| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Review
Volume 11, Number 3, September 2022, pages 53-61
Alternatives to Hysterectomy in Patients With Uterovaginal Prolapse
Baburam Dixit Thapaa, c, Tulasa Basneta, G. Willy Davilab, Mohan Chandra Regmia
aDepartment of Obstetrics and Gynecology, BP Koirala Institute of Health Sciences, Dharan, Nepal
bHoly Cross Medical Group, Fort Lauderdale, FL, USA
cCorresponding Author: Baburam Dixit Thapa, Department of Obstertrics and Gynecology, BPKIHS, Dharan, Nepal
Manuscript submitted January 31, 2022, accepted July 6, 2022, published online September 30, 2022
Short title: Alternatives to Hysterectomy for Prolapse
doi: https://doi.org/10.14740/jcgo795
| Abstract | ▴Top |
Background: Uterovaginal prolapse is a common problem in women. Hysterectomy has been considered as a standard procedure during surgical management of pelvic organ prolapse. However, in recent years, interest has been growing in the use of uterus-preserving surgeries. Different options available for uterine preservation include the Manchester Fothergill’s operation, sacral hysteropexy (abdominal, laparoscopic or robotic with or without mesh), uterosacral ligament hysteropexy, sacrospinous hysteropexy (with or without mesh) and colpocleisis. The aim of this review was to analyze the different options of uterus-preserving surgeries and compare their outcomes with prolapse surgeries including hysterectomy.
Methods: PubMed, MEDLINE, Clinical trials.gov and the Hinari database were reviewed through 2020 by two of the authors. Only randomized controlled trials (RCTs) or non-randomized prospective controlled studies (nrPCSs) where different uterus-preserving surgeries for uterovaginal prolapse were compared with surgeries involving hysterectomy were included for the review.
Results: We identified 225 articles from the electronic search and 19 articles meeting the inclusion and exclusion criteria were reviewed. Among them, 10 were RCTs and nine were nrPCSs. The review identified that objective prolapse recurrence, quality of life and adverse events were similar between uterine preservation and hysterectomy groups. Abdominal routes were non-inferior to vaginal uterus-preserving surgeries. Need for repeat surgery after a hysteropexy procedure ranged from 2% to 29%. The Manchester operation demonstrated good anatomical and symptomatic improvement as compared to hysterectomy. When comparing sacrohysteropexy routes, the laparoscopic approach had lower recurrent prolapse symptoms than open sacrohysteropexy. Operating time and estimated blood loss were less with uterus-preserving surgeries. The most common adverse events in hysteropexy surgeries were urinary incontinence, voiding dysfunction, sexual dysfunction and mesh erosion, when mesh used.
Conclusion: The evidence from currently available literature suggests the vaginal and abdominal uterus-preserving surgeries to be equally effective, and not inferior to surgical procedures including hysterectomy. When surgeons are faced with a patient requesting uterine preservation, counseling should be performed cautiously regarding choosing one type of hysteropexy over another. However, the data on long-term follow-up and outcomes are lacking.
Keywords: Hysterectomy; Sacrohysteropexy; Uterus-preserving surgeries; Uterine suspension; Uterovaginal prolapse; Vaginal hysteropexy
| Introduction | ▴Top |
Pelvic organ prolapse (POP) is a common condition that may affect up to 50-70% of women worldwide. On an average, a woman has an 11% risk of undergoing surgery for POP during her lifetime [1]. Pelvic reconstructive surgery can be performed through either abdominal (laparoscopy or laparotomy) or vaginal routes.
Even though the uterus may not be culprit for development of prolapse, hysterectomy is traditionally performed along with POP repairs [2]. Transvaginal hysterectomy (TVH) for POP typically is accompanied by vaginal vault suspension by either uterosacral ligament suspension (USLS) or sacrospinous ligament fixation (SSLF). More recently, the role of hysterectomy during POP repair has been under debate. While some researchers believe that hysterectomy increases risk of complications, others believe that uterine preservation increases the risk of recurrence [3].
Currently, women are increasingly choosing apical POP surgeries that preserve the uterus, a collection of procedures also known as hysteropexy. Preservation of the uterus may be desired for many reasons including future fertility, avoiding higher complication rates during hysterectomy, beliefs regarding impaired sexual function following hysterectomy, and personal choice. Uterine preservation surgeries include Manchester Fothergill’s operation, sacral hysteropexy (abdominal, laparoscopic or robotic with or without mesh), sacrospinous hysteropexy (SSHP, with or without mesh), USLS and colpocleisis. The available data show most approaches are equally effective [4].
There are no clear guidelines on alternatives to hysterectomy in the repair of POP [5, 6]. Given that the number of different studies comparing hysteropexy procedures in different reviews is limited, it is difficult to recommend any specific alternative to hysterectomy. We conducted a review of recent randomized controlled trials (RCTs) and prospective comparative studies, comparing POP surgery with hysterectomy and alternatives to hysterectomy (hysteropexy).
| Materials and Methods | ▴Top |
We performed a systematic search of articles published in peer-reviewed, open-access, indexed journals. An electronic search was conducted on PubMed, MEDLINE,Clinical trials.gov and the Hinari database until through December 2020. Search terms included hysteropexy, uterine prolapse, pelvic organ prolapse, uterine preservation, and hysterectomy. Studies were selected according to population, intervention, comparator, outcome and study design (PICOS) criteria. To be included in the review, the study population had to have POP with a uterus, undergoing surgery (uterine preserving or hysterectomy) and the study design had to be either an RCT or non-randomized prospective controlled study (nrPCS) where uterine preservation was compared with hysterectomy. Studies needed to include assessment of one or more POP outcomes, perioperative or postoperative adverse events, sexual health or quality of life (QoL). Prospective single arm studies, retrospective studies, studies with obliterative surgery (colpocleisis), and studies with only abstract published were not included. Studies that included hysterectomy for non-prolapse benign (fibroid uterus, cervical dysplasia, and adenomysosis) or malignant diseases and POP surgery without apical suspension were excluded.
Studies were graded as good (A), fair (B) and poor (C) depending on the quality of study, risk of biases and completeness of report based on outcomes according to the Cochrane risk of bias tool [7] and relevant questions from Newcastle-Ottawa scale [8].
Alternatives to hysterectomy were categorized as Manchester procedure (MP), modified Manchester (MM), SSHP, vaginal uterosacral hysteropexy, vaginal mesh sacrospinous hysteropexy (VMSSHP), laparoscopic or robotic sacrohysteropexy (LRSHP), laparoscopic uterosacral hysteropexy (Lap USHP) and abdominal sacrohysteropexy (Abd SHP).
| Results | ▴Top |
Eighty full text articles were identified from the search of databases. Nineteen articles met the inclusion and exclusion criteria at the end of the review process. Among them, 10 were RCTs and nine were prospective controlled studies (Fig. 1).
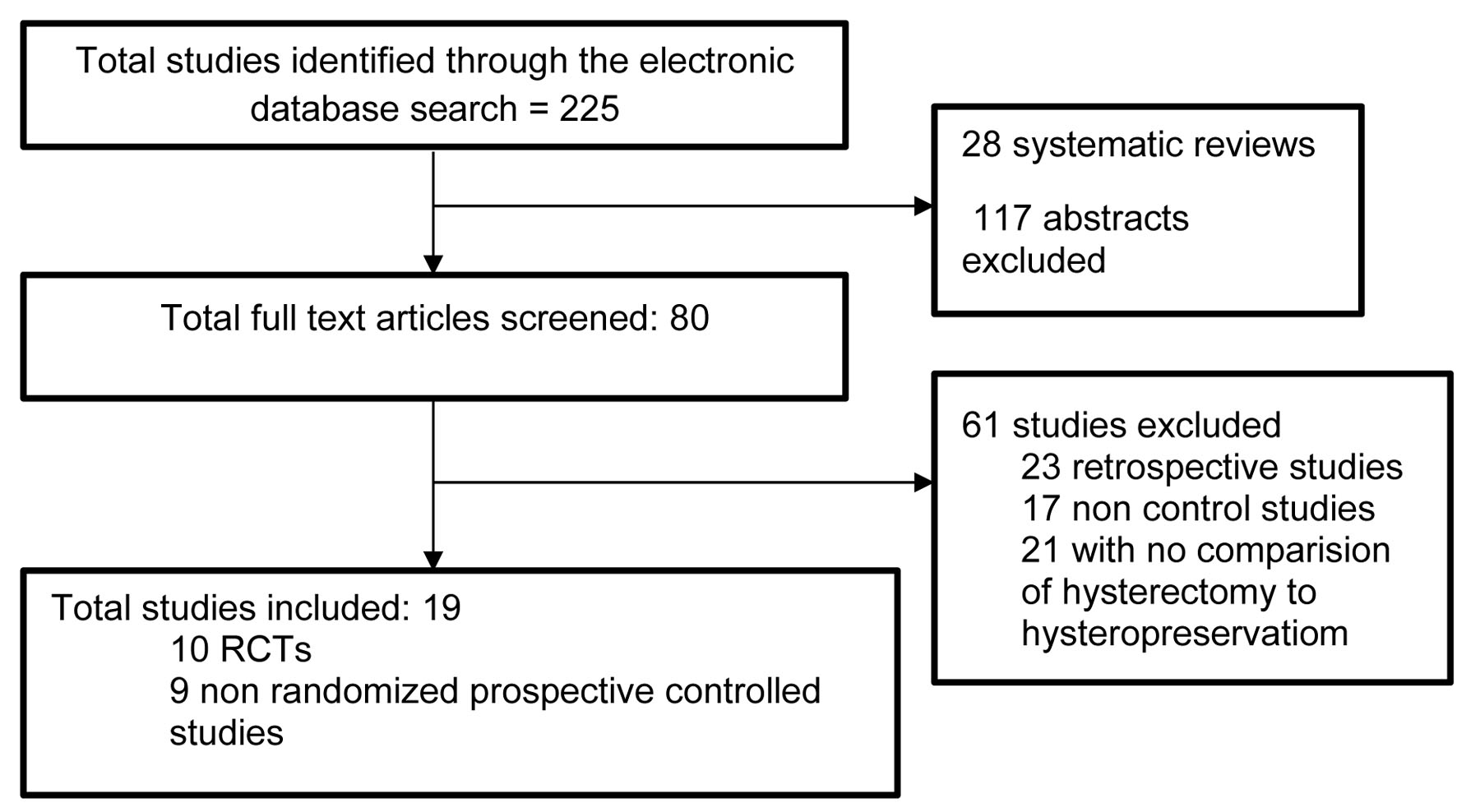 Click for large image | Figure 1. Flowchart showing screening of studies. |
The RCTs compared hysterectomy to hystero-preservation with different fixation types, or different routes or types of uterus-preserving surgeries in the management of uterovaginal prolapse. Of these, 17 studies compared hysterectomy with hystero-preservation with 14 studies that included vaginal hysterectomy. Three studies compared Manchester operation with vaginal hysterectomy. Six RCTs and three prospective controlled studies compared SSHP with other surgeries. One RCT and one nrPCS used vaginal mesh during SSHP. Abdominal route surgeries were compared in six studies (three RCTs and three nrPCS). Among them, two studies used a laparoscopic approach, whereas four used an open approach.
Vaginal hysterectomy technique and any performed associated POP repairs (vault, anterior or posterior) were not uniformly detailed in the reviewed papers. The same can be said about the uterine preservation papers reviewed, as most did not detail additional POP repairs performed, or their techniques used. We thus did not analyze the possible impact of these variables on the reported outcomes. We also did not include that information in the summary tables.
Since there are different alternatives to hysterectomy in terms of type or route of sugery, we reviewed them based on chosen route: either vaginal or abdominal (open/laparoscopic/robotic) hysteropexy.
Vaginal route surgeries
This includes MP, vaginal SSHP and vaginal mesh hysteropexy.
The Manchester operation
MP is considered as one of the earliest uterus-preserving surgeries. Cervical elongation (hypertrophy) is the most common reason for the procedure. The cervix is removed and the stump reattached to the cardinal and/or utero-sacral ligaments. The uterosacral and cardinal ligaments are plicated posteriorly and anteriorly, respectively in modified Manchester operations (Sturmdorf sutures) [9, 10]. Most of the research on MP are retrospective [11] or prospective controlled trials (Table 1) [12-14] and demonstrated significant anatomical and symptomatic improvement as a result of the surgery. We included two nrPCSs and one RCT in this review [9-11]. A retrospective study done in the Netherlands showed significantly less operating time and blood loss in the Manchester group than in the hysterectomy group [8]. The only RCT done in Turkey [11] found that the Manchester group had significantly shorter surgical time (62 vs. 77 min) and significantly shorter hospital stay (P = 0.042) than the vaginal hysterectomy group. Five years after the surgery, there was no statistically significant difference in the postoperative mean C point level between the groups (P = 0.132). Thys et al [12] discovered no differences in functional results or POP recurrence rates between the groups in a similar study.
 Click to view | Table 1. Characteristics of Studies Comparing Manchester Procedure With TVH |
In contrast to previous studies that showed similar anatomical and symptomatic improvement after both the procedures, Tolstrup et al in 2017 [13] found that the risk of recurrent or de novo POP in any compartment was higher after TVH (18.3%) compared to MP (7.8%) and there were more perioperative complications (2.7% vs. 0%, P = 0.007) after TVH. The authors concluded that MP should be recommended over TVH for surgical treatment of POP in the apical compartment if there are no additional indications for hysterectomy. With 2- to 5-year follow-up, the recurrence rate of uterine prolapse ranged from 2.04% to 7.8% and repeat surgery was 1.1-5.4%.
SSHP with or without mesh
The most researched vaginal approach for uterine preservation prolapse surgery is SSHP, which was first described by Richardson [15]. It suspends the cervix with permanent or delayed absorbable sutures by employing the sacrospinous ligaments.
The comparison of transvaginal SSHP with other operations was explored in nine studies (Table 2) (six RCTs and three nrPCSs). Six studies compared SSHP versus TVH (four RCTs [16-19] and two nrPCSs [20, 21]). One RCT [22] compared SSHP with Lap SHP and two (one RCT [23] and one nrPCS [24]) compared mesh augmented SSHP with TVH. In one study, TVH was compared to a combination of uterine preservation surgical techniques [25]. Two cohort studies comparing SSHP with vaginal hysterectomy found no difference in anatomical or symptomatic improvement, but the vaginal hysterectomy group had a three-fold increase in overactive bladder complaints. SSHP is advantageous in terms of blood loss, operational time, and recovery time. However, SSHP had the same rates of recurrence and reoperation as the hysterectomy group [20, 21].
 Click to view | Table 2. Characteristics of Studies Comparing SSHP With Surgeries Involving Hysterectomy |
A study done by Dietz et al [18] showed that SSHP had a shorter operative time and less blood loss. The hysterectomy group had 17% (95% CI: 2-30) decrease in recurrent prolapse compared to SSHP. There were no differences in QoL and urogenital symptoms between the groups.
In 2012, SSHP and vaginal hysterectomy with USLS were compared in a randomized controlled experiment. The follow-up after the procedure was scheduled at 1 and 5 years. At 12 months, SSHP was non-inferior to vaginal hysterectomy in terms of structural apical compartment recurrence with unpleasant bulge symptoms or repeat operation. There were no differences in functional results, QoL, complications, hospital stays, or sexual functioning between the two groups. Anatomical recurrence of the apical compartment with unpleasant bulge symptoms or repeat surgery was substantially higher in the hysterectomy group than in the SSHP group 5 years following surgery (7.8% vs. 1%) [16]. However, there was no difference between the two in terms of functional results, QoL, problems, hospital stays, or sexual functioning [17]. Jeng et al [19] evaluated sexual function in patients undergoing TVH versus SSHP and discovered that TVH patients had lessened sexual interest and orgasms than uterine preservation patients (5.1% vs. 13%).
Table 3 compares the primary and secondary findings of SSHP studies. The majority of the studies found that uterine preservation resulted in reduced blood loss, shorter operative time, and a higher rate of anterior compartment failure. Apical failure occurred at a variable rate. In contrast to the Dietz et al study, there was an increased apical failure rate after hysterectomy [18].
 Click to view | Table 3. Study Comparing SHP Through Various Routes With TVH |
Use of transvaginal mesh is an option during uterine preservation surgery. Mesh is frequently utilized to make a repair more durable. Recent systematic reviews and meta-analyses [26, 27] found that mesh uterine preservation (VMSSHP) surgery resulted in decreased blood loss and operating time, and that recurrence of POP ranged from 2-33% to 3-29%. De novo urinary incontinence, mesh exposure, sexual dysfunction, and urinary retention were all common complications linked with vaginal mesh surgery. When POP surgery included uterine preservation instead of vaginal hysterectomy, both mesh exposure and mesh exposure repeat operation were reduced [24, 26, 28]. Jirschele et al studied mesh augmented SSHP for uterovaginal prolapse and concluded that mesh augmented SSHP was an effective and safe procedure for treating uterovaginal prolapse [29].
One RCT [20] and one nrPCS [21] comparing VMSSHP with TVH were included in this review. The failure rates of POP in both groups were comparable. Mesh exposure was less prevalent, blood loss and operative time were reduced, and the total vaginal length was longer in the uterine preservation group relative to the hysterectomy group. Mesh exposure was seen in 8% of patients in the TVH RCT. In addition, ureteral kinking and suture exposure were shown to be more common in the hysterectomy group. As a result, the controversy over vaginal mesh’s usefulness and safety continues, and further study is needed [23].
Abdominal uterus-preserving surgeries (abdominal/laparoscopic/robotic hysteropexy)
Open, laparoscopic, and robotic sacrohysteropexy are three procedures for uterine preservation that use the sacral promontory as a fixation point with or without mesh. Arthure et al [30] described the open procedure initially but Addison et al [31] described the mesh sacrohysteropexy first. Cutner et al were the first to create a laparoscopic uterine sling suspension [32]. In this review, we identified four RCTs [19, 22, 33, 34] and four nrPCSs [35-38] (Table 4).
 Click to view | Table 4. Studies Comparing Abdominal Uterus-Preserving Surgeries With Surgeries Involving Hysterectomy |
Roovers et al [33] compared open Abd SHP with TVH with anterior and posterior repairs in 2004. Recurrent prolapse symptoms (39% vs. 12%) and repeated prolapse surgery (22% vs. 2%) were substantially greater in the abdominal group than in the vaginal group 1 year after the first surgery. In terms of blood loss, hospital stay, and complications, there was no statistical difference between the two groups. Rahmanou et al [34] conducted a similar study in which they evaluated Lap SHP vs. TVH with anterior and posterior repairs. In this study, Lap SHP had better apical support, longer total vaginal length, a shorter hospital stay, and an earlier return to work postoperatively. The findings were challenged by Alay et al [39] who remarked that the USLS technique used at the time of vaginal hysterectomy may not have been the strongest for apical suspension. They recommended that, because the uterosacral ligaments may be weak in cases of uterovaginal prolapse, McCall culdoplasty or sacrospinous ligament suspension be utilized for apical stabilization, as these procedures may be more equivalent to Lap SHP. Rosen et al [35] examined USLS with uterus or hysterectomy and found that the hysterectomy group had longer operating times with no difference in perioperative or postoperative complications or recurrent prolapse 24 months later.
In a prospective observational research, Alshiek et al [3] compared all types of uterus-conserving operations and discovered that the risk of prolapse recurrence was equal in all surgical methods (abdominal 13.3%, vaginal 14.7%, laparoscopic 11.6%, robotic 3.6%; P = 0.39). All groups had equal rates of intraoperative, postoperative, and long-term complications. Paek et al [36] compared open Abd SHP to LRSHP and reported similar results. They found that objective prolapse recurrence was similar between the groups, but that recurrent prolapse symptoms and repeat prolapse surgery were less common in the LRSHP group. In terms of adverse events, both groups experienced de novo urinary incontinence, but the Abd SHP experienced higher voiding dysfunction and sexual dysfunction rates.
Colposacropexy with or without hysterectomy was compared by Constantini et al [37]. They demonstrated that hysterosacrocolpopexy could be safely performed on women who desired uterine preervation. In terms of prolapse recurrence and improvement in voiding and sexual dysfunction, both surgeries produced identical results. In another study, the same author found that POP has a role in female sexual dysfunction and that uterine preservation operations are linked to better sexual function outcomes [38].
In the LAVA study, Lap SHP was compared to SSHP [22]. In terms of surgical failure, anatomical recurrence, and QoL 1 year after surgery, they determined that Lap SHP was not inferior to SSHP. SSHP had a greater rate of de novo dyspareunia, although it was not statistically significant. They came to the conclusion that while the alternatives for uterine preservation are limited, Lap SHP could be a viable alternative to SSHP.
Recently, two multicenter RCTs comparing various uterine preservation operations to hysterectomy were initiated with planned long-term follow-up [25]. They have reported that objective prolapse recurrence, QoL, and adverse events were similar in the uterine preservation and hysterectomy groups in early data comparison. Increased blood loss and hematoma were the most common major adverse events in both groups. They found no clinical evidence that abdominal uterine preservation surgeries are more effective than vaginal procedures a year following surgery. Abdominal surgeries are more expensive, and the long-term consequences are unknown. They plan to follow up these patients for the next 12 years. As a result, we may be able to better understand the most clinically effective, safe, and cost-efficient options.
The level/depth of dissection, mesh type, and mesh tension used in the reported Lap SHP procedures vary. These differences, as well as others, may influence anatomical and functional outcomes. As a result, more clinical trials are needed to determine optimal surgical techniques, especially when mesh is used [40].
In other hysteropexy techniques, the uterine corpus was previously suture-fixed with sacral promomtary. This surgery has been linked to severe cervical elongation [41].
Mesh has the potential to strengthen and extend apical support by supplementing deficient connective tissue. It may reduce the risk of sexual dysfunction and dyspareunia by preventing vaginal shortening. Clinical trials have yet to back up this claim.
| Discussion | ▴Top |
Our analysis found that uterus-conserving operations are just as beneficial as hysterectomy in the treatment of POP. When compared to hysterectomy, the MP takes less time, results in less blood loss, and requires less time in the hospital. There is no difference in POP recurrence. In short-term follow-up, SSHP was equivalent to hysterectomy for POP recurrence, but it was associated with less operative time and blood loss. The use of transvaginal mesh is still debatable, and the results are contradictory in terms of increased mesh exposure risk. When compared to the vaginal hysterectomy group, Abd SHP had a greater rate of prolapse symptoms and repeat prolapse surgery. However, it resulted in longer overall vaginal length. LRSHP, on the other hand, had greater apical support and a lower risk of repeat apical surgery than the other two groups.
Jeffris et al [42] examined whether hysterectomy is required for POP management and concluded that, despite the growing popularity of uterus-conserving operations, there is no strong evidence that they are superior to hysterectomy. The only putative benefits were improved apical support, reduced vaginal dysfunction, and improved psychological well-being.
The results of a review and meta-analysis of SSHP revealed that the apical failure rate was not significantly different from that of vaginal hysterectomy, indicating that SSHP was a safe and successful surgery for POP [43].
The review done in 2013 by Gutman and Maher [2] found that SSHP is equally effective as vaginal hysterectomy while being associated with lessened operative time, blood loss, and recovery time. Sacral colpopexy and hysterectomy were as successful as SHP (open/laparoscopic), although sacral colpopexy had a five-fold higher rate of mesh erosion than SHP.
According to systematic reviews with meta-analysis and clinical practice guidelines on uterus-preserving surgeries for POP, LRSHP, rather than open SHP, should be considered for women who desire uterine preservation and have no contraindications, to minimize estimated blood loss and urinary retention while reducing mesh exposure and the risk of repeat prolapse surgery. Mesh exposure, urine retention, and sexual dysfunction were the most prevalent adverse effects [27].
Strengths and limitations
A strength of this review is that only RCTs and prospective controlled studies were included. Single technique trials and retrospective reports were excluded. With the exception of colpocleisis, this review included all commonly used uterine preservation operations.
One limitation of this review is that it included a wide range of uterine preservation surgery procedures, resulting in a heterogeneous comparison of results. There are not any randomized trials comparing one uterine preservation operation to another, such as Manchester vs. SSHP. Furthermore, surgical techniques employed for each surgery, whether abdominally or vaginally, can differ significantly. As a result, results reported on a specific surgical approach may not be similar between studies because surgical technique can have a major impact on reported outcomes. In addition, the performance of associated POP repairs (anterior, posterior, and apical) can greatly influence the surgical results and were not uniformly reported in the reviewed series. Furthermore, the surgeon’s skill set and experience can be important, but this study cannot account for those variables.
| Conclusion | ▴Top |
Vaginal hysterectomy is considered as standard treatment for women with uterovaginal prolapse. Numerous uterine preservation surgeries are now becoming more widely accepted as realistic and successful options for women wishing to avoid hysterectomy. The evidence from currently available literature suggests the vaginal and abdominal uterus-preserving surgeries are overall equally effective, and not inferior to surgical procedures that include hysterectomy. However, data regarding long-term follow-up and outcomes are still pending. Counseling should be undertaken regarding available treatment options, the reported recurrence rates, effect on urinary and sexual function, cost and other side effects before a surgeon chooses hysterectomy or one type of hysteropexy over another when presented with a patient requesting uterine preservation. Furthermore, it is impossible to expect every pelvic surgeon to be an expert in all surgical techniques; however, each should be able to provide their patients with safe alternatives.
Acknowledgments
This paper is part of a formal fellowship education program for Dr. Dixit Thapa.
Financial Disclosure
No funding obtained for this project.
Conflict of Interest
None to declare.
Author Contributions
Dr. Baburam Dixit Thapa: study design, article search and synthesis, report writing, and final manuscript preparation. Dr. Tulasa Basnet: article search and synthesis and final manuscript preparation. Dr. G. Wily Davila and Dr. Mohan Ch Regmi: study design and final manuscript preparation.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201-1206.
doi pubmed - Gutman R, Maher C. Uterine-preserving POP surgery. Int Urogynecol J. 2013;24(11):1803-1813.
doi pubmed - Alshiek J, Garcia B, Minassian V, Iglesia CB, Clark A, Sokol ER, Murphy M, et al. Vaginal Energy-Based Devices. Female Pelvic Med Reconstr Surg. 2020;26(5):287-298.
doi pubmed - Korbly NB, Kassis NC, Good MM, Richardson ML, Book NM, Yip S, Saguan D, et al. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol. 2013;209(5):470.e471-476.
doi pubmed - Wu MP, Long CY, Huang KH, Chu CC, Liang CC, Tang CH. Changing trends of surgical approaches for uterine prolapse: an 11-year population-based nationwide descriptive study. Int Urogynecol J. 2012;23(7):865-872.
doi pubmed - Pelvic Organ Prolapse: ACOG Practice Bulletin, Number 214. Obstet Gynecol. 2019;134(5):e126-e142.
doi pubmed - Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
doi pubmed - Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603-605.
doi pubmed - Park YJ, Kong MK, Lee J, Kim EH, Bai SW. Manchester operation: an effective treatment for uterine prolapse caused by true cervical elongation. Yonsei Med J. 2019;60(11):1074-1080.
doi pubmed - Sitaram LA, Shah SH, Sequiera EJ. Shirodkar's modified manchester operation. J Obstet Gynecol India. 1967;296-301.
- de Boer TA, Milani AL, Kluivers KB, Withagen MI, Vierhout ME. The effectiveness of surgical correction of uterine prolapse: cervical amputation with uterosacral ligament plication (modified Manchester) versus vaginal hysterectomy with high uterosacral ligament plication. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(11):1313-1319.
doi pubmed - Thys SD, Coolen A, Martens IR, Oosterbaan HP, Roovers J, Mol B, Bongers MY. A comparison of long-term outcome between Manchester Fothergill and vaginal hysterectomy as treatment for uterine descent. Int Urogynecol J. 2011;22(9):1171-1178.
doi pubmed - Tolstrup CK, Husby KR, Lose G, Kopp TI, Viborg PH, Kesmodel US, Klarskov N. The Manchester-Fothergill procedure versus vaginal hysterectomy with uterosacral ligament suspension: a matched historical cohort study. Int Urogynecol J. 2018;29(3):431-440.
doi pubmed - Unlubilgin E, Sivaslioglu AA, Ilhan TT, Kumtepe Y, Dolen I. Which one is the appropriate approach for uterine prolapse: Manchester procedure or vaginal hysterectomy? Turkiye Klin J Med Sci. 2013;33(2):321-325.
doi - Richardson DA, Scotti RJ, Ostergard DR. Surgical management of uterine prolapse in young women. J Reprod Med. 1989;34(6):388-392.
- Detollenaere RJ, Den Boon J, Stekelenburg J, IntHout J, Vierhout ME, Kluivers KB, et al. Sacrospinous hysteropexy versus vaginal hysterectomy with suspension of the uterosacral ligaments in women with uterine prolapse stage 2 or higher: Multicentre randomized non-inferiority trial. BMJ. 2015;351:h3717.
doi pubmed - Schulten SFM, Detollenaere RJ, Stekelenburg J, IntHout J, Kluivers KB, van Eijndhoven HWF. Sacrospinous hysteropexy versus vaginal hysterectomy with uterosacral ligament suspension in women with uterine prolapse stage 2 or higher: observational follow-up of a multicentre randomised trial. BMJ. 2019;366:l5149.
doi pubmed - Dietz V, van der Vaart CH, van der Graaf Y, Heintz P, Schraffordt Koops SE. One-year follow-up after sacrospinous hysteropexy and vaginal hysterectomy for uterine descent: a randomized study. Int Urogynecol J. 2010;21(2):209-216.
doi pubmed - Jeng CJ, Yang YC, Tzeng CR, Shen J, Wang LR. Sexual functioning after vaginal hysterectomy or transvaginal sacrospinous uterine suspension for uterine prolapse: a comparison. J Reprod Med. 2005;50(9):669-674.
- Hefni M, El-Toukhy T, Bhaumik J, Katsimanis E. Sacrospinous cervicocolpopexy with uterine conservation for uterovaginal prolapse in elderly women: an evolving concept. Am J Obstet Gynecol. 2003;188(3):645-650.
doi pubmed - van Brummen HJ, van de Pol G, Aalders CI, Heintz AP, van der Vaart CH. Sacrospinous hysteropexy compared to vaginal hysterectomy as primary surgical treatment for a descensus uteri: effects on urinary symptoms. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(5):350-355; discussion 355.
doi pubmed - van IMN, van Oudheusden A, Veen J, van de Pol G, Vollebregt A, Radder CM, Housmans S, et al. Hysteropexy in the treatment of uterine prolapse stage 2 or higher: laparoscopic sacrohysteropexy versus sacrospinous hysteropexy-a multicentre randomised controlled trial (LAVA trial). BJOG. 2020;127(10):1284-1293.
doi pubmed - Nager CW, Visco AG, Richter HE, Rardin CR, Rogers RG, Harvie HS, Zyczynski HM, et al. Effect of vaginal mesh hysteropexy vs vaginal hysterectomy with uterosacral ligament suspension on treatment failure in women with uterovaginal prolapse: a randomized clinical trial. JAMA. 2019;322(11):1054-1065.
doi pubmed - Chu LC, Chuang FC, Kung FT, Huang KH. Comparison of short-term outcomes following pelvic reconstruction with Perigee and Apogee systems: hysterectomy or not? Int Urogynecol J. 2012;23(1):79-84.
doi pubmed - Hemming C, Constable L, Goulao B, Kilonzo M, Boyers D, Elders A, Cooper K, et al. Surgical interventions for uterine prolapse and for vault prolapse: the two VUE RCTs. Health Technol Assess. 2020;24(13):1-220.
doi pubmed - Meriwether KV, Antosh DD, Olivera CK, Kim-Fine S, Balk EM, Murphy M, Grimes CL, et al. Uterine preservation vs hysterectomy in pelvic organ prolapse surgery: a systematic review with meta-analysis and clinical practice guidelines. Am J Obstet Gynecol. 2018;219(2):129-146.e122.
doi pubmed - Meriwether KV, Balk EM, Antosh DD, Olivera CK, Kim-Fine S, Murphy M, Grimes CL, et al. Uterine-preserving surgeries for the repair of pelvic organ prolapse: a systematic review with meta-analysis and clinical practice guidelines. Int Urogynecol J. 2019;30(4):505-522.
doi pubmed - Carramao S, Auge AP, Pacetta AM, Duarte E, Ayrosa P, Lemos NL, Aoki T. [A randomized comparison of two vaginal procedures for the treatment of uterine prolapse using polypropylene mesh: hysteropexy versus hysterectomy]. Rev Col Bras Cir. 2009;36(1):65-72.
doi pubmed - Jirschele K, Seitz M, Zhou Y, Rosenblatt P, Culligan P, Sand P. A multicenter, prospective trial to evaluate mesh-augmented sacrospinous hysteropexy for uterovaginal prolapse. Int Urogynecol J. 2015;26(5):743-748.
doi pubmed - Arthure HG, Savage D. Uterine prolapse and prolapse of the vaginal vault treated by sacral hysteropexy. J Obstet Gynaecol Br Emp. 1957;64(3):355-360.
doi pubmed - Addison WA, Livengood CH, 3rd, Sutton GP, Parker RT. Abdominal sacral colpopexy with Mersilene mesh in the retroperitoneal position in the management of posthysterectomy vaginal vault prolapse and enterocele. Am J Obstet Gynecol. 1985;153(2):140-146.
doi - Cutner A, Kearney R, Vashisht A. Laparoscopic uterine sling suspension: a new technique of uterine suspension in women desiring surgical management of uterine prolapse with uterine conservation. BJOG. 2007;114(9):1159-1162.
doi pubmed - Roovers JP, van der Vaart CH, van der Bom JG, van Leeuwen JH, Scholten PC, Heintz AP. A randomised controlled trial comparing abdominal and vaginal prolapse surgery: effects on urogenital function. BJOG. 2004;111(1):50-56.
doi pubmed - Rahmanou P, Price N, Jackson SR. Laparoscopic hysteropexy versus vaginal hysterectomy for the treatment of uterovaginal prolapse: a prospective randomized pilot study. Int Urogynecol J. 2015;26(11):1687-1694.
doi pubmed - Rosen DM, Shukla A, Cario GM, Carlton MA, Chou D. Is hysterectomy necessary for laparoscopic pelvic floor repair? A prospective study. J Minim Invasive Gynecol. 2008;15(6):729-734.
doi pubmed - Paek J, Lee M, Kim BW, Kwon Y. Robotic or laparoscopic sacrohysteropexy versus open sacrohysteropexy for uterus preservation in pelvic organ prolapse. Int Urogynecol J. 2016;27(4):593-599.
doi pubmed - Costantini E, Mearini L, Bini V, Zucchi A, Mearini E, Porena M. Uterus preservation in surgical correction of urogenital prolapse. Eur Urol. 2005;48(4):642-649.
doi pubmed - Costantini E, Porena M, Lazzeri M, Mearini L, Bini V, Zucchi A. Changes in female sexual function after pelvic organ prolapse repair: role of hysterectomy. Int Urogynecol J. 2013;24(9):1481-1487.
doi pubmed - Alay I, Kaya C, Cengiz H. The accuracy of comparing laparoscopic hysteropexy versus vaginal hysterectomy for the treatment of uterovaginal prolapse. Int Urogynecol J. 2018;29(6):923.
doi pubmed - van IMN, Kerkhof MH, Schellart RP, Bongers MY, Spaans WA, van Eijndhoven HW. Variation in the practice of laparoscopic sacrohysteropexy and laparoscopic sacrocolpopexy for the treatment of pelvic organ prolapse: a Dutch survey. Int Urogynecol J. 2015;26(5):757-764.
doi pubmed - Vierhout ME, Futterer JJ. Extreme cervical elongation after sacrohysteropexy. Int Urogynecol J. 2013;24(9):1579-1580.
doi pubmed - Jefferis H, Jackson SR, Price N. Management of uterine prolapse: is hysterectomy necessary? Obstet Gynaecol. 2016;18(1):17-23.
doi - Kapoor S, Sivanesan K, Robertson JA, Veerasingham M, Kapoor V. Sacrospinous hysteropexy: review and meta-analysis of outcomes. Int Urogynecol J. 2017;28(9):1285-1294.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
