| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Case Report
Volume 11, Number 3, September 2022, pages 86-88
A Case Report on an 18-Year-Old Primigravida Patient With Uterine Didelphys
Sameer Narulaa, c, Maggie Jiangb, Paola Rosab
aRoss University School of Medicine, Miramar, FL, USA
bDepartment of Obstetrics and Gynecology, Kern Medical, Bakersfield, CA, USA
cCorresponding Author: Sameer Narula, Ross University School of Medicine, Miramar, FL, USA
Manuscript submitted August 15, 2022, accepted September 23, 2022, published online September 30, 2022
Short title: A Primigravida Patient With Uterine Didelphys
doi: https://doi.org/10.14740/jcgo818
| Abstract | ▴Top |
We present a case of an 18-year-old primigravida who presented to labor and delivery at 41 weeks and 3 days, admitted for induction of labor at late term. During her antepartum course, the patient was suspected to have a uterine anomaly, bicornuate vs. uterine didelphys, given the findings during her first trimester ultrasound. The patient was eventually taken for primary cesarean section for category 2 fetal heart tracings after being admitted for induction of labor. After delivery of the fetus and closure of the hysterotomy, patient was noted to have severe uterine atony, requiring massive transfusion protocol and cesarean hysterectomy with a total estimated blood loss of 6,680 cc. This was an interesting case due to the confirmation of the Mullerian anomaly found intraoperatively, and the adverse outcome for the young patient who required a hysterectomy for life-saving measures. Based on literature review, and in consideration of this case, we suggest if suspicion of a Mullerian anomaly in the antepartum period, a full evaluation of the anomaly be performed along with a plan for delivery.
Keywords: Uterine didelphys; Congenital defect; Mullerian duct; Hysterotomy
| Introduction | ▴Top |
Uterine didelphys is a congenital defect of the female genital system that arises from abnormal embryological development of the Mullerian ducts. A didelphys uterus, also known as a double uterus, is one of the least common Mullerian duct anomalies. These anomalies can occur due to failure of development, fusion, cannulization, or reabsorption which normally occurs between 6 and 12 weeks in utero [1]. According to the ESHRE nomenclature, it is a class U2b, with internal indentation > 50% of the uterine wall and external contour straight or with indentation < 50%. There also may be a double cervix or double vagina and a longitudinal septum separating them in two [2].
Most women with a uterine didelphys are asymptomatic, but some present with dyspareunia or dysmenorrhea in the presence of a varying degree of longitudinal vaginal septum. Typically, these uterine anomalies are found incidentally. Most sources estimated the incidence of these abnormalities to be from 0.5% to 5% of the general population of females. In contrast, bicornuate uterus, ESHRE class U3, typically has a fundus that is indented > 1 cm, or a fundal midline exceeding 50% of the uterine wall thickness, and the vagina and cervix are typically normal, with one cervix [2, 3]. It results from a partial instead of complete fusion of the Mullerian ducts. Depending on the extent of fusion, separation of the uterine horns can occur [4]. It is generally accepted that having a uterine anomaly is associated with adverse pregnancy outcomes, such as, increased likelihood of premature labor, spontaneous abortion, cesarean delivery (due to fetal positioning), and/or decreased live births in comparison to those with a normal uterine anatomy [3].
| Case Report | ▴Top |
An 18-year-old G1P0 with a suspected uterine anomaly at 41 weeks and 3 days presented to labor and delivery for scheduled induction of labor. During her prenatal course, findings during maternal-fetal medicine (MFM) first trimester ultrasound detected two definite uterine horns, with a vaginal septum present, but unable to confirm presence of two cervixes. At a subsequent visit, the ultrasound was unable to determine whether the uterus was bicornuate or didelphys, as well as the number of cervixes. No further imaging was ordered to confirm the type of uterine anomaly present. Following clinic visits throughout pregnancy course were unremarkable.
While being induced for late term, the patient developed an intraamniotic infection and developed category 2 fetal heart tracing which continued despite resuscitative measures. She was then taken for primary cesarean delivery. Extensive adhesions were encountered intraoperatively despite the patient having no history of other abdominal surgeries. Visual inspection revealed a uterine didelphys with two separate cervixes and normal tubes and ovaries bilaterally, as well as a transverse vaginal septum that was discovered at the time of her hysterectomy. Adhesions were also noted between the left uterine horn, and a portion of the large intestine. After delivery of the fetus, and closure of the hysterotomy, blood accumulation was greater than expected in the paracolic gutters. A full evaluation to assess for possible sources of bleeding was performed without any obvious source found.
During this time, the decision was made to convert to general anesthesia, due to regional anesthesia becoming inadequate for pain control.
At this point, the patient had lost approximately 2 L of blood, and received 4 units of packed red blood cells (RBCs). During evaluation of possible sources of bleeding, significant uterine atony was noted from both horns, despite continued uterine massage and multiple uterotonics. Massive blood transfusion protocol was initiated, and a decision was made to proceed with a cesarean hysterectomy for life-saving purpose. On-call gynecology-oncologist was called to the operating room, and aided in completion of the procedure without difficulties.
At the end of the operation, the patient’s estimated blood loss was 6,680 cc, and was transfused with a total of 18 units of packed red blood cells, 8 units of fresh frozen plasma, 2 units of platelets, and 7 units of cryoprecipitate. Total operative time in this case was approximately 7 h.
Patient was taken to intensive care unit postoperatively, and was downgraded to the post-partum floor after becoming more stable. Patient had an uncomplicated postoperative course, and was discharged in stable condition on hospital day 8.
Pathology report noted moderate chorioamnionitis, and confirmed uterine didelphys with separate uterine horns, uterine corpus, and separate cervixes. No evidence of other abnormalities or malignancy was noted (Fig. 1).
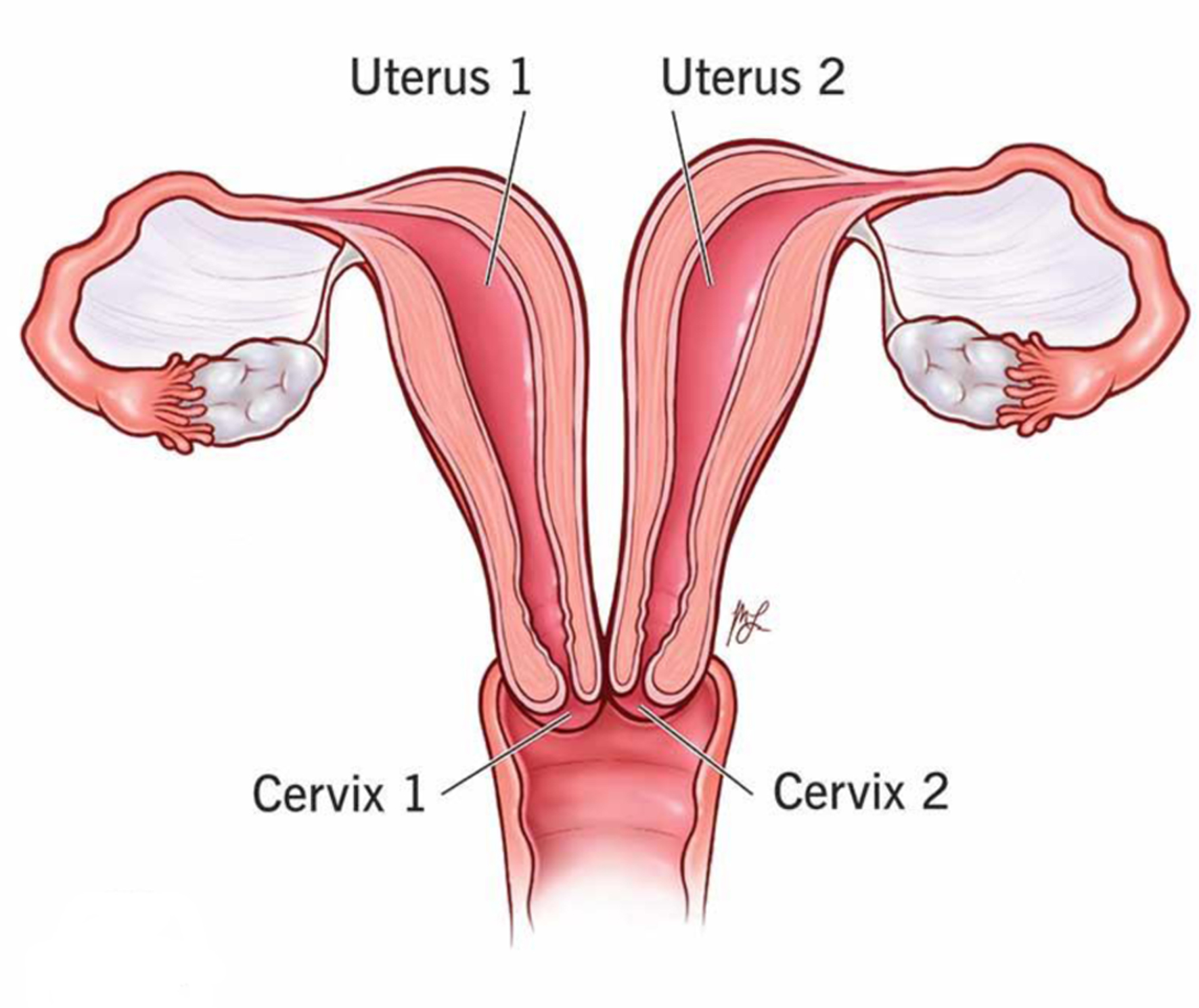 Click for large image | Figure 1. Uterus didelphys: causes, symptoms, diagnosis and treatment. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/23301-uterus-didelphys. Accessed September 18, 2022. |
| Discussion | ▴Top |
In analysis of the case, pathology reports, and further literature review, there are a few points we can consider for future pregnancy planning for women with uterine anatomical anomalies. We recommend discussing the routes of delivery as well as gestational age of delivery early in the antepartum period in patients with a Mullerian anomaly. Early planning would facilitate the proper resources to be available at the time of delivery to minimize possible maternal and fetal adverse outcomes.
Research has also shown the use of general anesthesia to increase the risk of uterine atony, prolonging bleeding time. These anesthetic agents interfere with uterine contractility by affecting hemodynamics. Although in some cases, general anesthesia is a necessity, use of such agents and their adverse effects on uterine tone should be considered [5, 6].
Based on literature review, the best long-term outcome in such uterine anomalies is achieved with an early diagnosis, complete evaluation, clear understanding of the anomaly, mobilization of appropriate surgical resources, sufficient preoperative counseling, and planned surgical intervention if necessary. In similar cases, surgical delivery has been perceived as the safest mode of delivery for Mullerian abnormalities [7]. Therefore, with the aforementioned case and similar presentations, it would have been beneficial to counsel the patient, schedule a delivery date with a planned delivery method at an earlier gestational age, and plan route of delivery given her uterine anomaly diagnosis.
Conclusion
Uterine anomalies, while rare, present a challenging case in labor and delivery. In many cases, uterine anomaly is a mystery until pregnancy is confirmed. In order to avoid emergency surgeries with less than ideal preparations, women with possible uterine anomalies detected at first trimester ultrasounds should be fully worked up, including: imaging such as an magnetic resonance imaging especially in indeterminate cases. Additionally, planning for delivery would allow for the appropriate resources to be available to facilitate a safe outcome for both mother and neonate. Patients with uterus didelphys belong to a high-risk group and deserve meticulous prenatal care [8]. Full diagnosis and evaluation of the anomaly is necessary and important in order to plan for delivery appropriately. On the basis of our review of the literature, we think that uterus didelphys is a sufficient, but not absolute indication for cesarean section. However, although vaginal deliveries have been reported in patients with uterine didelphys, we believe that surgical delivery is a safer method for this Mullerian anomaly [9].
Acknowledgments
None to declare.
Financial Disclosure
The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of Interest
The authors declared no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
Informed Consent
Informed consent for patient information to be published in this article was not obtained because she was lost to follow up.
Author Contributions
Sameer Narula: drafting article, revision, design of work, and conception. Maggie Jiang, DO: drafting article, revision, and interpretation. Paola Rosa, DO, FACOG: critical revision of article and final approval of article for publication.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Maiti GD, Tugnait P, Anand AK, Garg S. Uterine didelphys with pregnancy and cervical incompetence. Med J Armed Forces India. 2006;62(2):200-201.
doi - Grimbizis GF, Gordts S, Di Spiezio Sardo A, Brucker S, De Angelis C, Gergolet M, Li TC, et al. The ESHRE-ESGE consensus on the classification of female genital tract congenital anomalies. Gynecol Surg. 2013;10(3):199-212.
doi pubmed - Rezai S, Bisram P, Lora Alcantara I, Upadhyay R, Lara C, Elmadjian M. Didelphys uterus: a case report and review of the literature. Case Rep Obstet Gynecol. 2015;2015:865821.
doi pubmed - The American Fertility Society classifications of adnexal adhesions, distal tubal occlusion, tubal occlusion secondary to tubal ligation, tubal pregnancies, mullerian anomalies and intrauterine adhesions. Fertil Steril. 1988;49(6):944-955.
doi - Milligan KR. Use of halogenated anesthesia with maternal hemorrhage. NAACOGS Clin Issu Perinat Womens Health Nurs. 1991;2(3):396-401.
- Gilstrap LC, 3rd, Hauth JC, Hankins GD, Patterson AR. Effect of type of anesthesia on blood loss at cesarean section. Obstet Gynecol. 1987;69(3 Pt 1):328-332.
doi - Slavchev S, Kostov S, Yordanov A. Pregnancy and childbirth in uterus didelphys: a report of three cases. Medicina (Kaunas). 2020;56(4):198.
doi pubmed - Raga F, Bauset C, Remohi J, Bonilla-Musoles F, Simon C, Pellicer A. Reproductive impact of congenital Mullerian anomalies. Hum Reprod. 1997;12(10):2277-2281.
doi pubmed - Altwerger G, Pritchard AM, Black JD, Sfakianaki AK. Uterine didelphys and vaginal birth after cesarean delivery. Obstet Gynecol. 2015;125(1):157-159.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
