| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 8, Number 1, March 2019, pages 25-28
Treatment of Mesh-Associated Abscess Using an Incision-Free Technique: A Case Series
Joseph Panzaa, b, Parisa Samimia, Carl Zimmermana
aDepartment of Obstetrics and Gynecology, Vanderbilt University Medical Center, Nashville, TN, USA
bCorresponding Author: Joseph Panza, Department of Obstetrics and Gynecology, Vanderbilt University Medical Center, 1161 21st Ave. South B1100 MCN, Nashville, TN 37232-2521, USA
Manuscript submitted March 1, 2019, accepted March 12, 2019
Short title: Treatment of Mesh-Associated Abscess
doi: https://doi.org/10.14740/jcgo538
| Abstract | ▴Top |
Patients who undergo pelvic mesh placement are at risk for developing infectious complications. In the case of an abscess associated with the mesh, removal is often necessary for resolution of the infection. This report describes two cases of delayed abscesses associated with mesh for posterior compartment prolapse and stress urinary incontinence. Definitive treatment for both involved complete removal of the offending portion of mesh without the need for an incision. In patients who develop infectious complications involving pelvic mesh, providers must consider removal of the mesh as a method for source control. Here, exploration of an existing sinus tract allowed for complete mesh removal without the need for extensive dissection. This is especially important in those with medical comorbidities resulting in poor wound healing.
Keywords: Pelvic abscess; Pelvic mesh; Surgical technique
| Introduction | ▴Top |
The use of polypropylene mesh is a mainstay in the treatment of stress urinary incontinence (SUI) and is one of the most well studied surgical modalities in women’s health since its introduction in the mid-1990s [1, 2]. Mid-urethral slings and pelvic mesh for prolapse have undergone a number of permutations all with the goal of improving surgical outcomes while decreasing potential complications. Type I mesh remains in use as the standard of care for treatment of SUI [3]. More recently, concerns around the use of synthetic mesh for pelvic organ prolapse (POP) have resulted in a decrease in use [4]. Specific concerns include the risks of scaring, exposure, pain, and infectious complications. In any patient with a foreign body, there is risk of long-term infectious complications. We present two cases of mesh associated with abscess formation remote from initial placement and removed through an existing draining sinus tract eliminating the need for an incision.
| Case Reports | ▴Top |
Case 1
Case description
We first present the case of a 70-year-old G3P3003 with a complex surgical history involving multiple prolapse and incontinence procedures, presenting with a recurrent right gluteal abscess. Her medical history includes hypertension, hyperlipidemia, and diverticulitis. In addition to an abdominal hysterectomy, her pelvic reconstructive surgical history includes a retropubic midurethral sling in 2005 followed by a laparoscopic sacral colpopexy (Gynemesh, Ethicon Inc., Sommervile, NJ, USA) and transobturator sling (TVT-O, Ethicon Inc., Somerville, NJ, USA) a year later. She then underwent a rectocele repair and Avaulta (C.R. Bard, Inc., Murray Hill, NJ, USA) mesh procedure with excision of a previously placed sling (it is unclear which sling was removed based on the operative report) and placement of a pubovaginal sling.
The patient had undergone transcutaneous incision and drainage of a right ischioanal fossa abscess on two separate occasions without mesh removal at an outside institution. After the second procedure, vaginal mesh exposure was noted and she was referred to our institution. Initial exam revealed a region of scarring in the perianal area, to the right of the midline consistent with an intermittently draining buttock abscess. At her initial visit, it was not fluctuant, with no acute inflammation or tenderness. The scarred area was adjacent to one of the posterior Avaulta insertion points. In the midline of the distal vagina there was a mesh exposure of approximately 2.0 × 2.0 cm. No other mesh exposures were noted.
At that time, we recommended removal of all graft material with possible exploration of the right pelvic side wall and right ischioanal fossa in order to treat and avoid additional recurrence of her right buttock abscess. The patient was counseled that a staged procedure may be necessary to remove all mesh.
Surgical course
The initial procedure used the exposed vaginal mesh as a starting point. With gentle traction and a combination of sharp and blunt dissection, the mesh was debrided from the surrounding tissue to the ischioanal fossa. All visible mesh was removed from the vagina following the procedure.
At the patient’s 3- and 6-week post-operative visits, a pustule over the scarred perianal area was noted. The decision was made to proceed with surgical removal of graft material from the ischioanal area using a transgluteal approach to prevent and treat recurrent abscess formation.
Using a bile duct dilation probe, the right buttock abscess was traced through the ischioanal fossa to the right lateral aspect of the vagina. The tract was opened using a tonsil clamp. Cultures of the area revealed Streptococcus constellatus. The tonsil clamp was then used to explore the sinus tract and easily grasp and remove a 3-cm piece of mesh remaining in the fatty tissue of the buttock. The area was probed and irrigated and there was felt to be no more remaining mesh. The tract was then packed with iodoform packing.
The wound packing was removed in the clinic 2 days after surgery. She was instructed to probe the wound daily with a sterile cotton swab to facilitate healing from the base up. At her 3-week post-operative visit the wound had healed.
Case 2
Case description
Similarly, we present the case of a 50-year-old G2P2002 with a history of multiple pelvic and incontinence procedures presenting with left thigh myositis, cellulitis, and groin abscess. Her medical history is significant for type 2 diabetes mellitus, hepatitis C infection, and active tobacco use. Her pelvic reconstructive surgical history involves laparoscopic-assisted vaginal hysterectomy, transobturator mid-urethral sling (Align, C.R. Bard, Inc., Murray Hill, NJ, USA), and cystoscopy in March 2010 for symptomatic uterine prolapse, abnormal uterine bleeding, and SUI. She subsequently underwent a laparoscopic bilateral salpingo-oophorectomy, retropubic mid-urethral sling (Align, C.R. Bard, Inc., Murray Hill, NJ, USA) in October 2010 for persistent pelvic pain and SUI. In 2015, she presented to her provider at that time for persistent pelvic pain and was found to have a partial mesh exposure. Approximately 4 mm of exposed mesh was excised immediately beneath the mid-urethra.
She presented to our institution with left groin and upper thigh cellulitis. On magnetic resonance imaging (MRI), she was found to have a multi-loculated abscess and myositis in the left groin involving the left adductor magnus, brevis, and longus muscles (Fig. 1). The patient was treated with broad-spectrum antibiotics, but continued to experience left groin and thigh pain with persistent abscess. She remained afebrile with negative blood and urine cultures. On ultrasound imaging, an echogenic structure in the left groin measuring 3.2 × 0.6 cm was thought to be consistent with residual transobturator mesh. A 3.0 × 3.4 × 2.7 cm abscess was also seen (Fig. 2). No mesh could be visualized on internal exam, but a pin point area of friable granulation tissue with purulent drainage was palpated on the left lateral vaginal wall, which was tender on exam. A firm mass was palpated in the left groin, consistent with the abscess seen on imaging.
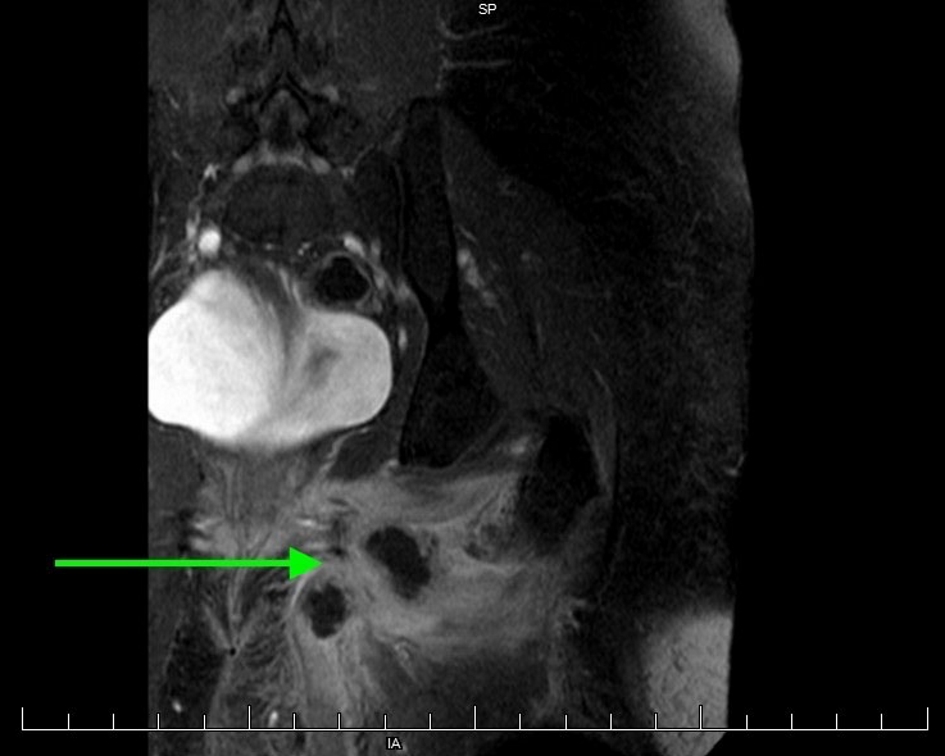 Click for large image | Figure 1. MRI of left groin abscess with associated inflammation. |
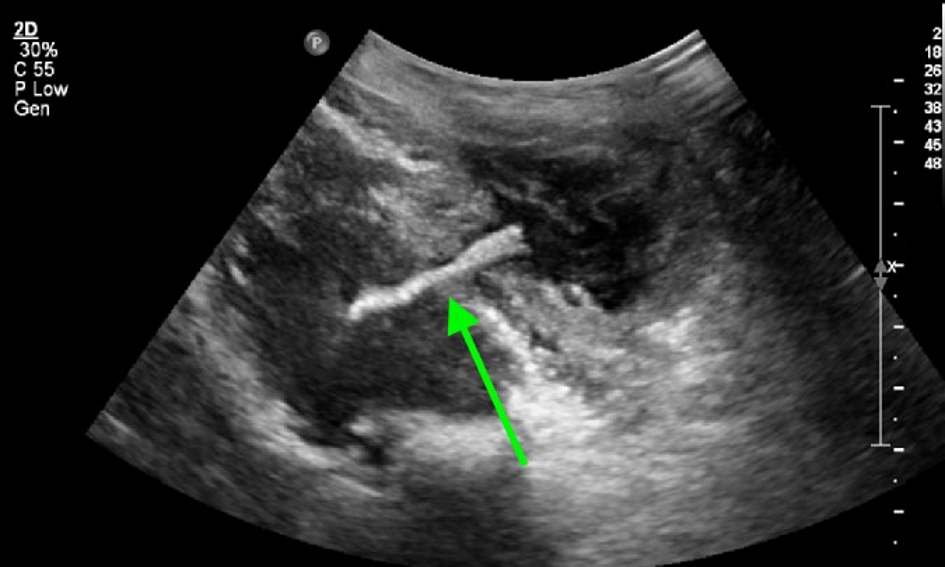 Click for large image | Figure 2. Ultrasound image of mesh within the left groin abscess. |
Given the persistent nature of the infection despite intravenous (IV) antibiotics, the patient was taken for exam under anesthesia and removal of left graft material.
Surgical course
Exam under general anesthesia revealed a 0.5-cm area of ulcerated tissue on the left lateral vaginal wall. The overlying epithelium was gently denuded revealing a scant area of white mesh, which was removed with gentle traction. The entirety of the left arm of the trans-obturator mesh was believed to be removed intact (Fig. 3). The operative site was copiously irrigated.
 Click for large image | Figure 3. Removed transobturator sling mesh. |
The groin abscess was drained. A small, central fluctuant area could be appreciated in the left groin. Approximately 8 mL of purulent discharge was aspirated. The vaginal epithelium was not closed, in order to prevent re-accumulation of purulent material, as there was presumed to be a connecting tract to the abscess given its location around the graft material.
Abscess cultures demonstrated mixed bacterial growth, with no single species isolated.
| Discussion | ▴Top |
While the use of transvaginal mesh for POP has decreased, there remains a large cohort of women who have had this material placed and are at risk for complications in the future. The cases presented here highlight the importance of considering mesh-related infections in patients found to have a pelvic abscess, specifically in the setting of a draining sinus.
Interestingly, both cases involved the use of type 1 mesh, which historically has less infectious complications due to its macroporous design and ability to integrate into host tissue. It is thought that vaginal exposure is the primary risk factor for infectious complications. Two other case reports were identified as involving abscesses associated with type 1 mesh. The first was associated with a Safyre T adjustable kit (Promedon, Cordoba, Argentina), which has silicone arms. The patient in this case had additional risk factors of immunocompromising condition following treatment for breast cancer [5]. The second was associated with an Aris kit (Coloplast, Denmark), in which a patient developed an obturator abscess 1.5 years after placement [6].
The second case in this report presents multiple risk factors for infectious complications, including poorly controlled diabetes, current tobacco use, and a history of multiple mesh surgeries and exposures. Thus, removing the mesh without making an incision in the adductor compartment, an area prone to infection, was a priority. Initial imaging did not clearly reveal any mesh associated with the abscess; it was not until an ultrasound of the adductor showed an unmistakable piece of mesh that the patient was taken to the operating room. Other cases have also shown that mesh is rarely visible on MRI and computed tomography (CT); thus a high degree of suspicion must be maintained in patients with a history of mesh placement [7]. We postulate that ultrasound is an effective, inexpensive tool for locating mesh and assisting in pre-operative planning.
For both patients, treatment was ultimately easily accomplished by complete removal, by extraction, of the foreign body through an infectious sinus tract identified on physical examination. Chronic infection and biofilm formation had prevented or reversed tissue ingrowth into the polypropylene netting allowing easy extraction simply by following the sinus tract. We suggest considering tract exploration in similar cases before more invasive dissection techniques are employed.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors have no conflict of interest or disclosures.
Informed Consent
Not applicable.
Author Contributions
JP and PS contributed to drafting the article. CZ revised the article for critically important content and gave final approval for submission.
| References | ▴Top |
- Welk B, Al-Hothi H, Winick-Ng J. Removal or revision of vaginal mesh used for the treatment of stress urinary incontinence. JAMA Surg. 2015;150(12):1167-1175.
doi pubmed - Jonsson Funk M, Siddiqui NY, Kawasaki A, Wu JM. Long-term outcomes after stress urinary incontinence surgery. Obstet Gynecol. 2012;120(1):83-90.
doi pubmed - Viereck V, Bader W, Lobodasch K, Pauli F, Bentler R, Kolbl H. Guideline-Based Strategies in the Surgical Treatment of Female Urinary Incontinence: The New Gold Standard is Almost the Same as the Old One. Geburtshilfe Frauenheilkd. 2016;76(8):865-868.
doi pubmed - Skoczylas LC, Turner LC, Wang L, Winger DG, Shepherd JP. Changes in prolapse surgery trends relative to FDA notifications regarding vaginal mesh. Int Urogynecol J. 2014;25(4):471-477.
doi pubmed - Brubaker L, Norton PA, Albo ME, Chai TC, Dandreo KJ, Lloyd KL, Lowder JL, et al. Adverse events over two years after retropubic or transobturator midurethral sling surgery: findings from the Trial of Midurethral Slings (TOMUS) study. Am J Obstet Gynecol. 2011;205(5):498 e491-496.
- Martinez Franco E, Rojo N, Amat Tardiu L. Obturator abscess with spread to the thigh muscles after a transobturator tension-free vaginal tape. Int Urogynecol J. 2016;27(6):973-976.
doi pubmed - Geoffrion R, Murphy M, Mainprize T, Ross S. Closing the chapter on obtape: a case report of delayed thigh abscess and a literature review. J Obstet Gynaecol Can. 2008;30(2):143-147.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
