| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Case Report
Volume 12, Number 2, August 2023, pages 65-69
Bilateral Aberrant Uterine Arteries and Clinical Significance With Uterine Embolization
Santosh Kaur Sangaria, b, Sushil Kumara, Ritwik Baidyaa, Estomih Phillip Mtuia
aDivision of Anatomy, Department of Radiology, Weill Cornell Medicine, New York, NY, USA
bCorresponding Author: Santosh Kaur Sangari, Division of Anatomy, Department of Radiology, Weill Cornell Medicine, New York, NY, USA
Manuscript submitted May 23, 2023, accepted July 1, 2023, published online August 7, 2023
Short title: Aberrant Uterine Artery
doi: https://doi.org/10.14740/jcgo883
| Abstract | ▴Top |
Uterine artery embolization (UAE) under angiographic guidance is the safe and most appropriate treatment option for the management of life-threatening intractable postpartum and gynecological bleeding when other options are not successful in controlling the hemorrhage. In most cases, the uterine artery (UA) is a direct branch of the anterior division of the internal iliac artery (IIA). It is important to be aware of the supplemental arterial supply of the uterus by aberrant UAs. Non-embolization of aberrant UAs supplying the uterus may be a major pitfall in the management of uterine bleeding. A 75-year-old female cadaver in the present study showed two UAs arising from the IIA bilaterally. The normal UA was not tortuous and was a direct branch of the anterior division of the IIA. It reached the cervix of the uterus and ascended in the broad ligament on the lateral margin of the uterus to supply it. Before the IIA was split into anterior and posterior divisions, it gave an additional tortuous branch, which directly approached the fundus of the uterus thereby supplying the superior part of the uterus, the fallopian tube and the ovary. This was the aberrant UA. The normal and aberrant UAs showed anastomosis with each other at the junction of the body of the uterus and cervix. Interventional radiologists and surgeons performing the normal UAE should be aware of this additional aberrant UA variation supplying the uterus.
Keywords: Aberrant uterine artery; Transcatheter embolization; Uterine hemorrhage; Cadaveric study
| Introduction | ▴Top |
Endovascular intervention is the most important treatment of postpartum/gynecologic bleeding these days. The various sophisticated techniques in transcatheter embolization have become the treatment of choice for the management of uterine bleeding due to various causes including postpartum hemorrhage, menorrhagia and leiomyoma of the uterus. It has become an alternative to surgery as well [1, 2]. Interventional radiologists have expanded their role in the management of various causes of uterine bleeding. Transcatheter embolization has become the most appropriate minimally invasive technique as an alternative to surgeries like hysterectomy. This also saves the patient with an ability to future pregnancies [3]. The present case reports a unique variation in the arterial supply of the uterus, which might be encountered during surgical procedures resulting in clinical implications.
| Case Report | ▴Top |
The observations were made during a regular dissection course in the gross anatomy lab of the medical college. A 75-year-old female cadaver died of cardiopulmonary arrest. The detailed medical history was not available.
During the dissection of the pelvis, the mid-sagittal section of the pelvis was performed through the pubic symphysis (PS) anteriorly and midline cut through the lower lumbar vertebrae, sacrum and coccyx. The branches of the internal iliac artery (IIA) were dissected on both sides. The internal iliac vein and its tributaries were separated and dissected out to clearly expose the branches of the IIA. The connective tissue around the branches of the IIA was removed thoroughly. The dissection showed that the IIA was divided into two divisions, i.e., anterior and posterior. The IIA gave origin to two uterine arteries (UAs). One UA followed a normal course on both sides. It was a direct branch of the anterior division of the IIA and was not tortuous. From its origin, it approached the cervix of the uterus, gave vaginal branches and ascended on the lateral margin of the uterus. This normal UA had the most commonly seen relationship with the ureter crossing below the UA (water under the bridge), by the side of the cervix (Fig. 1).
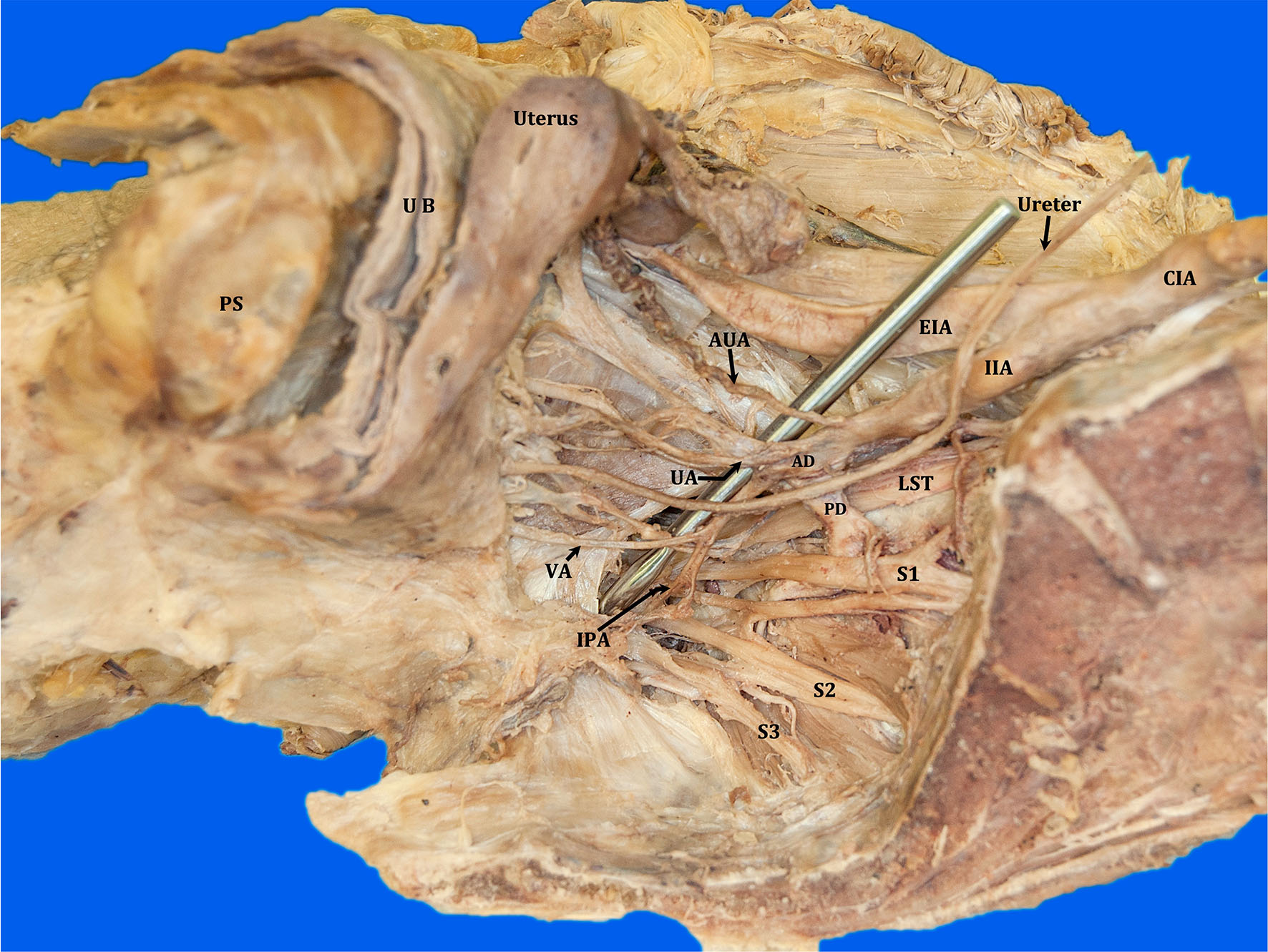 Click for large image | Figure 1. Midsagittal section of pelvis showing the branches of IIA. The arrows point to the two uterine arteries supplying the uterus: UA, AUA, CIA, EIA, PD, AD, PS, UB, VA, IPA, LST, S1, S2 and S3 nerves. IIA: internal iliac artery; UA: uterine artery; AUA: aberrant uterine artery; CIA: common iliac artery; EIA: external iliac artery; PD: posterior division of IIA; AD: anterior division of IIA; PS: pubic symphysis; UB: urinary bladder; VA: vaginal artery; IPA: internal pudendal artery; LST: lumbosacral trunk; S1: ventral rami of first sacral; S2: second sacral; S3: third sacral nerves. |
Before the IIA was divided into anterior and posterior divisions, it gave an additional tortuous artery, which was seen running in the broad ligament along with a tortuous vein directly towards the fundus of the uterus bilaterally. It was divided into branches to supply the uterus, the fallopian tube and the ovary. This was the aberrant UA (Figs. 1, 2). The ovarian artery followed a normal course on both sides, arising from the abdominal aorta to the suspensory ligament/infundibulopelvic ligament of the ovary to supply the ovary and the fallopian tube. Both the normal and the aberrant UAs were seen anastomosed with each other at the junction of the body of the uterus and cervix.
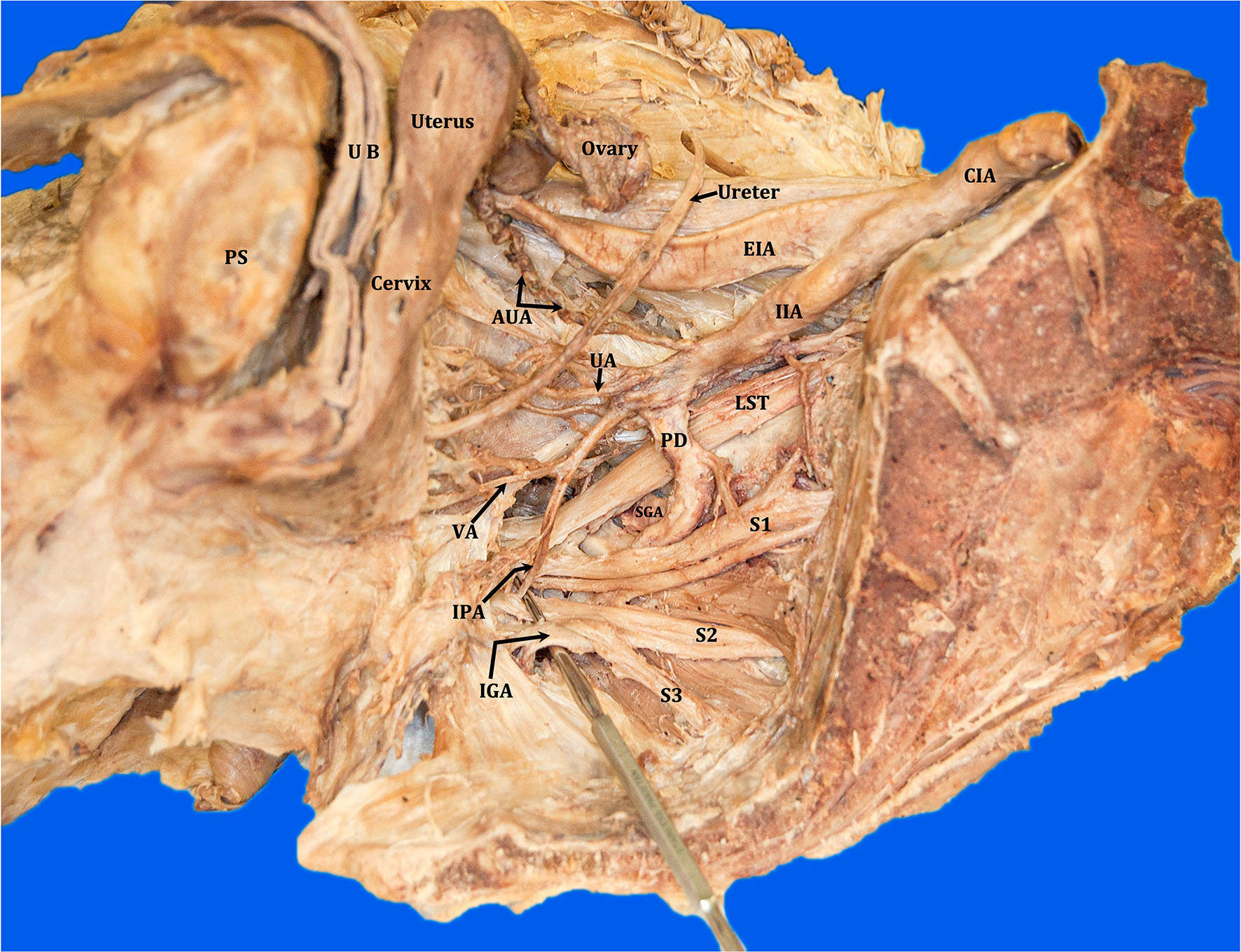 Click for large image | Figure 2. Midsagittal section of the pelvis showing the IGA arising from the PD, SGA, IIA, CIA, EIA, PS, UB. The arrows point to the two uterine arteries supplying the uterus: UA, AUA. VA, IPA, LST, S1, S2 and S3 nerves. IGA: inferior gluteal artery; PD: posterior division of the IIA; SGA: superior gluteal artery; IIA: internal iliac artery; CIA common iliac artery; EIA: external iliac artery; PS: pubic symphysis; UB: urinary bladder; UA: uterine artery; AUA: aberrant uterine artery; VA: vaginal artery; IPA: internal pudendal artery; LST: lumbosacral trunk; S1: ventral ramus of first sacral nerve; S2: ventral ramus of second sacral nerve; S3: ventral ramus of third sacral nerve. |
Figure 2 shows the IIA branches and their relationship with the ventral rami, ventral rami of first sacral (S1), second sacral (S2) and third sacral (S3) nerves and the lumbosacral trunk (LST) (formed by ventral rami of fourth lumbar (L4) and fifth lumbar (L5) spinal nerves). In this case, the inferior gluteal artery was a continuation of the posterior division of the IIA, a commonly seen variation.
Figure 3 shows midsagittal section of the different donors showing the distribution of normal UA branching directly from the anterior division of IIA for comparison. It is important to note that this normal UA had the most commonly seen relationship with the ureter crossing below the UA (water under the bridge), by the side of the cervix. It does not show any aberrant UA supplying the uterus. It is also important to note that in this case, the inferior gluteal artery is a direct branch of the anterior division of the IIA normally seen in most of the cadavers.
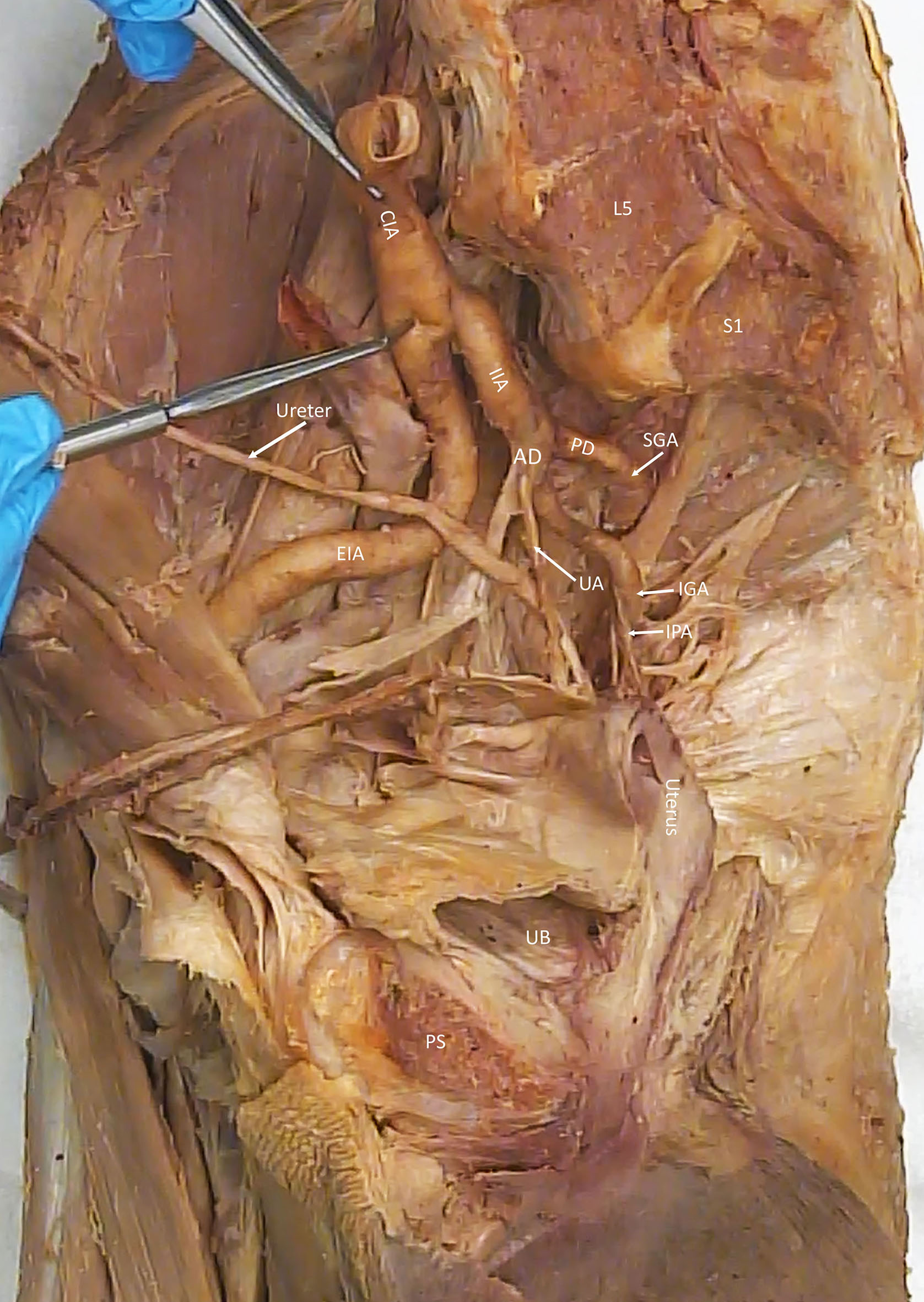 Click for large image | Figure 3. Midsagittal section of right pelvis from a donor showing normal UA for comparison. CIA, EIA, IIA, PD, AD, SGA, IGA, IPA, PS, UB, L5, S1. CIA: common iliac artery; EIA: external iliac artery; IIA: internal iliac artery; PD: posterior division of IIA; AD: anterior division of IIA; SGA: superior gluteal artery; IGA: inferior gluteal artery; IPA: internal pudendal artery; PS: pubic symphysis; UB: urinary bladder; L5: fifth lumbar vertebra; S1: first piece of sacrum. |
| Discussion | ▴Top |
Pelvic arterial embolization has undergone a number of advances and plays an important role in the management of obstetric hemorrhage. UAE is a successful and appropriate procedure for the control of postpartum hemorrhage [4]. Complete knowledge of the blood supply of the uterus is important for the management of uterine bleeding. When conservative measures do not work, it is important to pursue arterial embolization in treating postpartum hemorrhage [5].
In one of the common important variations, the aberrant UA may arise from the ovarian artery. In this case, UAE will result in a total failure [6]. Identification of all the variations in the branching pattern of the IIA is important to avoid untargeted embolization.
Most commonly, the UA arises from the anterior division of the IIA in 51% of cases [7]. According to another investigator, in 62.7% of cases, it has been reported that the UA may arise from the IIA via a common trunk with the umbilical artery. In 25.6% of cases, the UA is a direct branch of the IIA, in 9.3% of cases as a branch of the superior gluteal artery, and in 2.3% of cases as a branch of the internal pudendal artery (IPA) [8]. The UA commonly arises from internal iliac, umbilical or inferior gluteal arteries [9].
UA has been reported to originate directly from the abdominal aorta in close proximity to the origin of the ovarian artery [10]. The UA can also be replaced by the artery of the round ligament of uterus arising from the inferior epigastric artery [11].
The present case reports two UAs arising from the IIA. In addition to the normal UA, an aberrant UA arises from the IIA bilaterally. The aberrant UA was tortuous, accompanied by a tortuous vein. From its origin, it directly approached towards the fundus of the uterus and divided into branches to supply the uterus, the fallopian tube and the ovary. It is possible that the UA following the normal course supplies the inferior part of the uterus and vagina and the aberrant UA which directly reaches the fundus of uterus is responsible for mainly supplying the superior part of the uterus and fallopian tubes. Interventionists performing the normal UAE may not be successful in stopping obstetrical or gynecological bleeding and should be aware of such an additional aberrant UA as a complementary blood supply to the uterus.
The interventional radiologist should be aware of the arterial supply of the uterus by normal and the aberrant UA variations. While doing transcatheter UAE, the clinician has to be vigilant for the identification of the arteries supplying the uterus and embolize normal and aberrant UAs carefully for successful treatment of uterine hemorrhage.
This anomalous blood supply of the uterus also needs special attention during uterine surgeries.
Conclusions
Transcatheter embolization of UAs may not be able to control obstetric or gynecological bleeding due to the presence of aberrant UAs. This study reports two UAs supplying the uterus bilaterally. One UA which was a direct branch of the anterior division of the IIA followed a normal course, whereas an additional tortuous branch arose directly from the IIA with an accompanying tortuous vein and was seen to be directly passing towards the fundus of the uterus. Detailed knowledge of the anatomical variations of the UA is essential for the management of UAE and uterine surgeries. It is important to note that in general, the UAE or hysterectomy is used for the treatment of postpartum and gynecological hemorrhage, when other modes of treatment are not successful and the patient had already considerable blood loss. The clinician should be able to identify and be aware that aberrant arteries supplying the uterus are of critical importance and failure to do so can lead to further blood loss, failure of the procedure, or death if not treated quickly.
Learning points
For the management of postpartum/gynecological bleeding and uterine surgeries, surgeons should be aware of the variations in the arterial blood supply to the uterus by the aberrant UAs. In addition to the number of variations available in the literature, this study is a unique variation of the two UAs branching from the IIA on both sides to supply the uterus by two different routes. One UA follows a normal course whereas the aberrant tortuous UA directly reaches the fundus of uterus. The presence of aberrant UA reaching the fundus of uterus directly would be a potential cause of treatment failure during UAE and during surgery to avoid massive bleeding. For successful management of uterine bleeding, Doppler ultrasound studies and UA color imaging would be helpful to evaluate the distribution of the normal and aberrant UAs, UA blood flow and mean arterial pressure before undergoing UAE or any uterine surgery including hysterectomy.
Acknowledgments
All the authors would like to acknowledge the female donor, without whom the study would not have been possible. The authors would also like to thank our lab manager Crandell Warner and lab technician Jaswill Tejeda for taking care of the donors in the gross anatomy lab.
Financial Disclosure
The authors received no external financial support for the research, authorship and/or publication of this article. This project was supported by the Division of Anatomy, Weill Cornell Medicine.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Informed Consent
Our donation program requires the living donors to complete and sign an affidavit or if after death, by the next of kin or executor. The affidavit indicates the desire to donate the body to the medical college. It also indicates that the body will be used for the purposes of health science education, health science research and publication or in the advancement of medical therapy. In addition, the affidavit has to be signed by two witnesses before submission to our donation program.
Author Contributions
Santosh Sangari: dissection, observations, interpretation, photography, drafting and editing of the manuscript. Sushil Kumar and Ritwik Baidya: observations, labeling of figures, editing and revising of the manuscript. Estomih Mtui: provision of anatomical specimens, observation, editing and revising of the manuscript.
Data Availability
Data generated during the current case are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Pelage JP, Le Dref O, Mateo J, Soyer P, Jacob D, Kardache M, Dahan H, et al. Life-threatening primary postpartum hemorrhage: treatment with emergency selective arterial embolization. Radiology. 1998;208(2):359-362.
doi pubmed - Pelage JP, Soyer P, Repiquet D, Herbreteau D, Le Dref O, Houdart E, Jacob D, et al. Secondary postpartum hemorrhage: treatment with selective arterial embolization. Radiology. 1999;212(2):385-389.
doi pubmed - Salazar GM, Petrozza JC, Walker TG. Transcatheter endovascular techniques for management of obstetrical and gynecologic emergencies. Tech Vasc Interv Radiol. 2009;12(2):139-147.
doi pubmed - Gonsalves M, Belli A. The role of interventional radiology in obstetric hemorrhage. Cardiovasc Intervent Radiol. 2010;33(5):887-895.
doi pubmed - Greenwood LH, Glickman MG, Schwartz PE, Morse SS, Denny DF. Obstetric and nonmalignant gynecologic bleeding: treatment with angiographic embolization. Radiology. 1987;164(1):155-159.
doi pubmed - Matson M, Nicholson A, Belli AM. Anastomoses of the ovarian and uterine arteries: a potential pitfall and cause of failure of uterine embolization. Cardiovasc Intervent Radiol. 2000;23(5):393-396.
doi pubmed - Gomez-Jorge J, Keyoung A, Levy EB, Spies JB. Uterine artery anatomy relevant to uterine leiomyomata embolization. Cardiovasc Intervent Radiol. 2003;26(6):522-527.
doi pubmed - Arfi A, Arfi-Rouche J, Barrau V, Nyangoh Timoh K, Touboul C. Three-dimensional computed tomography angiography reconstruction of the origin of the uterine artery and its clinical significance. Surg Radiol Anat. 2018;40(1):85-90.
doi pubmed - Liapis K, Tasis N, Tsouknidas I, Tsakotos G, Skandalakis P, Vlasis K, Filippou D. Anatomic variations of the Uterine Artery. Review of the literature and their clinical significance. Turk J Obstet Gynecol. 2020;17(1):58-62.
doi pubmed pmc - Redlich A. Die verwendung der x-strahlen fur das studium des arteriellen systems der inneren weiblichen genitalien. Arch Anat u Physiol. 1909;33:357.
- Saraiya PV, Chang TC, Pelage JP, Spies JB. Uterine artery replacement by the round ligament artery: an anatomic variant discovered during uterine artery embolization for leiomyomata. J Vasc Interv Radiol. 2002;13(9 Pt 1):939-941.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
