segmental artery. (i) Left lower segmental artery. |
 Click for large image | Figure 5. After right para-aortic lymphadenectomy under retroperitoneal endoscopy. (b) Left renal vein. (c) Right main renal artery. (h) Right lower segmental artery. (i) Left lower segmental artery. |
Postoperative course
The pathological diagnosis was ovarian cancer: serous adenocarcinoma (ypT3bN1M0). Among the 54 dissected lymph nodes, two right high para-aortic lymph nodes showed metastasis. There was no presence of postoperative micturition disorder and renal function degeneration. The patient underwent postoperative adjuvant chemotherapy for 1 year postoperatively, without any recurrence.
| Discussion | ▴Top |
In this report, as many as six renal arteries were found in a female patient; nevertheless, laparoscopic surgery was successfully performed. Moreover, it was difficult to diagnose all the vascular anomalies preoperatively; thus, surgery must be performed carefully by avoiding blind maneuvers.
When performing laparoscopic para-aortic lymphadenectomy for cases with complex renal vascular abnormalities, a retroperitoneal approach is employed to preserve the renal blood vessels and surgical fields. In left para-aortic lymphadenectomy, the ureter, left ovarian vein, and IMA are pushed toward the ventral peritoneum, and the lymph node is peeled and pressed to the dorsal side (Fig. 3). With the identification of the aorta and left renal vein by tracing the common iliac artery and left ovarian vein, the loose areolar tissues anterior to the vessel are separated or divided to expose the adventitia of the vessel. In the left para-aortic lymph node region surrounded by the abdominal aorta, left renal blood vessel, and iliopsoas muscle, only the lumbar artery, lumbar vein, and ovarian artery are likely to be operated on. However, the accessory renal artery in this case was the artery in each segment as shown on CT imaging. Apart from the accessory renal artery, which had not been identified preoperatively, the vein tracing the left ovarian vein was identified to be not a trunk of the left renal vein but a branch. The thickest branch was found on the cephalic side of the identified branch, which was observed on the caudal side; however, it was a blood vessel not normally observed. We have always operated on the vessel sheath without blind manipulation and have identified all unexpected renal vessels naturally in the process. Under general anatomical recognition, if vascular sheath treatment is performed only with a sealing device, renal vascular injury, massive hemorrhage, or renal infarction may occur. Renal blood vessels could be identified, but to ensure blood vessel preservation, lymph node collection, and a successful operative field, it is necessary to divide the high and low para-aortic lymph nodes into two, deferring the en bloc removal of the lymph nodes.
Renal vascular abnormalities are detected by MRI, contrast CT, 3D-CTA, and ultrasonography [4-6], but it is difficult to assess all the blood vessels preoperatively. In this case, we could not assess the three accessory renal arteries and the left renal vein subtype preoperatively due to the narrow vessel diameter, and the confluence site of the branch of the left renal vein was difficult to identify even after postoperative reexamination (Figs. 1, 2).
Renal artery and vein abnormalities differ in terms of the site of occurrence [2, 4, 5]. Nevertheless, both abnormalities may appear [7]. The anastomosis of the renal vein system including the inferior vena cava, results in the regression of the posterior cardinal, supracardinal and subcardinal veins. The left renal vein results from the anastomosis of the subcardinal vein, forming one vein, and the left adrenal, lower phrenic, left ovarian, and lumbar veins usually flow and go over the abdominal aorta [5] (Fig. 3). When diagnosing malformations of the renal venous system, it is considered necessary to perform angiography through left femoral vein puncture [5]. In this case, vein branches from the left kidney were not connected until the point right before the abdominal aorta, but the left renal vein trunk itself was only one. We considered the presence of an anastomotic subtype between the subcardinal veins.
Accessory renal arteries are derived from five segments of the kidney [2, 4], and there have been reports that up to 10 renal arteries have been recognized by angiography (eight accessory renal arteries) [8]. The rate of having four to five unidirectional renal arteries (three to four accessory renal arteries) is 0.2 to 2% [9], and this rarely occurs in Japanese women, as with the present case. The accessory renal artery becomes the segmental artery and may supply a more major area than the main renal artery [4]. The frequency of these cases varies between races and both sexes: it is 30% for Caucasians and Africans, but for Indians and Asians are in the 13.5-18.5% range. In men, the frequency is 28%, whereas in women, it is 16%, with rare occurrence in women of Asians [10]. Although the accessory renal artery is basically derived from the abdominal aorta [11], it is also derived from the renal artery itself [12] and rarely from the common iliac, external or internal iliac, hepatic, middle sacral, inferior phrenic, lumbar, pancreatic, and colonic arteries [11, 12]. The accessory renal arteries of the upper and lower poles of the kidney may be the base of the adrenal and gonadal arteries [2]. In the field of urology, the presence of an accessory renal artery is a matter of concern, but in gynecological laparoscopic surgery, it may be possible to encounter one or two maximum accessory renal arteries [7, 13, 14]. This report has the most common finding with four accessory renal arteries.
With regard to en bloc removal in laparoscopic para-aortic lymphadenectomy with renal vascular abnormalities, splitting the lymph nodes is required as necessary to minimize tumor scattering, renovascular injury, and surgical field failure, which is similar in laparotomy. In gynecological laparoscopic surgery, whereby preoperative diagnosis is difficult with contrast CT alone and the viewing direction of the operative field is fixed, blind operation should not be performed especially with the presence of renovascular abnormalities. Thus, with due consideration of these aspects, it is possible to perform laparoscopic surgery safely even in complicated cases without preoperative diagnosis as in the present case.
Acknowledgments
We would like to thank Editage (www.editage.jp) for English language editing.
Conflict of Interest
There is no conflict of interest to declare.
Financial Support
There was no funding source for this article.
| References | ▴Top |
- MacLennan GT. Hinman's atlas of urosurgical anatomy, 2nd ed. Elsevier Books, 2012:192-194.
- MacLennan GT. Hinman's atlas of urosurgical anatomy, 2nd ed. Elsevier Books, 2012:158-159.
- Pomel C, Naik R, Martinez A, Ferron G, Nassif J, Dauplat J, Jeyarajah A. Systematic (complete) para-aortic lymphadenectomy: description of a novel surgical classification with technical and anatomical considerations. BJOG. 2012;119(2):249-253.
doi pubmed - MacLennan GT. Hinman's atlas of urosurgical anatomy, 2nd ed. Elsevier Books, 2012:158.
- MacLennan GT. Hinman's atlas of urosurgical anatomy, 2nd ed. Elsevier Books, 2012:11-20.
doi - Urban BA, Ratner LE, Fishman EK. Three-dimensional volume-rendered CT angiography of the renal arteries and veins: normal anatomy, variants, and clinical applications. Radiographics. 2001;21(2):373-386; questionnaire 549-355.
- Klemm P, Frober R, Kohler C, Schneider A. Vascular anomalies in the paraaortic region diagnosed by laparoscopy in patients with gynaecologic malignancies. Gynecol Oncol. 2005;96(2):278-282.
doi pubmed - Kinnunen J, Totterman S, Tervahartiala P. Ten renal arteries. Eur J Radiol. 1985;5(4):300-301.
pubmed - Jamkar AA, Khan B, Joshi DS. Anatomical study of renal and accessory renal arteries. Saudi J Kidney Dis Transpl. 2017;28(2):292-297.
doi pubmed - Satyapal KS, Haffejee AA, Singh B, Ramsaroop L, Robbs JV, Kalideen JM. Additional renal arteries: incidence and morphometry. Surg Radiol Anat. 2001;23(1):33-38.
doi pubmed - Eisendrath DN, Strauss DC. The surgical importance accessory renal arteries. JAMA. 1910;55(16):1375-1377.
doi - Chitra R. A study of various types of accessory renal arteries. Int J Anat Res. 2016;4(3):2269-2273.
- Lee YS, Lee JH, Choi JS, Son CE, Jeon SW, Kim JT, Joo KJ, et al. Accessory polar renal artery encountered in transperitoneal systemic laparoscopic paraaortic lymphadenectomy. Eur J Gynaecol Oncol. 2011;32(1):87-90.
pubmed - Lee WM, Choi JS, Bae J, Jung US, Eom JM. Encountering the Accessory Polar Renal Artery during Laparoscopic Para-Aortic Lymphadenectomy. J Minim Invasive Gynecol. 2018;25(1):10-11.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
