| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Case Report
Volume 12, Number 3, December 2023, pages 93-97
The C-Arm Technique to Locate a Lost Needle During Robotic Gynecology Surgery
Emily Nguyena, c , Jennifer Ferraroa
, Sam Siddighib
aDivision of Obstetrics and Gynecology, Riverside Community Medical Center, Riverside, CA, USA
bFemale Pelvic Medicine and Reconstructive Surgery, Loma Linda University Health Care, Loma Linda, CA, USA
cCorresponding Author: Emily Nguyen, Department of Obstetrics and Gynecology, Riverside Community Hospital, Riverside, CA 92501, USA
Manuscript submitted September 8, 2023, accepted October 19, 2023, published online December 28, 2023
Short title: Finding a Lost Needle
doi: https://doi.org/10.14740/jcgo910
| Abstract | ▴Top |
The loss of a needle during robotic surgery can be a potentially harmful medical event, especially if retained. While the occurrence of such an event is uncommon, loss of a needle can cause a significant challenge to find and retrieve. Failure to find a lost needle can also have tremendous medicolegal consequences, as a result, this issue is classified as a “never event”. There is currently no standardized process for finding a lost needle during a robotic gynecologic operation. The objective of this report was to review the current literature on lost surgical needles and present a case that utilized a mobile C-arm fluoroscopy to triangulate a lost needle during robotic surgery. Although the use of C-arm fluoroscopy has been noted in the literature, the technique has not been described in detail. We describe a safe and efficient way to find lost needles intraoperatively that can be integrated into a standardized protocol.
Keywords: Foreign bodies; Laparoscopy; Minimally invasive surgery; Needle loss; Robotic
| Introduction | ▴Top |
Although the incidence of lost instruments is low, approximately 0.06-0.11%, robotic surgery seems to have a higher risk of losing a needle than laparoscopic surgery. The Joint Commission has made an Advisory Statement regarding an increase of retained foreign bodies during robotic surgery and recommended that standardized processes be implemented [1]. Greater than 80% of needles are lost during retrieval. Losing a needle is significant because it may result in injury to the patient, prolongs operative time, increases surgeon anxiety, and may have exorbitant medicolegal consequences [2]. Various authors have suggested algorithms for prevention of needle loss and for finding a lost needle; however, none explained the best technique to radiographically locate a lost needle during robotic surgery.
There are several disadvantages to currently recommended intraoperative “radiographs” for identification of a lost needle. A plain abdominal X-ray done in the operating room may only find 29% of lost needles, especially if the needle is between 4 and 10 mm [3]. The plain X-ray has a higher chance of incomplete field visualization and may miss a needle if it overlaps intestinal gas or fecal matter. Additionally, to obtain a plain X-ray in the operating room, the patient will need to be lifted off the operating table in order to place a plate underneath the patient to capture X-rays. This repositioning leads to loss of the sterile surgical field and prolongation of operative time. Moreover, repositioning of the patient will often shift the needle further away from the surgical field and increase the difficulty of retrieval [4].
We present a case where fluoroscopy was used to successfully find a lost needle during a robotic sacrocolpopexy without having to move the patient and disrupt the sterile field. Based on our experience, we propose a new standardized protocol utilizing this method to find a lost needle.
| Case Report | ▴Top |
Investigations
A 32-year-old female presented to our hospital for a robotic supracervical hysterectomy and robotic sacrocolpopexy due to pelvic organ prolapse. During the surgery, a TH-18 needle (17 mm) was lost upon attempted retrieval of the needle through the right upper quadrant assistant port. The assistant used a needle holder to grasp the Gore-Tex CV3 suture near the needle swage. Upon retrieval, the needle was caught on the port and was displaced into the abdominopelvic cavity.
Diagnosis
The surgical assistant and surgeon immediately noted the missing needle. A thorough search of the operating room, operative field, as well as the trocars, especially the assistant port, was undertaken by both the registered nurse first assistant (RNFA) and the circulating nurse. The operating room staff conducted a search of the area while taking care to maintain the sterile field and avoid moving the patient, equipment on or near the operating table, or the patient’s bed in order to avoid potentially moving the needle more. Meanwhile, the surgeon manipulated the da Vinci camera to conduct a systematic visual search of the top of the viscera and lateral edges of the abdominal cavity. Since the patient was in Trendelenburg, the surgeon started the search in the upper quadrants where the needle was most likely to fall due to gravity and then moved in a clockwise fashion to survey all four abdominal quadrants and pelvis. The surgeon did not attempt to manipulate the bowel to avoid disrupting the needle and causing unforeseen injury to other structures.
Treatment
After the initial search was unsuccessful, the decision was then made to utilize fluoroscopic imaging to locate the needle. In preparation, the robot was undocked, and all trocars were left in place. A mobile C-arm was then positioned over the upper abdomen while maintaining the sterile field. A hemostat was placed on the abdomen to serve as a maker to localize the lost needle. Anteroposterior (AP) and lateral images of the upper and lower abdomen as well as the pelvis were obtained using one pulse per second to precisely locate the lost needle; by using different AP and lateral angles, the surgeon was able to configure an approximate three-dimensional location the needle was located in. The hemostat was moved, and additional images were taken as needed for better localization. With this technique we were able to locate the TH-18 needle in an efficient manner in the left lower pelvis (Fig. 1a, b). We then re-docked the robot and retrieved the needle, which was in the left rectovaginal space, as identified on imaging. Once the needle was found, we finished the operation with no further “adverse” events.
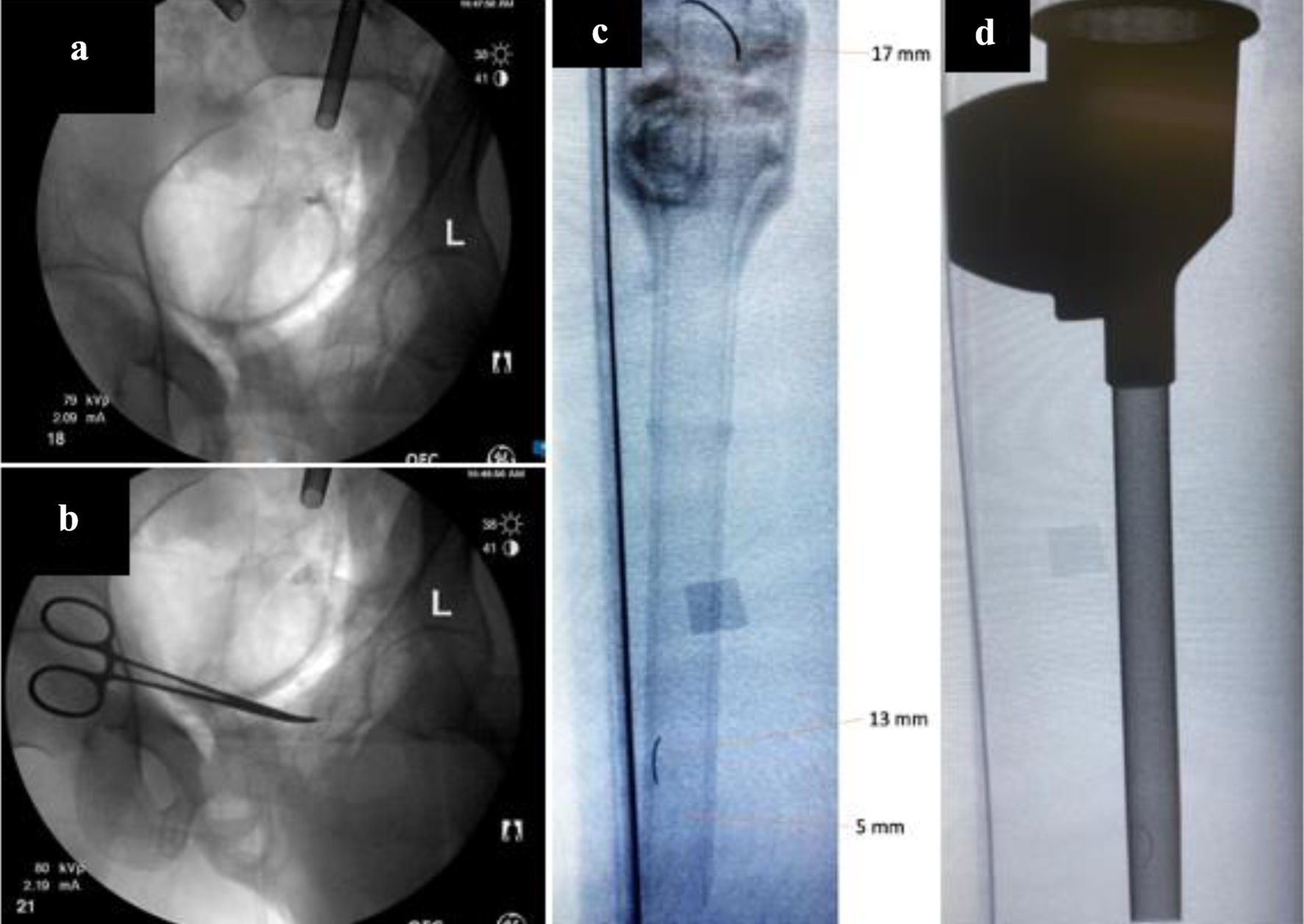 Click for large image | Figure 1. (a) Needle found in pelvis. (b) Hemostat used to triangulate needle. (c) A 17-mm, 13-mm, and 5-mm needle in a standard 8-mm trocar. (d) A 13-mm needle in a metallic laparoscopic trocar. |
Follow-up and outcomes
The needle was retrieved from the patient’s abdomen and the rest of the operation was completed. By using the mobile C-arm, we were able to avoid contamination of the operative field and avoid repositioning the patient. Overall, the needle was found in a safe, time-efficient manner. The patient was not subjected to any excessive radiation, nor did she experience any injury to her nearby organs during this incident.
| Discussion | ▴Top |
The loss of a needle during laparoscopic or robotic surgery presents a complex and potentially dangerous situation for the surgeon, the surgical team, and the hospital system. While retrieval of a needle in any surgical case presents a challenge, retrieval is made even more challenging in cases employing minimally invasive techniques due to the limited visual field of the camera, the smaller size of needles used, greater difficulty manipulating structures, and lack of the tactile sensation of open surgery. Most guidelines regarding lost surgical instruments and needles are aimed at prevention of misplacing these surgical items. Though there are no specific guidelines, the usual protocol for locating a lost needle involves a visual search and then subsequent intraoperative imaging such as an abdominal X-ray [5]. However, there is currently no consensus in current literature on how best to manage a retained or lost needle during a laparoscopic or robotic procedure.
There have been various case reports and proposals on how to best manage a lost item during laparoscopic and robotic procedures. Ostrzenski et al proposed using abdominal radiographs and radiopaque threads to create a “net” on the abdomen and metallic instruments to help localize and retrieve the missing needle without having to convert to open surgery [6]. In another case report, Kandioler-Eckersberger et al described using a magnetic probe to recover broken metallic pieces during laparoscopy [7]. Furthermore, Gulack et al proposed an algorithm that utilizes the C-arm and plain films to standardize management. However, the details of the C-arm procedure were not described [8]. Based on a survey of minimally invasive surgeons, Jayadevan et al proposed a similar protocol that incorporated a visual survey of the abdomen, intraoperative fluoroscopy radiography, port inspection, and a quadrant-based systematic visual search for the recovery of needles [9]. None of these proposed algorithms describe their fluoroscopic technique when retrieving the lost item. To the best of our knowledge, our case report is the first to describe how best to utilize fluoroscopy to recover a lost needle during robotic surgery. We propose a new protocol for the recovery of needles lost during abdominal and pelvic minimally invasive surgery (Fig. 2).
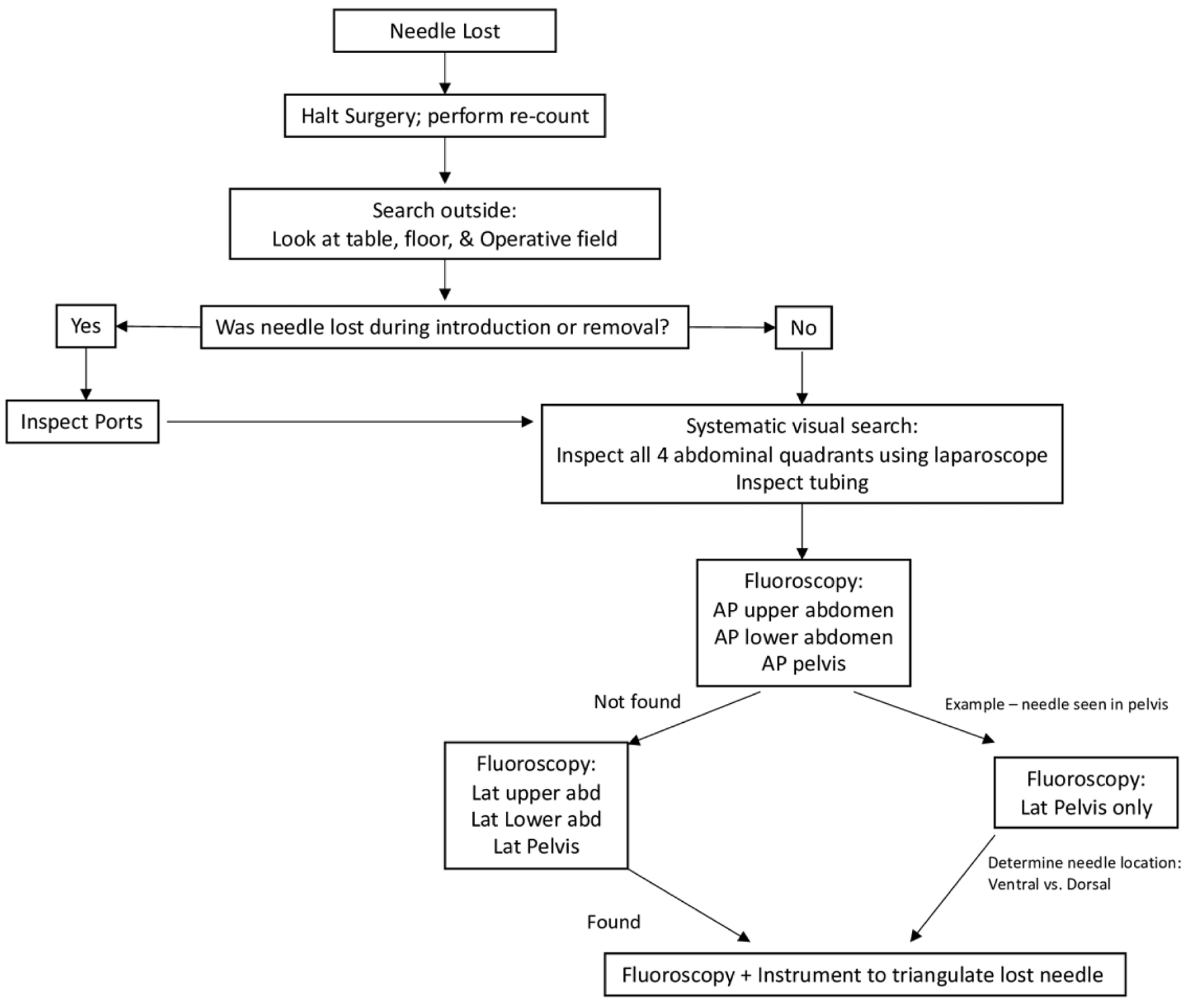 Click for large image | Figure 2. A flow diagram of proposed protocol of surgical needle lost during minimally invasive surgery. Each step assumes failure to find the needle during the prior step. |
Under current circumstances, obtaining a radiograph on a patient undergoing robotic surgery involves undocking the robot, repositioning the surgical table, removing trocars, lifting the patient in order to place an X-ray plate, and finally taking a radiographic picture and waiting for the radiologist to interpret. When the patient is lifted off the table, there is a high probability that the sterile surgical field will be compromised. If the radiologist or surgeon can identify the lost needle in the abdominopelvic cavity, then the surgical team must attempt to find where it is located by using a two-dimensional X-ray image.
Efficient recovery of misplaced needles is imperative for the safety of the patient as well as limiting high operating costs; one study calculated that the average operating room time is $36-37 per minute using financial data from California’s fiscal year in 2014 [10]. We advocate for our fluoroscopic technique because not only does it have a higher probability of identifying the lost needle, but it also avoids moving the patient and all the disadvantages discussed above, thereby limiting operating room time, and saving on cost.
Limitations with intraoperative plain radiographs include inadequate imaging evaluation due to overlapping images from bowel gas and fecal matter and decreased detection rate with smaller size of the needle [4]. The C-arm allows for different angles to help overcome that limitation and provides better visualization of the lost object. As demonstrated in Figure 1c and d, a 13-mm and 17-mm easily can be identified both inside a regular 8-mm laparoscopic trocar as well as inside the metallic robotic trocar. In obtaining these photos, we had to utilize different angles using fluoroscopy to best visualize the needles. This is another advantage of fluoroscopy as the various angles allow for identification of the needle even in the presence of gas or intestinal stool. On the other hand, while the C-arm allows for visualization of the object from multiple angles, the C-arm is not able to produce a three-dimensional image. As a result, the surgeon may spend a while searching in the expected area with bowel in the way. Prior studies have suggested that the surgical team can use a hemostat or other radiopaque object (such as staples) to place on either the lateral or AP surface of the patient in order to help identify the plane of the needle in the three-dimensional abdominal space [11, 12]. This technique may be able to circumvent the limitations caused by the two-dimensional nature of C-arm images. While our case was able to identify the needle’s location in an area away from the bowel, it is conceivable that if images show that the needle is found in a bowel occupying area, it may be appropriate to run the bowel. By collecting imaging beforehand, we were able to identify the needle’s location without having to unnecessarily run the bowel in this situation. Furthermore, it is difficult to see a 5-mm needle even with fluoroscopy. Our technique utilizes lower levels of radiation. Typically, fluoroscopic pulse rates are between 15 and 30 pulses per second, but our choice of 1 pulse/second allowed for localization without subjecting the patient or staff (i.e., scatter radiation) to a higher radiation dose. We were able to use a hemostat clamp along with our fluoroscopic intraoperative technique to efficiently triangulate the lost needle (Fig. 1a, b).
Learning points
Our case demonstrates the dilemma a robotic-assisted surgeon can face when a needle is lost. This case emphasizes the importance of special care when extracting the needle to prevent the tip of the needle from catching the port, dislodging from the grasper, and getting lost in the abdominopelvic cavity. Overall, precautions for handling needles during minimally invasive surgery are important. Best practice should continue to be aimed at prevention with proper communication of the surgical team; however, a standardized approach to locating a lost needle should be created to increase the likelihood of needle recovery and decrease time spent during the recovery procedure.
Acknowledgments
The authors would like to anonymously acknowledge the patient on whom the case report is based.
Financial Disclosure
The authors have no financial funding or relationships to disclose.
Conflict of Interest
The authors have no conflict of interest relevant to this article.
Informed Consent
Informed consent was obtained from this patient for publication of this case report and any accompanying images.
Author Contributions
Emily Nguyen, MD helped with conception and design, drafting, and critical revisions of this manuscript. Jennifer Ferraro, MD helped with drafting and revisions of this manuscript. Sam Siddighi, MD supervised and helped with conception and design, drafting, and critical revisions of this manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Sentinel Event Alert 51: Preventing unintended retained foreign objects [Internet]. Jointcommission.org. 2023 [cited Apr 24, 2023]. Available from: https://www.jointcommission.org/resources/sentinel-event/sentinel-event-alert-newsletters/sentinel-event-alert-issue-51-preventing-unintended-retained-foreign-objects/#.ZEbIcuzMI6A.
- Barto W, Yazbek C, Bell S. Finding a lost needle in laparoscopic surgery. Surg Laparosc Endosc Percutan Tech. 2011;21(4):e163-165.
doi pubmed - Ponrartana S, Coakley FV, Yeh BM, Breiman RS, Qayyum A, Joe BN, Poder L, et al. Accuracy of plain abdominal radiographs in the detection of retained surgical needles in the peritoneal cavity. Ann Surg. 2008;247(1):8-12.
doi pubmed - Contegiacomo A, Conti M, Trombatore P, Dezio M, Muciaccia M, Lozupone E, Natale L, et al. Radiological features and management of retained needles. Br J Radiol. 2020;93(1114):20200316.
doi pubmed pmc - Goldberg JL, Feldman DL. Implementing AORN recommended practices for prevention of retained surgical items. AORN J. 2012;95(2):205-216.
doi pubmed - Ostrzenski A. An intraoperative method of localizing a missing piece of a broken laparoscopic instrument. Am J Obstet Gynecol. 1997;176(3):726-727.
doi pubmed - Kandioler-Eckersberger D, Niederle B, Herbst F, Wenzl E. A magnetic probe to retrieve broken metallic parts of instruments during laparoscopic procedures. Surg Endosc. 2002;16(1):208-209.
doi pubmed - Gulack BC, Skertich NJ, Sullivan GA, Shah AN, Zani A. The lost suture needle: An algorithm to standardize management and improve outcomes. J Pediatr Surg. 2021;56(11):2128-2129.
doi pubmed - Jayadevan R, Stensland K, Small A, Hall S, Palese M. A protocol to recover needles lost during minimally invasive surgery. JSLS. 2014;18(4):e2014.00165.
doi pubmed pmc - Childers CP, Maggard-Gibbons M. Understanding costs of care in the operating room. JAMA Surg. 2018;153(4):e176233.
doi pubmed pmc - Lynch CM, Powers AK. Management of a broken needle at the time of laparoscopic burch. JSLS. 2000;4(3):275-276.
pubmed pmc - Zaman S, Clarke R, Schofield A. Intraoperative loss of a surgical needle: a laparoscopic dilemma. JSLS. 2015;19(2):e2013.00401.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
