| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Case Report
Volume 9, Number 4, December 2020, pages 119-123
Appendicitis in COVID-19-Positive Patient in Postpartum Period: Differential Diagnosis Dilemma
Predrag Savica, Milan Lackovica, d, Ivana Filipovica, Vladimir Djukica, b, Tamara Bakicc, Sladjana Mihajlovica, b
aUniversity Hospital Dragisa Misovic Dedinje, Belgrade, Serbia
bUniversity of Belgrade, Faculty of Medicine, Belgrade, Serbia
cUniversity of Belgrade, Faculty of Pharmacy, Belgrade, Serbia
dCorresponding Author: Milan Lackovic, University Hospital Dragisa Misovic Dedinje, Belgrade, Serbia
Manuscript submitted May 14, 2020, accepted July 23, 2020, published online December 15, 2020
Short title: Postpartum Appendicitis With COVID-19
doi: https://doi.org/10.14740/jcgo649
| Abstract | ▴Top |
The clinical symptoms of appendicitis in puerperium are atypical and often overlap with other symptoms. A 33-year patient, 8 days postpartum, was admitted due to high fever up to 38.7 °C, dry cough and data showing that she was in contact with coronavirus disease 2019 (COVID-19)-positive person. She was examined, and laboratory and radiographic evaluations were done. After initial treatment she started recovering well, but on the next day due to deterioration of her condition she was urgently operated and acute appendicitis was diagnosed. The coincidence of symptoms of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and the symptoms of appendicitis, as well as impaired immune status in puerperium, make it difficult to detect appendicitis in a timely manner and open the question if acute viral infection such as SARS-CoV-2 can trigger an acute appendicitis.
Keywords: Appendicitis; Puerperium; COVID-19
| Introduction | ▴Top |
Abdominal pain often occurs during pregnancy and after delivery, and the diagnosis in this context is wide ranging. Appendicitis more frequently affects pregnant women, especially in the third trimester of pregnancy. Appendicitis is the most common acute abdominal condition requiring surgical intervention during pregnancy [1-4]. Due to the type of pain and clinical presentation, appendicitis is often difficult to diagnose in the intrapartum or postpartum period. The clinical symptoms are atypical and often overlap with other symptoms of frequent urogenital and non-urogenital conditions in the postpartum period, such as puerperal endometritis, urinary tract infection, adnexal torsion, tubo-ovarian abscess, ovarian vein thrombosis, septic pelvic thrombophlebitis, pyelonephritis, pneumonia and cholecystitis [5]. Patients with appendicitis typically look ill, exhausted and lie in bed, as movement and coughing intensify the pain. Fever is a common feature. In cases of a perforated appendix, the abdominal pain intensifies and is often of a more diffuse character, with probable development of rigidity, tachycardia and elevation of temperature above 39 °C. Laboratory analysis could be helpful in making a diagnosis. Inflammatory parameters (leukocytosis, neutrophilia, and C-reactive protein (CRP) elevation) have shown to be as important as clinical findings (direct and rebound abdominal tenderness and guarding), especially in cases with advanced appendicitis [6, 7]. In addition to ultrasonography, when appendicitis is suspected, additional use of computed tomography (CT) or magnetic resonance imaging (MRI) can be of great help to avoid unnecessary surgery as well as delays in diagnosis [8]. The etiology and pathogenesis of appendicitis have not been understood yet. According to one hypothesis mechanical obstruction due to impaired faeces, peritoneal adhesion or inflated mural lymphoid tissue can cause appendicitis. Also, direct invasion of the pathogen or inflammatory response to infection agent break down the mucosal barrier and lead to appendicitis [9]. In general this obstruction provides an ideal condition for bacterial proliferation that leads to further mucus secretion and increases luminal pressure. Mucosal ischemia follows, owing to decreased lymphatic and venous drainage. It promotes a localized inflammation that may progress to gangrene and perforation [10]. Some studies have focused on an immunological reaction as a potential cause of appendicitis. According to them inflammation in appendicitis is present from the beginning or very early in the progression of the disease. Appendicitis at an early stage is characterized by neutrophils’ infiltration of the mucosa and submucosa [11]. Furthermore some studies showed also an important role of specific immunity in the appendicitis pathogenesis, although the significance of the Th1/Th2 balance in appendicitis has not been understood well yet [12]. In that immunological context of the diseases, pregnant women as well as women in early postpartum period are at high risk knowing the fact that they can be considered as immunocompromised patients [13].
In this paper we have presented an unusual case of postpartum appendicitis after infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and provided an analysis of concomitance of appendicitis and SARS-CoV-2 infection.
| Case Report | ▴Top |
A 33-year-old patient, secundigravida, 8 days postpartum, was referred to coronavirus disease 2019 (COVID-19) dedicated obstetrics and gynecology hospital due to high fever up to 38.7 °C, dry cough and data showing that she was in contact with COVID-19-positive household member. Her past history was negative to serious illnesses. Patient was discharged from the maternity ward with her newborn 5 days prior to admission to our hospital in good physical condition with no signs of infection or inflammation. She was delivered spontaneously of a 4,020 g female infant after 5 h of labor. The prenatal course was normal. Upon admission patient was complaining of abdominal discomfort, nausea, high fever and dry cough. Her vital signs were in reference range except axillary body temperature (38.5 °C). Arterial blood pressure was 120/80 mm Hg, heart rate 77/min, oxygen saturation 98% and respiration rate 20/min were in reference range. The laboratory and radiographic evaluations were done. Due to a household contact with a COVID-19-positive person, COVID-19 swaps were collected. Gynecological examination revealed mild painful sensitivity of uterus and recto-uterine pouch. There was no adnexal tenderness. Abdomen was locally painfully sensitive but there were no signs of acute abdomen. No other irregularities were found. Pelvic ultrasonography revealed intracavitary mass of 17 mm with echoic characteristics of retained products of conception after delivery, without any blood flows. In recto-uterine pouch a formation was visualized (size 130 × 85 mm), with no blood flows. General surgeon was consulted and he excluded a possibility of acute appendicitis.
After receiving COVID-19-positive results of nasopharyngeal swab, chest X-ray was performed and no radiological signs of pneumonia were observed (Fig. 1).
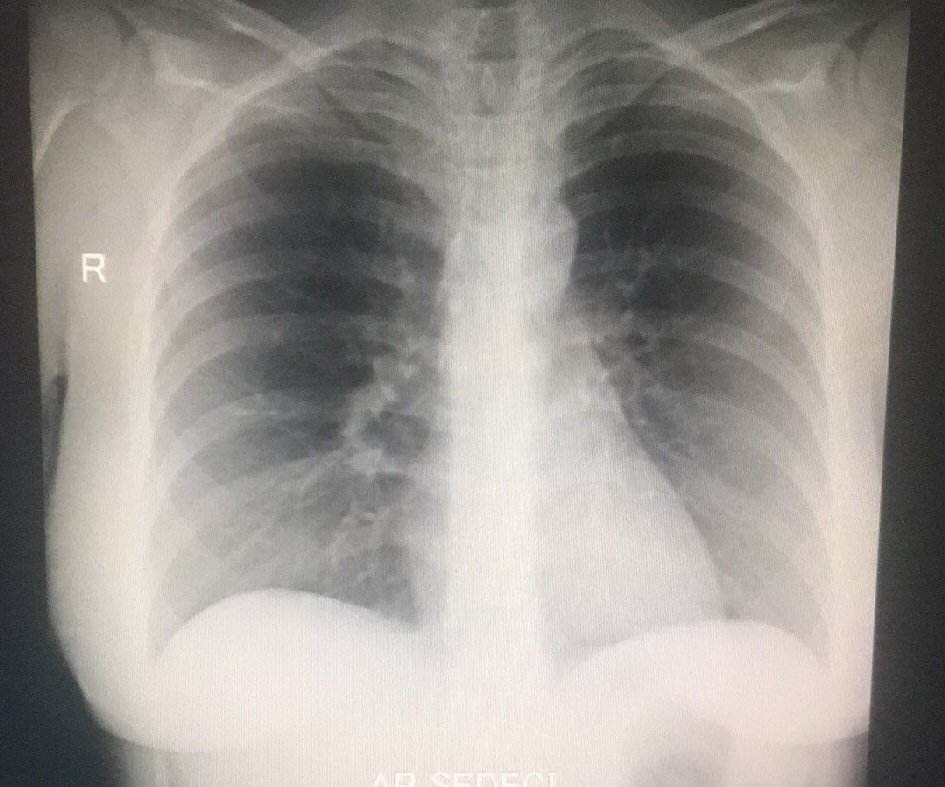 Click for large image | Figure 1. Chest X-ray. |
Laboratory analysis indicated elevated markers of infection and anemia (Table 1). SARS-CoV-2 immunoglobulin M (IgM) and IgG were negative.
 Click to view | Table 1. Laboratory Analysis |
Double antibiotic treatment (ceftriaxone and metronidazole), probiotic and antipyretic were introduced.
Due to pelvic ultrasound results instrumental revision of uterine cavity was performed. Histopathology analysis revealed signs of endometritis and presence of retained products of conception. Patient was treated conservatively as endometritis complicated with acute pelvic peritonitis with triple antibiotic therapy (ceftriaxone, metronidazole and vancomicin), probiotic and antipyretic. Patient was under constant surveillance and in the next 24 h signs of infection were decreasing. In the meanwhile results of her COVID swaps revealed that she was COVID-19-positive. Antiviral therapy was not administrated since she did not have any radiological or clinical signs of pneumonia.
On the following day signs of infection started to rise up dramatically; patient had diarrhea and her heart rate was increasing due to high fever. Patient complained of constant abdominal pain. Pelvic ultrasound was repeated and formation in recto-uterine pouch was enlarged (size 150 × 100 mm). Abdomen was diffusely painfully sensitive. Patient was immediately referred to CT diagnostics. CT scan report revealed presence of free fluid in Morrison’s pouch and right paracolic space and blurred strip zones between bowels. In recto-uterine pouch a formation was described, with density of 25 HU (size 135 × 81 mm, Figs. 2, 3). Spleen had regular size and place, as well as kidneys, liver and gallbladder. Appendix was not enlarged, there were no signs of edema, and it had its usual position given changed anatomical relations in postpartum period. Taking into consideration her deteriorating general condition, values of laboratory analysis and imaging results, explorative laparoscopy was performed.
 Click for large image | Figure 2. Free fluid in Morrison’s pouch (arrow). |
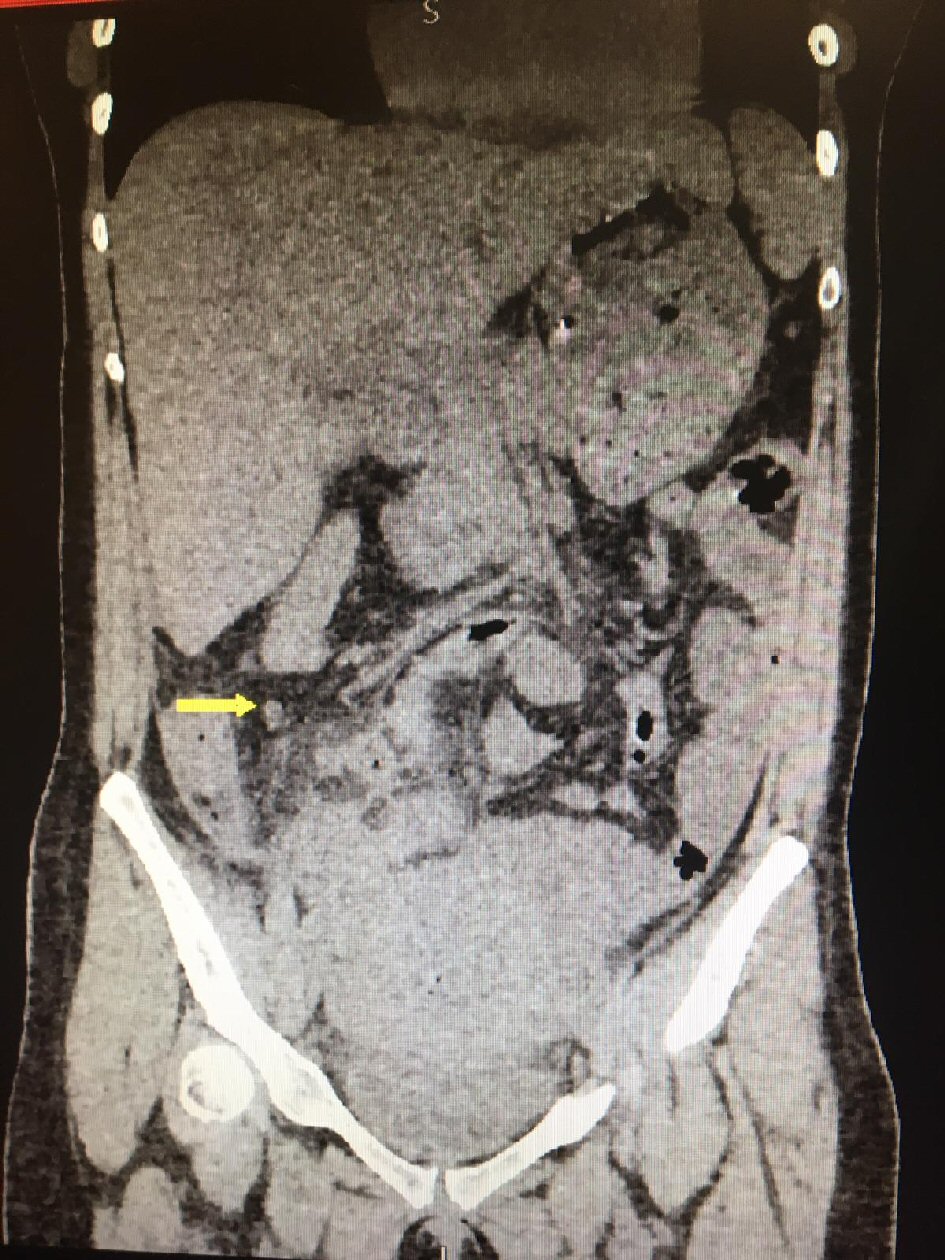 Click for large image | Figure 3. Formation in recto-uterine pouch (arrow). |
Using minimally invasive approach abdominal and pelvic cavity were explored. Massive pus and fibrin deposits were visualized between the intestines, on uterus and in recto-uterine pouch. Gangrenous appendix was visualized with tissue necrosis signs and perforation on basal part. General surgeon was consulted and appendectomy was performed. Right paracolic and retrouterine drain were placed. Histopathology results confirmed presence of gangrenous, ruptured appendix.
Patient was under constant medical surveillance for the next 8 days until she was discharged. She was receiving antibiotic therapy for the next 7 days after the operation and she was afebrile during this time. There were no signs of sepsis.
COVID swaps were recollected 5 days after the operation. The results were negative and she was discharged. Mandatory 14 days long quarantine was requested.
| Discussion | ▴Top |
Infections that occur in the postpartum period are assumed to be related to pregnancy or delivery. The focus of puerperal morbidity should not be limited to urogenital causes, and non-urogenital causes of sepsis should also be considered. Appendicitis is one of the most common non-urogenital causes of puerperal morbidity [13]. Establishing the diagnosis of acute appendicitis in puerperium represents many challenges, and in the time of SARS-CoV-2 pandemic it is much more difficult. As it is previously mentioned, the clinical presentation of SARS-CoV-2 infection may include also gastrointestinal symptoms such as abdominal discomfort, vomiting, nausea, diarrhea followed with high fever and fatigue. For these reasons we were facing many challenges in making an appropriate diagnosis. The presentation of acute appendicitis during the puerperium is mostly atypical and there is often an overlap of symptoms with other more common urogenital and non-urogenital infections in immediate postpartum period; and in our case there was possibility to overlap with manifestation of SARS-CoV-2 infection [14]. In this case after clinical, laboratory and radiographic evaluation the patient was treated as acute pelvic peritonitis with triple antibiotics and was continually monitored. She started recovering well, but after 24 h due to the deterioration of her condition the decision for explorative laparoscopy has been made due to acute appendicitis. Based on published study the SARS-CoV-2 was detected in the fecal samples, because the virus enters the blood from the lungs and then travels from the blood to the intestine; and in our case it may directly damages appendix mucosa and submucosa and cause inflammation [15].
Our case is especially interesting because from immunological point of view pregnancy can be consider as a state of the immune system impairment and in that sense pregnant women represent an immune-unique population. The presence of the fetus and the placenta alters maternal immunity. Signals originating from the placenta can change the mother’s immune response to external and internal antigens [16]. Up to now it is explained that infection with novel SARS-CoV-2 virus stimulates both inherited and specific immunity. The white blood cell (WBC) count in peripheral blood in the early stage of the SARS-CoV-2 disease is normal or slightly low [17], and lymphopenia is observed in infected patients [18]. Laboratory findings of our patients showed the WBC count, neutrophil count and CRP above and lymphocyte count below reference range. Those findings can be explained with the concomitance appendicitis and SARS-CoV-2 infection. The absence of IgM and IgG antibodies in our patient can be explained with the fact that B lymphocytes can be reduced in an early stage of the disease. Published papers have showed (interleukin-6) IL-6 level significantly increased in patients affected with SARS-CoV-2 but also in patients with acute appendicitis.
The coincidence of symptoms of SARS-CoV-2 infection and the symptoms of appendicitis mentioned above, as well as impaired immune status, make it difficult to detect appendicitis in a timely manner and also open the question if acute viral infection such as SARS-CoV-2 can trigger an acute appendicitis. We are only beginning to understand host factors, such as differential expression of cell surface proteins may determine infection risk, disease presentation and outcomes particular in high-risk group.
Appendicitis continues to pose a diagnostic challenge to emergency physicians and surgeons, particularly in puerperium. Clinical impression remains a crucial tool in diagnosis and treatment allocation in those with suspected appendicitis. This specific case is of a great importance to better understand etiology and pathophysiology of acute appendicitis. Further area of research should focus for novel diagnostic test and biomarkers particularly in high-risk groups [19-21].
Acknowledgments
None to declare.
Financial Disclosure
The authors declare no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript.
Conflict of Interest
The authors did not report any potential conflict of interest.
Informed Consent
Informed consent was obtained for patient.
Author Contributions
Predrag Savic and Milan Lackovic conceived and designed the study, and coordinated the data collection. Ivana Filipovic and Tamara Bakic revised the study results and drafted the manuscript. Vladimir Djukic and Sladjana Mihajlovic contributed to data interpretation and manuscript preparation. All authors read and approved the final manuscript.
Data Availability
Data requests can be sent to Dr. Milan Lackovic.
| References | ▴Top |
- Saunders P, Milton PJ. Laparotomy during pregnancy: an assessment of diagnostic accu-racy and fetal wastage. Br Med J. 1973;3(5872):165-167.
doi pubmed - Gomez A, Wood M. Acute appendicitis during pregnancy. Am J Surg. 1979;137(2):180-183.
doi - Mazze RI, Kallen B. Appendectomy during pregnancy: a Swedish registry study of 778 cases. Obstet Gynecol. 1991;77(6):835-840.
- Mourad J, Elliott JP, Erickson L, Lisboa L. Appendicitis in pregnancy: new information that contradicts long-held clinical beliefs. Am J Obstet Gynecol. 2000;182(5):1027-1029.
doi pubmed - Basili G, Romano N, Bimbi M, Lorenzetti L, Pietrasanta D, Goletti O. Postpartum ovari-an vein thrombosis. JSLS. 2011;15(2):268-271.
doi pubmed - Andersson RE, Hugander AP, Ghazi SH, Ravn H, Offenbartl SK, Nystrom PO, Olaison GP. Diagnostic value of disease history, clinical presentation, and inflammatory parameters of appendicitis. World J Surg. 1999;23(2):133-140.
doi pubmed - Andersson RE, Hugander AP, Ghazi SH, Ravn H, Offenbartl SK, Nystrom PO, Olaison GP. Why does the clinical diagnosis fail in suspected appendicitis? Eur J Surg. 2000;166(10):796-802.
doi pubmed - Basaran A, Basaran M. Diagnosis of acute appendicitis during pregnancy: a systematic review. Obstet Gynecol Surv. 2009;64(7):481-488; quiz 499.
doi pubmed - Andersson RE, Lambe M. Incidence of appendicitis during pregnancy. Int J Epidemiol. 2001;30(6):1281-1285.
doi pubmed - Prystowsky JB, Pugh CM, Nagle AP. Current problems in surgery. Appendicitis. Curr Probl Surg. 2005;42(10):688-742.
doi pubmed - Tsuji M, Puri P, Reen DJ. Characterisation of the local inflammatory response in appendi-citis. J Pediatr Gastroenterol Nutr. 1993;16(1):43-48.
doi pubmed - Ruber M, Berg A, Ekerfelt C, Olaison G, Andersson RE. Different cytokine profiles in patients with a history of gangrenous or phlegmonous appendicitis. Clin Exp Immunol. 2006;143(1):117-124.
doi pubmed - Lackovic M, Mihajlovic S, Bakic T, Marina LJ, Stefan Sojat A, Ilic M, Rovcanin M, et al. Imunski sistem u trudnoci. Prev Ped. 2020;6(1-2):37-40.
- Belfort MA, Clark SL, Saade GR, et al. Hospital readmission after delivery: evidence for an increased incidence of nonurogenital infection in the immediate postpartum period. Am J Ob-stet Gynecol. 2010;202:35.e1-e7.
doi pubmed - Chen Y, Chen L, Deng Q, Zhang G, Wu K, Ni L, Yang Y, et al. The presence of SARS-CoV-2 RNA in the feces of COVID-19 patients. J Med Virol. 2020;92(7):833-840.
doi pubmed - Mor G, Cardenas I. The immune system in pregnancy: a unique complexity. Am J Reprod Immunol. 2010;63(6):425-433.
doi pubmed - Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720.
doi pubmed - Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061-1069.
doi pubmed - Thompson GC, Schuh S, Gravel J, Reid S, Fitzpatrick E, Turner T, Bhatt M, et al. Varia-tion in the diagnosis and management of appendicitis at Canadian pediatric hospitals. Acad Emerg Med. 2015;22(7):811-822.
doi pubmed - Andersson M, Ruber M, Ekerfelt C, Hallgren HB, Olaison G, Andersson RE. Can new inflammatory markers improve the diagnosis of acute appendicitis? World J Surg. 2014;38(11):2777-2783.
doi pubmed - Sit M, Catal O, Aktas G, Yilmaz EE, Tosun M, Savli H. Serum amyloid A and Omentin levels in acute appendicitis: a preliminary study for a novel diagnostic approach. Clin Ter. 2014;165(1):e35-38.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
