| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Review
Volume 11, Number 4, December 2022, pages 89-100
Pyometrium as an Early Indicator of Cervical Squamous Cell Carcinoma: A Systematic Review
Brittany Deryndaa, c, Gul Emek Yuksekb, Mohtashim Naeemb, Rahil Malika
aNova Southeastern University, Dr. Kiran C. Patel College of Osteopathic Medicine, Fort Lauderdale, FL, USA
bHCA Florida Westside Hospital, Pathology, Plantation, FL, USA
cCorresponding Author: Brittany Derynda, Nova Southeastern University, Dr. Kiran C. Patel College of Osteopathic Medicine, Fort Lauderdale, FL, USA
Manuscript submitted September 25, 2022, accepted October 24, 2022, published online December 30, 2022
Short title: Pyometrium and Cervical Squamous Cell Carcinoma
doi: https://doi.org/10.14740/jcgo830
| Abstract | ▴Top |
We present the case of an 81-year-old G5P5 Caucasian female who presented to the emergency room for lower abdominal pain, bloating, and green-colored vaginal discharge for the past 3 weeks. A computed tomography of the abdomen and pelvis showed markedly distended endometrial cavity containing fluid and small air bubble concerning for cervical stenosis verses endometrial neoplasm/endometritis suggestive of pyometra. Dilation and curettage was performed with endometrial curette, of which pathology revealed endometritis and detached fragments of squamous cell carcinoma, which showed positive staining with p16, p63, and high Ki67, which is consistent with cervical HPV-related squamous cell carcinoma. The endometrial tissue seen was negative for malignancy. The patient underwent total hysterectomy with bilateral salpingo-oophorectomy and pelvic/para-aortic lymph node dissection, and postoperative recovery was complicated by postoperative ileus which led to a small bowel obstruction. Pyometrium is uncommon, however often presents in postpartum or postmenopausal women and has an 80% association with malignancy. After thorough review of 80 case reports of women with pyometrium, we highlight the importance of considering gynecological malignancy as an underlying cause of pyometra in postmenopausal women, and the importance of early diagnosis in attempt to decrease rates of spontaneous perforated pyometra.
Keywords: Pyometrium; Squamous cell carcinoma; Postmenopausal; Uterine perforation; Spontaneous perforated pyometrium
| Introduction | ▴Top |
Pyometra, or pyometrium, is defined as the accumulation of pus in the uterine cavity due to an interference with drainage and occurs in 0.1-0.2% of all gynecological patients and 12.6% of elderly gynecological patients [1]. Pyometrium is uncommon, but is usually associated with advanced endometrial or cervical cancer. Pyometrium typically presents in postpartum or postmenopausal women with malodorous purulent vaginal discharge, bleeding, and pelvic pain, but can also be asymptomatic [2]. Manifestation of pyometrium is thought to be caused by the accumulation of pus in the uterine cavity resulting from bacteria ascending through the cervical canal with interference with its natural secretion drainage due to cervical stenosis [3]. It is imperative that in postmenopausal women diagnosed with pyometra gynecological malignancy be considered as an underlying cause until proven otherwise. Additionally, early diagnosis of pyometrium may decrease rates of spontaneous perforated pyometra (SPP). Although presentation of SPP predominantly presents with abdominal pain, vomiting and fever, there are no specific symptoms, making diagnosis difficult [4]. Here we describe a case of a postmenopausal female with pyometrium who was found to have underlying cervical squamous cell carcinoma. Additionally, we provide, to our knowledge, an original systematic review of case reports of pyometra focused on presenting symptoms, pathological results, and complications.
| Case Report | ▴Top |
Investigations
The patient was an 81-year-old G5P5 Caucasian female with a history of dementia, alcoholic hepatitis, anemia, hypertension, chronic obstructive pulmonary disease, gastroesophageal reflux disease, irritable bowel syndrome, gastritis, and dyslipidemia. Obstetrical history was significant for menopause at the age of 50 and normal pap smears, although she could not recall the date of her last pap smear. The patient presented to the emergency room for lower abdominal pain, bloating, and green-colored vaginal discharge for the past 3 weeks.
Diagnosis
A computed tomography (CT) of the abdomen and pelvis showed a markedly distended endometrial cavity containing fluid and small air bubble concerning for cervical stenosis verses endometrial neoplasm/endometritis suggestive of pyometra. The patient underwent dilation and curettage with endometrial curette, of which pathology revealed abundant acute purulent inflammation consistent with clinical diagnosis of pyometra, and glandular epithelium with numerous plasma cells consistent with endometritis and multiple detached fragments of squamous cell carcinoma, which showed positive staining with p16, p63, and high Ki-67, that was consistent with cervical human papillomavirus (HPV)-related squamous cell carcinoma (Figs. 1-4). The endometrial tissue seen was negative for malignancy.
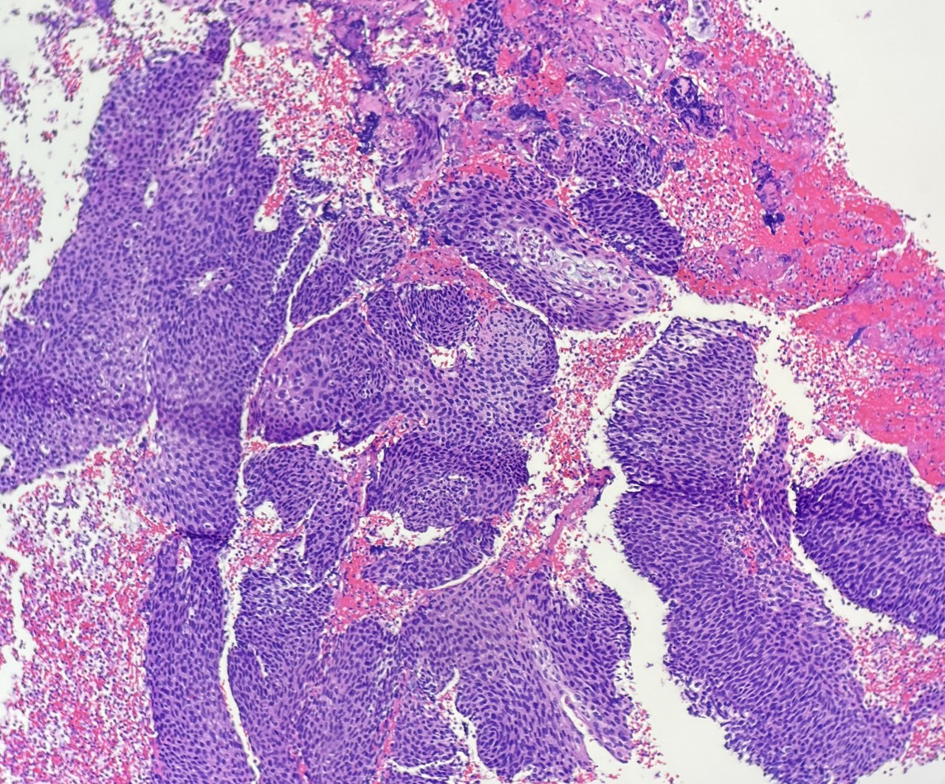 Click for large image | Figure 1. Multiple detached fragments of squamous cell carcinoma in the curettage material (H&E, × 10). H&E: hematoxylin and eosin. |
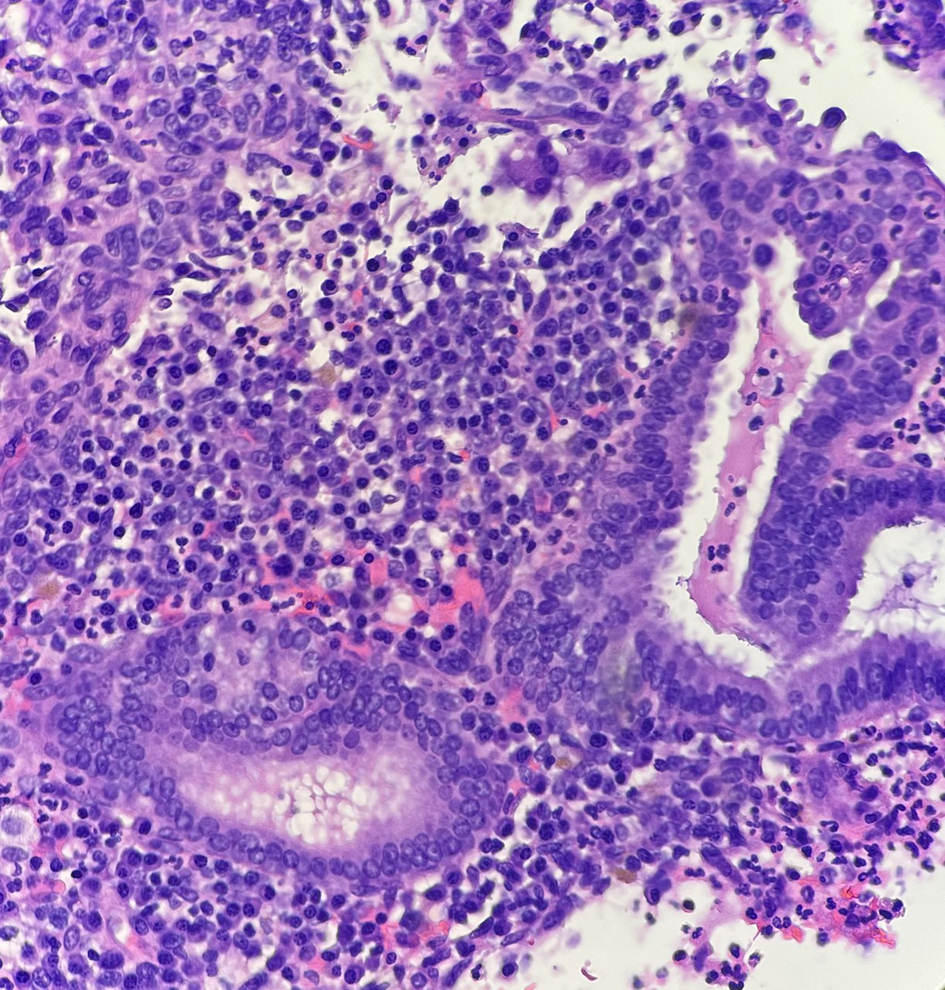 Click for large image | Figure 2. Fragments of glandular epithelium with numerous plasma cells in the curettage material (H&E, × 40). H&E: hematoxylin and eosin. |
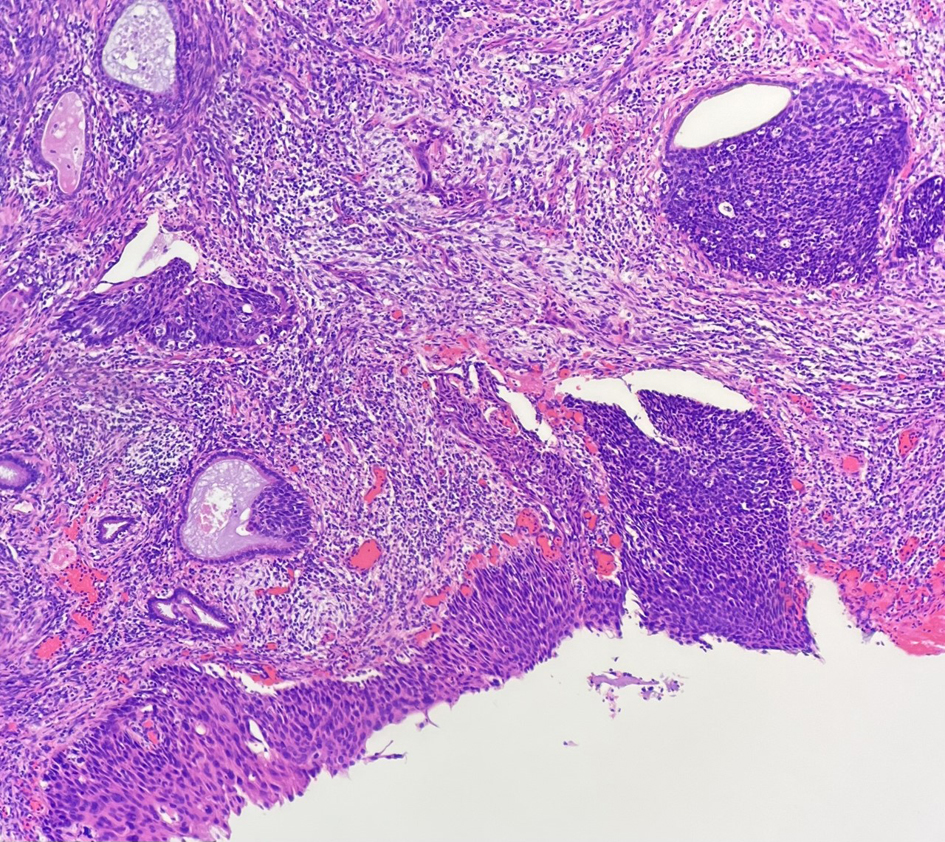 Click for large image | Figure 3. Residual minute microscopic focus of squamous cell carcinoma, hysterectomy material (H&E, × 10). H&E: hematoxylin and eosin. |
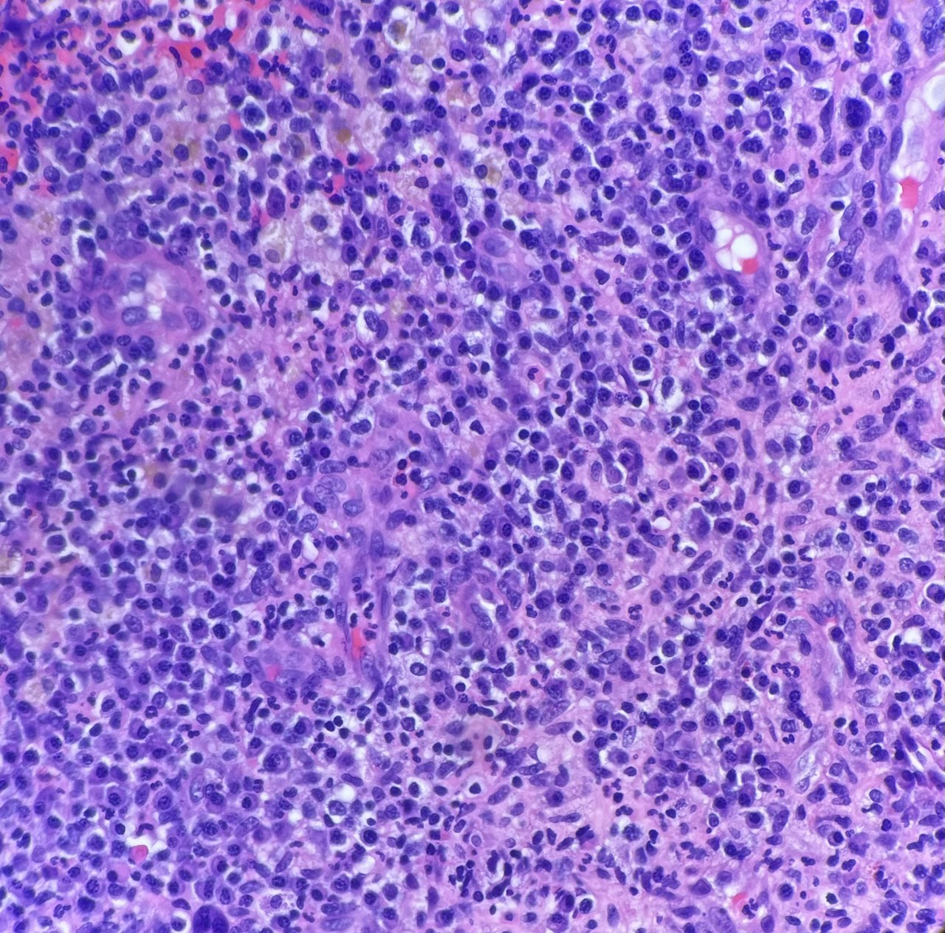 Click for large image | Figure 4. Endometrium with severe acute, histiocytic and plasmocytic inflammation, hysterectomy material (H&E, × 40). H&E: hematoxylin and eosin. |
Treatment
The patient underwent robotic-assisted total hysterectomy with bilateral salpingo-oophorectomy and sentinel, pelvic, and para-aortic lymph node dissection. Pathology revealed residual minute microscopic cervical squamous cell carcinoma (pT1a1 pN0) HPV associated in background of extensive high grade squamous intraepithelial lesion with glandular involvement and severe acute, histiocytic and plasmocytic inflammation consistent with endometritis. Based on various factors, including tumor, node and metastasis (TNM) staging, adjuvant treatment with radiation and chemotherapy was not deemed necessary.
Follow-up and outcomes
Postoperative recovery was complicated by postoperative ileus which led to a small bowel obstruction. The patient removed her own nasogastric tube on multiple occasions which led to acute hypoxemic respiratory failure and intubation. Additionally, the patient formed a new right lateral abdominal wall hernia that contained incarcerated small bowel. The patient returned to the operating room for a diagnostic laparotomy with small bowel resection and reduction of the hernia. Following hernia repair, the patient was discharged to a skilled nursing facility.
| Methods and Search Strategy | ▴Top |
We conducted an electronic-based search using the database PubMed. The medical subject heading of “pyometrium” was used. The search was limited to trials in humans and published in the English language from the 1990s to present day. We manually searched the reference lists of identified studies. We included all original case report articles and excluded pediatric cases.
| Results | ▴Top |
Our search yielded 698 citations with exclusion criteria of non-English articles and date of completion prior to 1990s (Fig. 5). After excluding articles in non-humans, we obtained 206 articles. After eliminating pediatric cases, 113 articles remained. After further exclusion of articles that were abstracts only, picture only articles, articles that the authors were unable to obtain or not related to pyometra, 74 articles were eligible for review. Additionally, five articles reported on multiple cases, leading to the grand total of 80 patient case reports analyzed. Raw data are available in Table 1 [5-75].
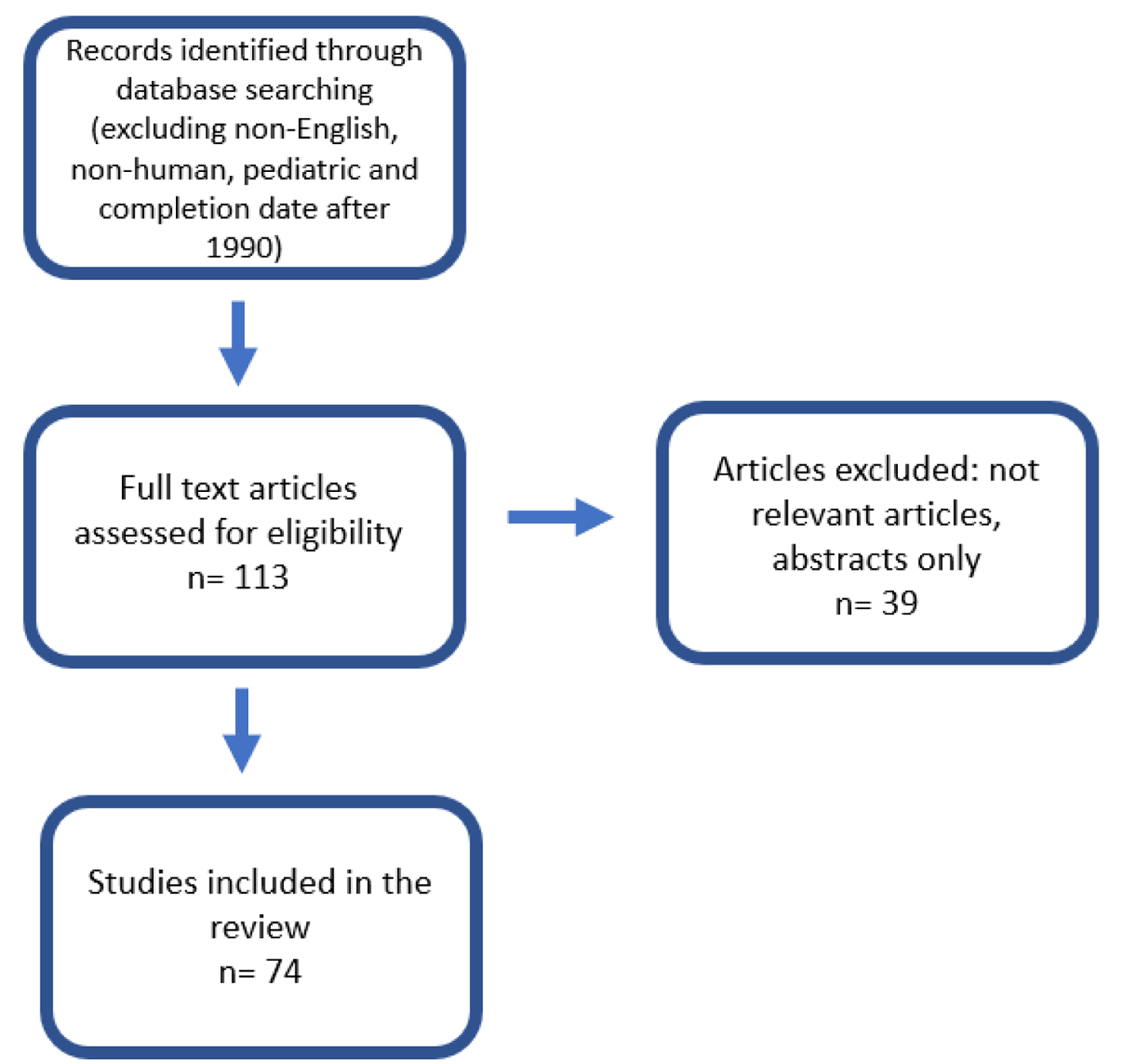 Click for large image | Figure 5. Flow diagram for article selection. |
 Click to view | Table 1. Characteristics of All Studies Included in the Systematic Review |
| Discussion | ▴Top |
Pyometrium has a reported incidence of 0.01-0.05% in all gynecological patients; however, this occurs more frequently in postmenopausal women, with an incidence of 13.6% in women over 60 years old [4]. The pooled average age of patients in our study population was 66 years (range 21-102 years). Of patients diagnosed with cancer, the average age of patients was 64.5 years (range 38-102). In patients not diagnosed with malignancy, the average age was 66.5 years (range 21-93 years). It has previously been shown that in younger patients, there is an increased incidence of pyometrium in those with diabetes, congenital cervical anomalies, cervicitis, large submucosal uterine fibroids, cervical cancer, recent vaginal surgery, or injection drug use [2]. When looking at possible risk factors of pyometra within the cases we analyzed, majority of the patients were multiparous; however, a majority of the studies did not report on the previous medical history of their patient, making it difficult to compare risk factors to those previously identified in the literature.
Known common presenting symptoms of pyometrium include abdominal pain, vomiting, nausea, and fever [9]. The most common presenting symptom within the cases we analyzed was abdominal pain, with 63.2% of patients exhibiting this complaint. The list of differential diagnosis of abdominal pain is vast and includes but is not limited to appendicitis, inflammatory bowel disease, diverticulitis, constipation, acute urinary retention, nephrolithiasis, ovarian torsion, pelvic inflammatory disease and complications of pregnancy including ectopic pregnancy [8]. Additional presenting symptoms within the cases we analyzed included vaginal bleeding and discharge, weight loss, constipation, vomiting, fever, and low back pain.
Diagnosis of pyometrium is traditionally made via imaging modalities including ultrasound (US), CT, or magnetic resonance imaging (MRI), which are required for confirmation or for evaluation of possible complications [5]. Findings from imaging suggestive of pyometra can include uterine enlargement and dilation, accumulation of discharge, and free air. Of the cases we analyzed, 93.6% of them used either US, CT, or MRI for diagnosis of pyometrium. Alternative methods of diagnosis included abdominal X-ray or exploratory laparotomy.
Pyometra has previously been reported to be associated with malignancy in 35% of cases in which pyometra was present [8], however this reported frequency has decreased to 13.6% in the last decade due to progress of cancer screening and diagnosis. Of cases reported, all the cases were diagnosed as squamous cell carcinoma of the cervix besides one reported by Vyas et al 2009 that was reported to be adenocarcinoma of the cervix [6].
Pyometra is often due to a polymicrobial cause, including both aerobic and anaerobic organisms [77] with the most common microorganisms including E. coli, Streptococcus spp., Bacteroides fragilis and Peptostreptococcus anaerobius [78]. Of the case reports we analyzed, there was a wide variety of causative microbes including Tuberculosis, Escherichia, Pseudomonas, Fusobacterium, Enterococcus, Pneumococcus, Clostridium, Sphenoides, Streptococcus, Staphylococcus, Bacteroides and Actinomyces. The microbes we identified were similar to those previously reported on.
Current literature supports basic pyometra treatment with transcervical drainage, irrigation of uterine cavity, and antibiotic therapy with emergency surgical intervention in cases of SPP [4]. In a previous case review of pyometra, treatment with hysterectomy was completed in 82% of cases [9]. Majority (61.6%) of the cases analyzed in our study were treated with hysterectomy. Of those treated with hysterectomy, 72.9% also underwent concurrent bilateral salpingo-oophorectomy. Average age of those treated with hysterectomy was 68.6 years old with a range of 23 to 92 years old. Additionally, only 9% of those treated with hysterectomy had diagnosis of squamous cell carcinoma of the cervix, with the rest having benign findings. Alternative treatment methods included antibiotic therapy and drainage of the pyometra.
If left untreated, pyometra can rarely result in the serious complication of SPP. Prognosis after SPP can be poor, especially in women of advanced age and those with poor general health. Current literature reports rates of SPP to be around 5% [4]; however, in our study group, uterine rupture was reported as a complication in 36.1% of cases. Additional complications reported included subcutaneous abscess, pneumonia, wound dehiscence, and respiratory insufficiency. Eight patients died following complications of the pyometra which included complications such as sepsis, pneumonia, colouterine fistula, organ failure and cancer progression due to refusal of treatment. No cases of recurrence were reported.
| Conclusion | ▴Top |
Preoperative diagnosis of pyometra is difficult but imperative, as early treatment may prevent from future uterine rupture and aid in identification of underlying cause including malignancy. Majority of cases in our analysis presented with abdominal pain and were treated with hysterectomy; however, a wide range of presentations and treatment modalities were identified in the reports included in this analysis. An increased number of cases were complicated by uterine rupture compared to previously reported research, in addition to an increased rate of underlying malignancy. With the presentation of our case and analysis of previously published case reports, we highlight the importance of considering malignancy as a differential diagnosis when presented with a postmenopausal patient with pyometrium, in addition to early intervention to prevent uterine rupture.
Learning points
Highlight a case of pyometra in a postmenopausal woman with underlying gynecological malignancy.
Uterine perforation is a dangerous, and not uncommon consequence of prolonged pyometra, highlighting the importance of early diagnosis.
Underlying gynecological malignancy should be considered as an underlying cause of pyometrium in postmenopausal women.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Author Contributions
BD: literature search, introduction, discussion, abstract, and references. RM: case report, images, and literature search. GEK and MN: description of pathology findings, and images.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
SPP: spontaneous perforated pyometra; US: ultrasound; CT: computed tomography; MRI: magnetic resonance imaging
| References | ▴Top |
- Sawabe M, Takubo K, Esaki Y, Hatano N, Noro T, Nokubi M. Spontaneous uterine perforation as a serious complication of pyometra in elderly females. Aust N Z J Obstet Gynaecol. 1995;35(1):87-91.
doi pubmed - Greenspoon JS, Ault M, James BA, Kaplan L. Pyomyoma associated with polymicrobial bacteremia and fatal septic shock: case report and review of the literature. Obstet Gynecol Surv. 1990;45(9):563-569.
doi pubmed - Sirha R, Miskin A, Abdelmagied A. Postnatal pyomyoma: a diagnostic dilemma. BMJ Case Rep. 2013;2013:bcr2013201137.
doi pubmed - Yazawa H, Imaizumi K. Generalized peritonitis secondary to spontaneously perforated pyometra in elderly women:two cases with different clinical courses and surgical approaches and review of the literature. Fukushima J Med Sci. 2020;66(1):53-59.
doi pubmed - Zarour CC, Zaki-Metias KM, Kaur M, Mian A, Olson EB, Seedial SM. Idiopathic pyometra in a postmenopausal patient. Clin Imaging. 2021;80:145-147.
doi pubmed - Vyas S, Kumar A, Prakash M, Kapoor R, Kumar P, Khandelwal N. Spontaneous perforation of pyometra in a cervical cancer patient: a case report and literature review. Cancer Imaging. 2009;9:12-14.
doi pubmed - Saini A, Yadav G, Gothwal M, Singh P, Kathuria P, Elhence P. Tuberculosis and ovarian malignancy: Sometimes mimics, sometimes coexists. J Obstet Gynaecol Res. 2020;46(6):945-949.
doi pubmed - Walthall L, Heincelman M. Pyometra: an atypical cause of abdominal pain. J Investig Med High Impact Case Rep. 2021;9:23247096211022481.
doi pubmed - Yildizhan B, Uyar E, Sismanoglu A, Gulluoglu G, Kavak ZN. Spontaneous perforation of pyometra. Infect Dis Obstet Gynecol. 2006;2006:26786.
doi pubmed - Uno K, Tano S, Yoshihara M, Mayama M, Ukai M, Kishigami Y, Nishikawa Y, et al. A case report and literature review of spontaneous perforation of pyometra. J Emerg Med. 2016;50(5):e231-236.
doi pubmed - Tay WMI, Subramanian M, Chinchure D, Kok SXS. Clinics in diagnostic imaging (199). Pyometra. Singapore Med J. 2019;60(9):487-490.
doi pubmed - Huang Y, Tian Q. Postmenopausal spontaneous rupture of pyometra: A case report. Medicine (Baltimore). 2018;97(52):e13659.
doi pubmed - Ikematsu Y, Kitajima T, Kamohara Y, Inoue K, Maeda J, Amano M, Kohzaki S. Spontaneous perforated pyometra presenting as pneumoperitoneum. Gynecol Obstet Invest. 1996;42(4):274-276.
doi pubmed - Reis MI, Vicente AP, Cominho J, Gomes AS, Martins L, Nunes F. Pyometra and pregnancy with Herlyn-Werner-Wunderlich syndrome. Rev Bras Ginecol Obstet. 2016;38(12):623-628.
doi pubmed - Sala A, Restaino S, De Carlo C, Comand M, Frigo A, Martinez Rivero S, Zanetti E, et al. Postoperative streptococcus constellatus bacteremia in a 75-year-old patient with pyometra: a case report. Am J Case Rep. 2021;22:e931167.
doi pubmed - Konishi Y, Kagabu S, Mori K, Kato M. Uterine perforation of pyometra in a cervical cancer: A case report and literature review. J Obstet Gynaecol. 2016;36(3):378-379.
doi pubmed - Chishti U, Elorbany S, Akhtar M, Williams J, Heenan S, Barton DPJ. Genital tuberculosis in a post-menopausal Caucasian woman: a case report. J Obstet Gynaecol. 2019;39(2):284-285.
doi pubmed - Hagiya H, Ogawa H, Takahashi Y, Kimura K, Hasegawa K, Otsuka F. Actinomyces turicensis bacteremia secondary to pyometra. Intern Med. 2015;54(21):2775-2777.
doi pubmed - Kutuk MS, Ozgun MT, Tas M, Uludag S. Spontaneous uterine perforation due to pyometra. J Obstet Gynaecol. 2013;33(3):322-323.
doi pubmed - Gul A, Gul Kebapcilar A, Sahin G, Akar S, Celik C. An unusual complication of LEEP cervical conisation with a retained intrauterine device (IUD): a case report. J Obstet Gynaecol. 2019;39(5):718-719.
doi pubmed - Shapey IM, Nasser T, Dickens P, Haldar M, Solkar MH. Spontaneously perforated pyometra: an unusual cause of acute abdomen and pneumoperitoneum. Ann R Coll Surg Engl. 2012;94(8):e246-248.
doi pubmed - Gatongi DK, Kay V. Endometrial tuberculosis presenting with postmenopausal pyometra. J Obstet Gynaecol. 2005;25(5):518-520.
doi pubmed - Pankaja S, Rrukaj A, Bathula U. Diverticular disease of the colon presenting as pyometra: a case report. J Med Case Rep. 2014;8:135.
doi pubmed - Kroon HM, Smolders RG. Acute abdomen caused by spontaneous perforation of pyometra in a patient with cervical cancer. BMJ Case Rep. 2016;2016:bcr2016215958.
doi pubmed - Gupta R, Das A, Krishna PS. Streptococcus agalactiae causing pyometra in an elderly female with cervical cancer. J Infect Dev Ctries. 2012;6(12):891-894.
doi pubmed - Yahmadi A, Haoues N, Zaafouri H, Ben Maamer A, Bouhafa A, Cherif A. Pyometra in a post-menopausal woman diagnosed preoperatively: a case report. Tunis Med. 2014;92(12):768.
- Stunell H, Hou D, Finlayson S, Harris AC. Spontaneous perforation of pyometra due to acute necrotising endometritis. J Obstet Gynaecol. 2011;31(7):673-674.
doi pubmed - Kim J, Cho DH, Kim YK, Lee JH, Jeong YJ. Sealed-off spontaneous perforation of a pyometra diagnosed preoperatively by magnetic resonance imaging: a case report. J Magn Reson Imaging. 2010;32(3):697-699.
doi pubmed - Lodhi W, Golara M, Karangaokar V, Yoong W. Uterine necrosis following application of combined uterine compression suture with intrauterine balloon tamponade. J Obstet Gynaecol. 2012;32(1):30-31.
doi pubmed - Shahid N, Khan H, Onon TS. Perforation of pyometra leading to diffuse peritonitis is not necessarily iatrogenic. J Obstet Gynaecol. 2006;26(1):76-77.
doi pubmed - Chan LY, Lo KW, Cheung TH. Radiographic appearance of pyometra on computer tomography mimicking pelvic abscess. Acta Obstet Gynecol Scand. 2006;85(9):1144-1145.
doi pubmed - Yang CY, Lai MY, Yang WC, Lin CC, Ng YY. Cervical cancer with pyometra—an insidious cause of uraemia in a post-menopausal woman. Nephrol Dial Transplant. 2006;21(10):2984-2985.
doi pubmed - Chen PH, Hsien L, Lee SL, Chang CY, Chang CC. Pneumoperitoneum caused by perforation of pyometra associated with a lost intrauterine device and perforated malignancy of the sigmoid colon. Taiwan J Obstet Gynecol. 2011;50(1):124-125.
doi pubmed - Cheung WK, Ho MP, Shueng PW, Tsang YM. Early cervical cancer complicated by pyometra presenting as a pelvic cystic mass and vaginitis in a 102-year-old patient. J Am Geriatr Soc. 2011;59(6):1140-1141.
doi pubmed - Hofmann GE, Warikoo P, Jacobs W. Ultrasound detection of pyometra at the time of embryo transfer after ovum retrieval for in vitro fertilization. Fertil Steril. 2003;80(3):637-638.
doi - Lee SL, Huang LW, Seow KM, Hwang JL. Spontaneous perforation of a pyometra in a postmenopausal woman with untreated cervical cancer and "forgotten" intrauterine device. Taiwan J Obstet Gynecol. 2007;46(4):439-441.
doi - Zidi YS, Bouraoui S, Atallah K, Kchir N, Haouet S. Primary in situ squamous cell carcinoma of the endometrium, with extensive squamous metaplasia and dysplasia. Gynecol Oncol. 2003;88(3):444-446.
doi - Chan LY, Lam MH, Yuen PM. Sonographic appearance of Mycobacterium pyometra mimicking carcinoma of uterine corpus. Acta Obstet Gynecol Scand. 2005;84(11):1124-1125.
doi pubmed - Razquin S, Mayayo E, Anton E, Alvira R. Squamous cell carcinoma in situ of the endometrium as superficial extension of cervical carcinoma. Gynecol Obstet Invest. 1993;35(3):190-192.
doi pubmed - Kaneko Y, Doi M, Kaibara M. Spontaneous perforation of pyometra: a case report. Asia Oceania J Obstet Gynaecol. 1994;20(3):263-267.
doi pubmed - Iwase F, Shimizu H, Koike H, Yasutomi T. Spontaneously perforated pyometra presenting as diffuse peritonitis in older females at nursing homes. J Am Geriatr Soc. 2001;49(1):95-96.
doi pubmed - Amin-Hanjani S, Good JM. Pyometra after endometrial resection and ablation. Obstet Gynecol. 1995;85(5 Pt 2):893-894.
doi - Dharmadhikari D, Dharmadhikari R, Macdonald J, Beukenholdt R. Intrauterine contraceptive device-related actinomycosis infection presenting as an incarcerated inguinal hernia. J Obstet Gynaecol Res. 2007;33(4):595-597.
doi pubmed - Kim SH, Kim SH. Modified snare technique for transvaginal intrauterine device removal in a patient with refractory cervical stenosis. J Vasc Interv Radiol. 2008;19(11):1671-1672.
doi pubmed - Tai CC, Lien WC, Wang HP, Liu KL. Early diagnosis of gas-forming pyometra in an aged patient can prevent mortality. Am J Emerg Med. 2007;25(1):126-127.
doi pubmed - Sam C, Hamid MA, Swan N. Pyometra associated with retained products of conception. Obstet Gynecol. 1999;93(5 Pt 2):840.
doi - Urushidani S, Kuriyama A. Large pyometra mimicking the bladder in an elderly female patient. J Emerg Med. 2020;58(3):e161-e163.
doi pubmed - Larkin JO, Walsh TJ, Wallis F, Waldron DJ. Pyometrium secondary to diverticular colouterine fistula. Eur J Obstet Gynecol Reprod Biol. 2011;156(2):234-235.
doi pubmed - Emergui Zrihen Y, Obreros Zegarra LP, Garcia Hernandez JA. Spontaneous uterine rupture due to pyometra, a case report. Eur J Obstet Gynecol Reprod Biol. 2017;217:182-183.
doi pubmed - Noack F, Briese J, Stellmacher F, Hornung D, Horny HP. Lethal outcome in xanthogranulomatous endometritis. APMIS. 2006;114(5):386-388.
doi pubmed - Nikkhah-Abyaneh Z, Khulpateea N, Aslam MF. Pyometra after ovum retrieval for in vitro fertilization resulting in hysterectomy. Fertil Steril. 2010;93(1):268.e261-262.
doi pubmed - Dogan-Ekici AI, Usubutun A, Kucukali T, Ayhan A. Xanthogranulomatous endometritis: a challenging imitator of endometrial carcinoma. Infect Dis Obstet Gynecol. 2007;2007:34763.
doi pubmed - Hurst N, Macht M, Travis PJ, Pierce M, Brown WW, 3rd. Postmenopausal female with abdominal pain. J Emerg Med. 2013;45(6):e221-222.
doi pubmed - Shukla PA, Kumar A, Klyde D, Contractor S. Pyomyoma after uterine artery embolization. J Vasc Interv Radiol. 2012;23(3):423-424.
doi pubmed - Yasa C, Ugurlucan FG, Yalcin O. Management of pyometra after LeFort colpocleisis resistant to drainage. Int Urogynecol J. 2016;27(4):645-646.
doi pubmed - Nakao A, Mimura H, Fujisawa K, Ezawa K, Okamoto T, Iwagaki H, Isozaki H, et al. Generalized peritonitis due to spontaneously perforated pyometra presenting as pneumoperitoneum: report of a case. Surg Today. 2000;30(5):454-457.
doi pubmed - Orum M, Fuglsang-Damgaard D, Nielsen HL. Clostridium hastiforme bacteraemia secondary to pyometra in a 64-year-old woman. BMJ Case Rep. 2017;2017:bcr2016218084.
doi pubmed - Inui A, Nitta A, Yamamoto A, Kang SM, Kanehara I, Tanaka H, Nakamura S, et al. Generalized peritonitis with pneumoperitoneum caused by the spontaneous perforation of pyometra without malignancy: report of a case. Surg Today. 1999;29(9):935-938.
doi pubmed - Choudhary D, Mohanty D, Garg PK. Pyometra: a rare cause of acute peritonitis. Surg Infect (Larchmt). 2014;15(3):354-355.
doi pubmed - Chuang CJ, Hung YC, Hsieh MC, Hsu CS. Huge asymptomatic pyometra with an intrauterine device. Taiwan J Obstet Gynecol. 2013;52(3):426-427.
doi pubmed - Izumi J, Hirano H, Yoshioka H, Takisawa J. Computed tomography findings of spontaneous perforation of pyometra. Jpn J Radiol. 2010;28(3):247-249.
doi pubmed - Yin WB, Wei YH, Liu GW, Zhao XT, Zhang MS, Hu JL, Zhang NY, et al. Spontaneous perforation of pyometra presenting as acute abdomen: a rare condition with considerable mortality. Am J Emerg Med. 2016;34(4):761.e763-765.
doi pubmed - Shayya RF, Weinstein MM, Lukacz ES. Pyometra after Le Fort colpocleisis resolved with interventional radiology drainage. Obstet Gynecol. 2009;113(2 Pt 2):566-568.
doi pubmed - Ploteau S, Renou M, Lopes P. Uterine necrosis and pyometra following surgical hemostatic Cho suture for postpartum haemorrhage: two cases. Eur J Obstet Gynecol Reprod Biol. 2012;161(2):233-234.
doi pubmed - Saha PK, Gupta P, Mehra R, Goel P, Huria A. Spontaneous perforation of pyometra presented as an acute abdomen: a case report. Medscape J Med. 2008;10(1):15.
- Geranpayeh L, Fadaei-Araghi M, Shakiba B. Spontaneous uterine perforation due to pyometra presenting as acute abdomen. Infect Dis Obstet Gynecol. 2006;2006:60276.
doi pubmed - Bagga PK, Jaswal TS, Datta U, Mahajan NC. Primary endometrial squamous cell carcinoma with extensive squamous metaplasia and dysplasia. Indian J Pathol Microbiol. 2008;51(2):267-268.
doi pubmed - Chao A, Wang AM, Wang TH, Wu TI, Chao AS. An atypical and fatal case of pyometra accompanied by the superficial spread of squamous cell carcinoma of the endometrium and the fallopian tubes. Taiwan J Obstet Gynecol. 2013;52(3):440-442.
doi pubmed - Cho MK, Kim CH, Kim YH. Primary invasive carcinoma of the vagina after Le Fort partial colpocleisis for stage IV pelvic organ prolapse: a case report. Int Urogynecol J. 2011;22(11):1459-1461.
doi pubmed - Kriplani A, Buckshee K, Relan S, Kapila K. 'Forgotten' intrauterine device leading to actinomycotic pyometra—13 years after menopause. Eur J Obstet Gynecol Reprod Biol. 1994;53(3):215-216.
doi - Kimura H, Sodani H, Takamura H, Maeda K, Kanno M, Uogishi M, Kanno S, et al. Spontaneously perforated pyometra presenting as diffuse peritonitis: report of a case. Surg Today. 1994;24(2):150-152.
doi pubmed - Chaopotong P, Benjapibal M, Thamkhantho M. Spontaneous perforation of pyometra in an elderly woman: a case report. J Med Assoc Thai. 2012;95(5):723-726.
- Roth TM. Pyometra and recurrent prolapse after Le Fort colpocleisis. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(6):687-688.
doi pubmed - Deutchman ME, Hartman KJ. Postpartum pyometra: a case report. J Fam Pract. 1993;36(4):449-452.
- Habek D. Pyometra and bilateral pyotuboovarium in an 84-year-old woman. Eur J Obstet Gynecol Reprod Biol. 2005;123(2):258-260.
doi pubmed - Chan LY, Lau TK, Wong SF, Yuen PM. Pyometra. What is its clinical significance? J Reprod Med. 2001;46(11):952-956.
- Muram D, Drouin P, Thompson FE, Oxorn H. Pyometra. Can Med Assoc J. 1981;125(6):589-592.
- Matui T, Normura H, Kato H. A case of mechanical ileus where the perforation point of the pyometra become the obstructive point- Study of the operative method for pyometra perforation. J Jpn Collag Surg. 2015;40:988-993.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
