| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Case Report
Volume 11, Number 4, December 2022, pages 113-116
Huge Mature Cystic Teratoma With Compression and Obstructive Outcome
W Fadhlina W Adnana, Mohd Pazudin Ismaila , Erinna Mohamad Zona
, Nik Mohamed Zaki Nik Mahmooda
, Mohd Shukri Othmana
, Zaleha Kamaludinb
aDepartment of Obstetrics and Gynecology, School of Medical Sciences, Health Campus, Universiti Sains Malaysia, Kubang Kerian, Kelantan, Malaysia
bDepartment of Pathology, School of Medical Sciences, Health Campus, Universiti Sains Malaysia, Kubang Kerian, Kelantan, Malaysia
cCorresponding Author: W. Fadhlina W. Adnan, Department of Obstetrics and Gynecology, School of Medical Sciences, Health Campus, Universiti Sains Malaysia, Kubang Kerian, Kelantan, Malaysia
Manuscript submitted September 11, 2022, accepted October 13, 2022, published online December 30, 2022
Short title: Huge Mature Cystic Teratoma
doi: https://doi.org/10.14740/jcgo828
| Abstract | ▴Top |
Mature cystic teratoma generally presents in a predictable and favorable course. Patients are usually asymptomatic, and the tumor is slow growing. We highlight a case of huge right ovarian teratoma with an unusual presentation with extensive compression disease, which results in the complexity of the case management. A 45-year-old woman, para 4, presented with suprapubic mass 10 × 10 cm with sudden onset lower abdominal pain for 1 day. Pain suddenly subsided, and we diagnosed it as torsion de-torsion. Within 2 months’ duration prior to the scheduled surgery, the tumor progressively increases in size to 24 × 20 cm. The features were also suspicious of malignancy, with bilateral obstructive uropathy causing renal impairment and extensive bilateral lower limb and pelvic vein thrombosis. We inserted a bilateral nephrostomy tube followed by antegrade stenting, and intravenous infusion (IVI) of heparin was changed to subcutaneous (S/C) Clexane 40 mg, twice a day (BID) until the renal function normalized. Surgery was delayed for 6 weeks while she was closely monitored. Intraoperatively the right ovarian tumor has ruptured, features consistent with teratoma. She recovered well postoperatively. Mature cystic teratoma, although generally having a benign course, may present with a fast-growing tumor, with severe bilateral obstructive uropathy and extensive pelvic vein thrombosis.
Keywords: Mature cystic teratoma; Deep vein thrombosis; Obstructive uropathy; Surgery
| Introduction | ▴Top |
Mature cystic teratoma is generally a benign tumor, familiar in women in their 30s, with a size less than 15 cm, and usually presents with acute abdominal pain from torsion of the cyst. They usually have a predictable and favorable course. We highlight a case of unusual presentation of mature cystic teratoma with extensive compression disease, which results in the complexity of the case management.
| Case Report | ▴Top |
A 45-year-old Malay lady, para 4, presented to our emergency department with a suprapubic mass of 10 × 10 cm for 4 months’ duration associated with sudden onset colicky abdominal pain for 1 day.
On our assessment, her pain has subsided. Blood pressure (BP) and pulse rate (PR) were normal. On examination, the abdomen was soft and non-tender on palpation. There was a mass in the suprapubic region (10 × 10 cm in size), cystic in consistency with restricted mobility. Bedside ultrasound revealed the mass as a right ovarian tumor with mixed solid cystic, predominantly cystic with a solid area of 2 × 2 cm. The contralateral ovary, uterus and the rest of the abdominal cavity were normal. The provisional diagnosis was a benign tumor, most likely teratoma with torsion de-torsion. Tumor markers results were cancer antigen 125 (CA 125): 90 U/mL, carcinoembryonic antigen (CEA): 1.5, alpha fetoprotein (AFP): < 8.5 ng/mL, beta human chorionic gonadotropin (BHCG): < 0.5 mIU/mL and lactate dehydrogenase (LDH) was 450 IU/L. She was scheduled for elective surgery laparotomy + cystectomy +/- salpingo-oophorectomy later due to coronavirus disease 2019 (COVID-19) pandemic-elective operating theatre restrictions.
She presented 2 months later for the elective surgery and was noted that the abdominal mass progressively increased to about 28 × 20 cm, cystic to firm consistency, with restricted mobility. Her blood investigations showed that white blood cell (WBC): 15.32 × 109/L, hemoglobin (Hb): 11.6 g/dL, platelet: 457 × 109/L, Urea: 8.5 mmol/L, creatinine: 116 µmol/L, liver function test (LFT) was all normal, CA 125: 59 U/mL, CEA: 2.9 ng/mL, AFP: 2.47 ng/mL (normal), LDH: 350 U/L, BHCG: < 0.5 mIU/mL.
Ultrasound showed that the mass was predominantly cystic with an irregular border and an increase in the size of the solid area within the mass. Bowel appears to be displaced laterally, both kidneys showing severe hydronephrosis. At the same assessment, we noted bilateral lower limb swelling, which was suspected and confirmed as bilateral long segment thrombus from popliteal veins until external iliac veins.
Computed tomography (CT) scan thorax, abdomen and pelvis with angiogram showed a huge right ovarian tumor with mixed solid cystic measuring 24 × 20 cm with solid components within and areas possible breach in the capsule (Fig. 1). The angiogram showed no active bleeding. There was severe bilateral hydronephrosis bilaterally and extensive pelvic vein thrombosis. The inferior vena cava was still patent. The liver and lungs were normal. There was no evidence of pulmonary embolism. The conclusion was huge right ovarian tumor with malignant germ cell tumor (immature teratoma) cannot be ruled out, causing bilateral obstructive uropathy and extensive bilateral pelvic and lower limb thrombosis.
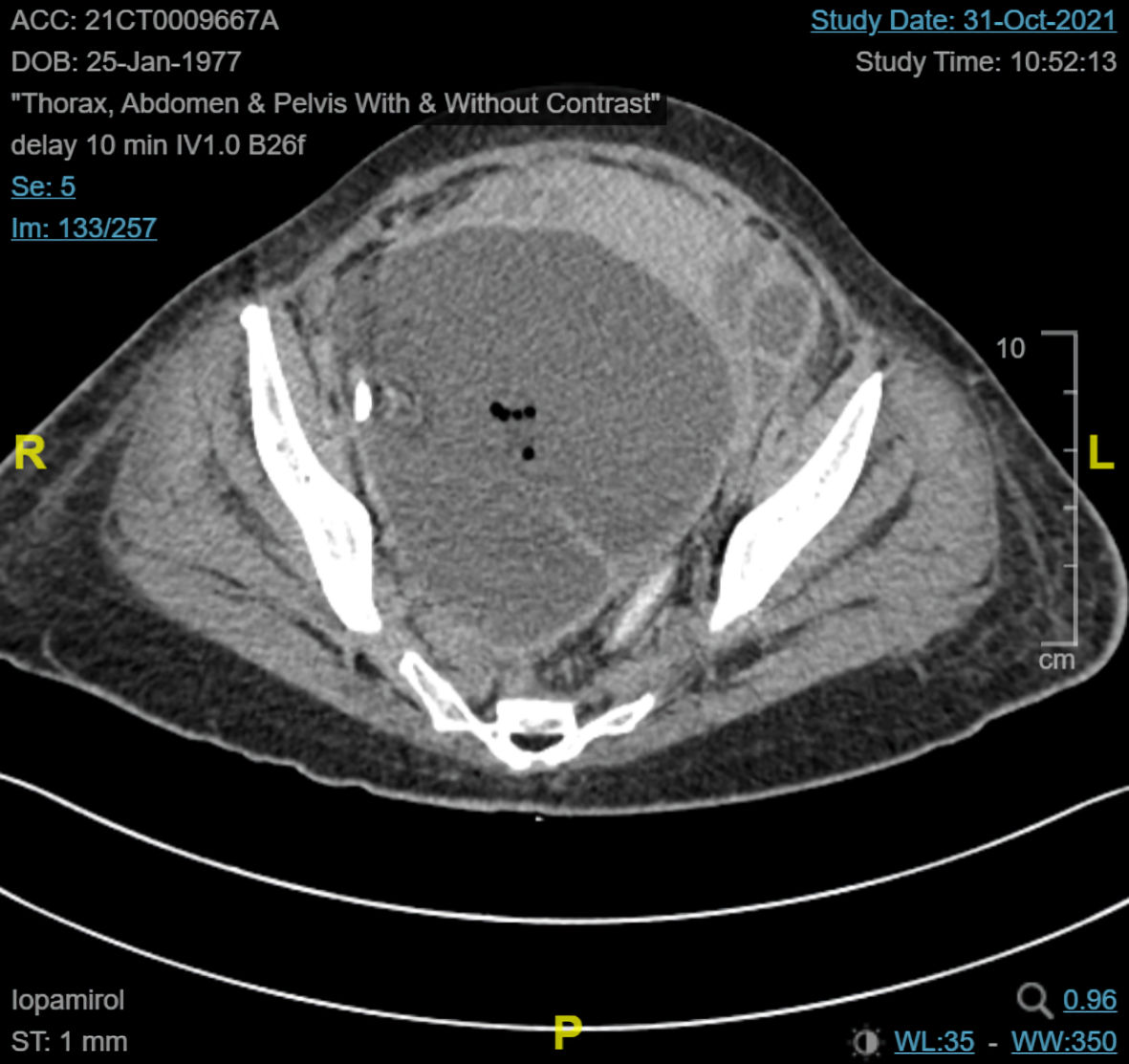 Click for large image | Figure 1. Large cystic mass arising from pelvic region, with presence of internal septations, teeth-like calcifications, fat component and air pockets within. |
The patient and her husband were counseled extensively regarding the diagnosis and further plan. The main issues were a huge right ovarian tumor with suspicious immature teratoma, extensive bilateral lower limb deep vein thrombosis (DVT), and bilateral obstructive uropathy with renal impairment. We proceed with bilateral nephrostomy tube insertion and antegrade ureteric stenting. Once the renal function test was normal, we changed her intravenous infusion (IVI) of heparin into subcutaneous (S/C) Clexane 40 mg, twice a day (BID) for a complete 6 weeks’ duration. She was seen regularly in the clinic with the risk of tumor bleed and monitored.
Bilateral lower limb Doppler ultrasound following 6-week treatment with anticoagulant showed still presence of thrombus at the left lower limb but resolved thrombosis on the right leg. This showed a partial response to the anticoagulant, likely due to still presence of the huge ovarian tumor.
We proceed with exploratory laparotomy and debulking surgery. Intraoperatively the right ovarian tumor already ruptured with a 5 × 5 cm capsular breach with the content of hair and sebum spilled from the tumor. There were no tumor deposits on the surface of the peritoneum, bowels, omentum, liver and subdiaphragmatic area. We managed to debulk the whole tumor (right salpingo-oophorectomy) and proceed with total abdominal hysterectomy and omentectomy. We did peritoneal washing with 10 L of normal saline.
The histopathology report showed all three germinal layers of epithelium with no immature components and no malignant transformation on all the components (Fig. 2a, b). The conclusion on the tumor was mature cystic teratoma. The rest of the contralateral ovary, uterus, and omentum were all within normal findings. The patient recovered well postoperatively, and the stent was finally removed. She was followed up in the gynecology clinic. She remains well, with no active complaints, and ultrasound findings were normal at each visit.
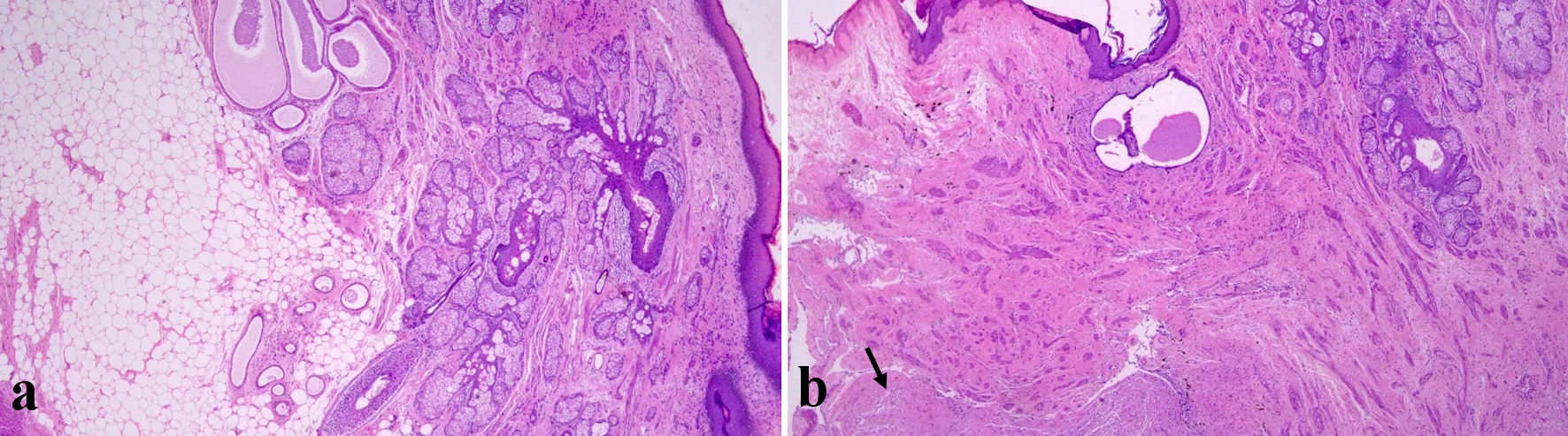 Click for large image | Figure 2. (a, b) Right ovarian cyst wall showing mature skin and its adnexa, adipocytes, and glial tissue (black arrow) (H&E, × 40). H&E: hematoxylin and eosin. |
| Discussion | ▴Top |
Ovarian mature cystic teratoma is common in young women in the reproductive age group (the 30s) [1]. The incidence reported varied from 5% to 44% of all ovarian tumors and among benign ovarian tumors. Ovarian mature teratoma accounts for 58% [2-4].
A reported case of giant ovarian teratoma (size more than 15 cm) is rare [1, 5]. The tumor size is generally around 7 - 11 cm [2, 4], but it can grow up to 28 cm [6]. The tumor has been reported to grow slowly, at 1.8 mm per year [1, 7].
From the evaluation of clinical features of patients with ovarian mature teratoma, the majority are asymptomatic and noted from incidental findings during physical examination or ultrasound [8]. Among patients who presented early, the main complaint is abdominal mass, especially in a giant tumor. Delayed presentation for diagnosis and treatment in giant teratoma is possible in asymptomatic women, with poor socio-economic backgrounds or in areas with restricted health care [9], such as this case.
Patients may present extensively varied symptoms such as lower abdominal pain, gastrointestinal symptoms, or pressure/mass symptoms (urinary frequency, constipation, dyspnea, orthopnea and hydronephrosis [1, 5]. Giant ovarian teratoma commonly presents with acute abdominal pain caused by adnexal torsion and abdominal distension due to the rapid growth of a large, unilateral tumor undergoing capsular distension, hemorrhage and necrosis [10, 11]. However, from the literature review, this is the only known case reporting ovarian teratoma with not only abdominal pain and distension, but also having compression on genitourinary symptoms (obstructive uropathy), gastrointestinal symptoms (constipation) and pelvic vein (thrombosis). These complications are attributed to the giant size of the tumor. These complications add to the complexity of managing the case: obstruction must be relieved with ureteric stenting and anticoagulant.
Well-known complications of ovarian teratoma are torsion, hemorrhage, and rupture. Torsion is the most common cause for emergency surgery (15%). When there is delay in patient presenting to hospital or delay in diagnosis being made, torsion of ovarian teratoma can lead to gangrene [1]. In the case of giant teratoma, it is less likely to have presented with torsion, with one reported case [1].
Spontaneous rupture of dermoid cysts is rare, occurring in 1-2% of the cases [12-14]. Evaluation of 88 cases of ruptured dermoid was reported, with a total of 75 cases published [12]. Among the factors evaluated for the patients, giant teratoma has a higher risk of rupture: 49% are idiopathic, pregnancy-related (26%) and torsion and malignant transformation (7%) [12]. Risks associated with tumor rupture included spillage of sebaceous material, shock and hemorrhage (rare), sequelae marked granulomatous reaction (chemical peritonitis) and may subsequently develop into the formation of dense adhesion [5].
One of the rare complications associated with ovarian teratoma is malignant transformation, which is rare (1-2%). Large tumor size is one of the risk factors for malignant transformation [9, 15]. This comprehensive evaluation of the tumor using ultrasound, tumor markers and a CT scan is important in giant teratoma to exclude malignant transformation. In this patient, the tumor is unlikely to be malignant, as the tumor markers were normal, other than the increment in the size, and the tumor features are similar. The tumor increase in size is likely due to the rupture of the tumor capsule, and the dense tumor content compresses the surrounding structure.
Thus, the most important point in assessing ovarian teratoma is to evaluate the possibility of malignancy, especially from large teratoma and possible accidental rupture or infiltration to adjacent structures [10].
The conventional treatment for large ovarian mature cystic teratoma is by laparotomy approach [1]. There is one successful laparoscopy approach [5] and one case approach laparoscopy and then converted to laparotomy [12]. We proceed with midline laparotomy given its huge size and anticipation of difficult surgery due to compression to the bowel, ureter, bladder, and pelvic vein. We proceed with standard complete debulking surgery and tumor resection, washing, and closure. There was no postoperative peritonitis.
Conclusions
Mature cystic teratoma, although generally having a benign course, may present with a fast-growing tumor, with severe bilateral obstructive uropathy and extensive pelvic vein thrombosis. In conclusion, with a strong understanding of the clinical and pathophysiology of mature cystic teratoma and meticulous management of the case involving a multidisciplinary team, the patient would have a better prognosis. Management of extensive DVT with anticoagulant, nephrostomy and ureteric stenting are inter-related with the surgical management of the huge tumor for safe surgery (reduce the risk of pulmonary embolism and ureteric injury).
Learning points
It is unusual for ovarian mature cystic teratoma, a benign tumor, to grow fast and cause compression to the surrounding organ (bowel, bladder) and veins.
Management of the case with huge tumors already with evidence of rupture, with obstructive uropathy and lower limb thrombosis, need to be individualized based on the case.
Surgery should require careful planning with a multidisciplinary team of gyne-oncologists, surgery, urology, medical and anesthetists.
Acknowledgments
All the authors would like to acknowledge the contribution of Prof. Dr. Mohd Shafie Abdullah and his team in the Department of Interventional Radiology for their assistance in management of the patient.
Financial Disclosure
The authors received no financial support for the research, authorship and/or publication of this article.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Informed Consent
Written informed consent was obtained from the patient to publish this case report and accompanying images.
Author Contributions
WFWA was directly involved in the clinical management of the case, research and writing of the paper. MPI was involved in the clinical management of the case and contributed to the writing of the article. EMZ was involved in the analysis and review of the paper. NMZNM is the consultant of the case and contributed to the research and review of the paper. MSO is the consultant of the case and involved in the conceptual idea of the paper. ZK is involved in the review of the histopathology of the case.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Abbas AM, et al. Torsion of huge dermoid cyst in adolescent girl: A case report. Middle East Fertility Society Journal. 2017;22(3):236-239.
doi - Keskin HL, et al. A giant dermoid cyst of the ovary. Zeynep Kamil Med J. 2011;42(4):161-163.
- Comerci JT, Jr., Licciardi F, Bergh PA, Gregori C, Breen JL. Mature cystic teratoma: a clinicopathologic evaluation of 517 cases and review of the literature. Obstet Gynecol. 1994;84(1):22-28.
- Papadias K, Kairi-Vassilatou E, Kontogiani-Katsaros K, Argeitis J, Kondis-Pafitis A, Greatsas G. Teratomas of the ovary: a clinico-pathological evaluation of 87 patients from one institution during a 10-year period. Eur J Gynaecol Oncol. 2005;26(4):446-448.
- Uyanikoglu H, Dusak A. A huge ovarian dermoid cyst: successful laparoscopic total excision. J Clin Diagn Res. 2017;11(8):QD03-QD05.
doi pubmed - Dos Santos L, Mok E, Iasonos A, Park K, Soslow RA, Aghajanian C, Alektiar K, et al. Squamous cell carcinoma arising in mature cystic teratoma of the ovary: a case series and review of the literature. Gynecol Oncol. 2007;105(2):321-324.
doi pubmed - Khanna S, Srivastava V, Saroj S, Mishra SP, Gupta SK. An unusual presentation of ovarian teratoma: a case report. Case Rep Emerg Med. 2012;2012:845198.
doi pubmed - Laufer M, Goldstein D. Benign and malignant ovarian masses. Pediatric and Adolescent Gynecology. Philadelphia: Lippincott Williams and Wilkins; 2005. p. 706-710.
- Okonta PI, Mofon C. Huge benign ovarian cystic teratoma in a patient with a history of Hansen's disease. Case Rep Obstet Gynecol. 2014;2014:345767.
doi pubmed - Ye LY, Wang JJ, Liu DR, Ding GP, Cao LP. Management of giant ovarian teratoma: A case series and review of the literature. Oncol Lett. 2012;4(4):672-676.
doi pubmed - Ghaemmaghami F, Abbasi F, Abadi AG. A favorable maternal and neonatal outcome following chemotherapy with etoposide, bleomycin, and cisplatin for management of grade 3 immature teratoma of the ovary. J Gynecol Oncol. 2009;20(4):257-259.
doi pubmed - Li RY, Nikam Y, Kapurubandara S. Spontaneously ruptured dermoid cysts and their potential complications: a review of the literature with a case report. Case Rep Obstet Gynecol. 2020;2020:6591280.
doi pubmed - Peterson WF, Prevost EC, Edmunds FT, Hundley JM, Jr., Morris FK. Benign cystic teratomas of the ovary; a clinico-statistical study of 1,007 cases with a review of the literature. Am J Obstet Gynecol. 1955;70(2):368-382.
doi - Waxman M, Boyce JG. Intraperitoneal rupture of benign cystic ovarian teratoma. Obstet Gynecol. 1976;48(1 Suppl):9S-13S.
- Avci S, Selcukbiricik F, Bilici A, Ozkan G, Ozagari AA, Borlu F. Squamous cell carcinoma arising in a mature cystic teratoma. Case Rep Obstet Gynecol. 2012;2012:314535.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
