| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Case Report
Volume 12, Number 3, December 2023, pages 98-101
Multiple Spontaneous Fractures in Pregnancy
Abigail Immanuela, b, c, Pamela Taxela
aSchool of Medicine, University of Connecticut, Farmington, CT 06030, USA
bPrimary Care Internal Medicine Residency Program, University of Connecticut, Farmington, CT 06030, USA
cCorresponding Author: Abigail Immanuel, School of Medicine, University of Connecticut, Farmington, CT 06030, USA
Manuscript submitted September 30, 2023, accepted November 22, 2023, published online December 28, 2023
Short title: Multiple Spontaneous Fractures in Pregnancy
doi: https://doi.org/10.14740/jcgo915
| Abstract | ▴Top |
Pregnancy-associated osteoporosis and skeletal metastases due to rectal carcinoma are both unusual causes of spontaneous fractures. We present the case of a pregnant patient diagnosed with stage IIIB rectal carcinoma at 18 weeks of gestation who developed several spontaneous sacral fractures. This case illustrates the need to evaluate the etiology of spontaneous fractures during pregnancy in the setting of a locally advanced cancer, as the diagnosis of pregnancy-associated osteoporosis in late pregnancy and early post-partum should be considered.
Keywords: Osteoporosis; Pregnancy; Rectal carcinoma
| Introduction | ▴Top |
Though relatively rare, pregnancy-associated osteoporosis is a condition that has been associated with thoracolumbar and sacral fractures. The process of fetal skeletal development requires a significant amount of calcium from maternal sources which may place the mother at risk of decreased bone mineral density and consequent fractures. We present the case of a pregnant patient with spontaneous bilateral sacral fractures in the setting of stage IIIB rectal cancer, presenting the diagnostic challenge of metastatic disease versus pregnancy-associated osteoporosis.
| Case Report | ▴Top |
A 35-year-old G6P1 female at 18 weeks of gestation underwent noninvasive prenatal testing and was found to have abnormal results suggestive of monosomy 18. The test also detected the presence of malignant cells. The patient was offered amniocentesis and chorionic villus sampling to determine if the fetal karyotype was consistent with monosomy 18 but declined. Given the concern for malignancy, the patient underwent a magnetic resonance imaging (MRI) of the chest, abdomen, and pelvis which revealed bilateral lymphadenopathy in the pelvis, right upper rectal wall thickening, and a 13 mm nodule along the right rectum. A biopsy revealed infiltrating ulcerated adenocarcinoma, and the patient was diagnosed with stage IIIB, T3 N1 M0 rectal cancer of the proximal rectum.
For the next 3 months, the patient received seven out of eight cycles of neoadjuvant chemotherapy with FOLFOX (folinic acid, fluorouracil, and oxaliplatin) and was unable to complete the final cycle due to the delivery of her baby. Seven weeks into the treatment course at 28 weeks of gestation, a repeat MRI revealed improvement of the rectal wall thickening, stable to slightly decreased pelvic lymph node size, and a new nondisplaced incomplete fracture of the inferior portion of the right sacrum. Due to concern for metastatic disease, an MRI was performed and did not demonstrate a clear osseous lesion in the area.
After her initial fracture, the patient was referred to the Cancer and Bone Health Clinic at 29 weeks of pregnancy. Upon evaluation, she reported no acute fall or trauma. She walked on the treadmill 1 h daily for exercise and had noticed a dull pain in the right gluteal region that began several weeks prior to fracture diagnosis. She attributed this to her pregnancy as she could not identify a clear inciting event for the pain. The patient was taking prenatal vitamin, 2,000 IU of vitamin D daily, and low-dose calcium carbonate tablets twice daily since learning of her fracture in an effort to increase calcium intake as her dietary intake was limited. Her past medical history included hypertension, asthma, allergic rhinitis, eczema, and polycystic ovarian syndrome. The patient’s past obstetrical history included a delivery at 39 weeks with in vitro fertilization (IVF) complicated by hypertension and gestational diabetes. Menarche was at age 15 years, and she had oligomenorrhea throughout her reproductive years. She had no prior fractures other than during childhood related to sports and activities. There was a family history of osteoporosis in a maternal grandmother and osteopenia in her mother.
On physical examination, the patient was a well-appearing pregnant female. Her body mass index (BMI) was 32.8 kg/m2. She denied any significant history of tobacco or alcohol use. Her medications included a steroid inhaler used rarely for asthma. Laboratory evaluation revealed normal serum calcium but showed a bone-specific alkaline phosphatase of 21 U/L (normal: 11 - 29) and moderately elevated urine N-telopeptide cross-links (NTx) of 57 nM BCE/mM creatinine (normal: 17 - 94 nM BCE/mM), suggestive of high bone turnover, which has been shown in the third trimester of pregnancy [1]. Vitamin D level was 48 ng/mL (normal: 30 - 80 ng/mL). The patient was counseled to significantly increase her total calcium intake to 1,200 - 1,500 mg/day, given the high fetal demands during the third trimester and to continue taking adequate vitamin D.
Two weeks later at a routine prenatal visit, the patient reported left-sided low back and sacral pain, which was exacerbated by movement, resulting in limited ambulation. This pain felt similar to the right-sided sacral pain she experienced previously with her initial fracture. This raised concern for a second insufficiency fracture which was confirmed when an MRI showed a stress fracture of the left sacral ala along with subtle progression of the preexisting right sacral fracture with no definitive evidence of osseous metastatic disease, supporting the diagnosis of pregnancy-associated osteoporosis (Fig. 1).
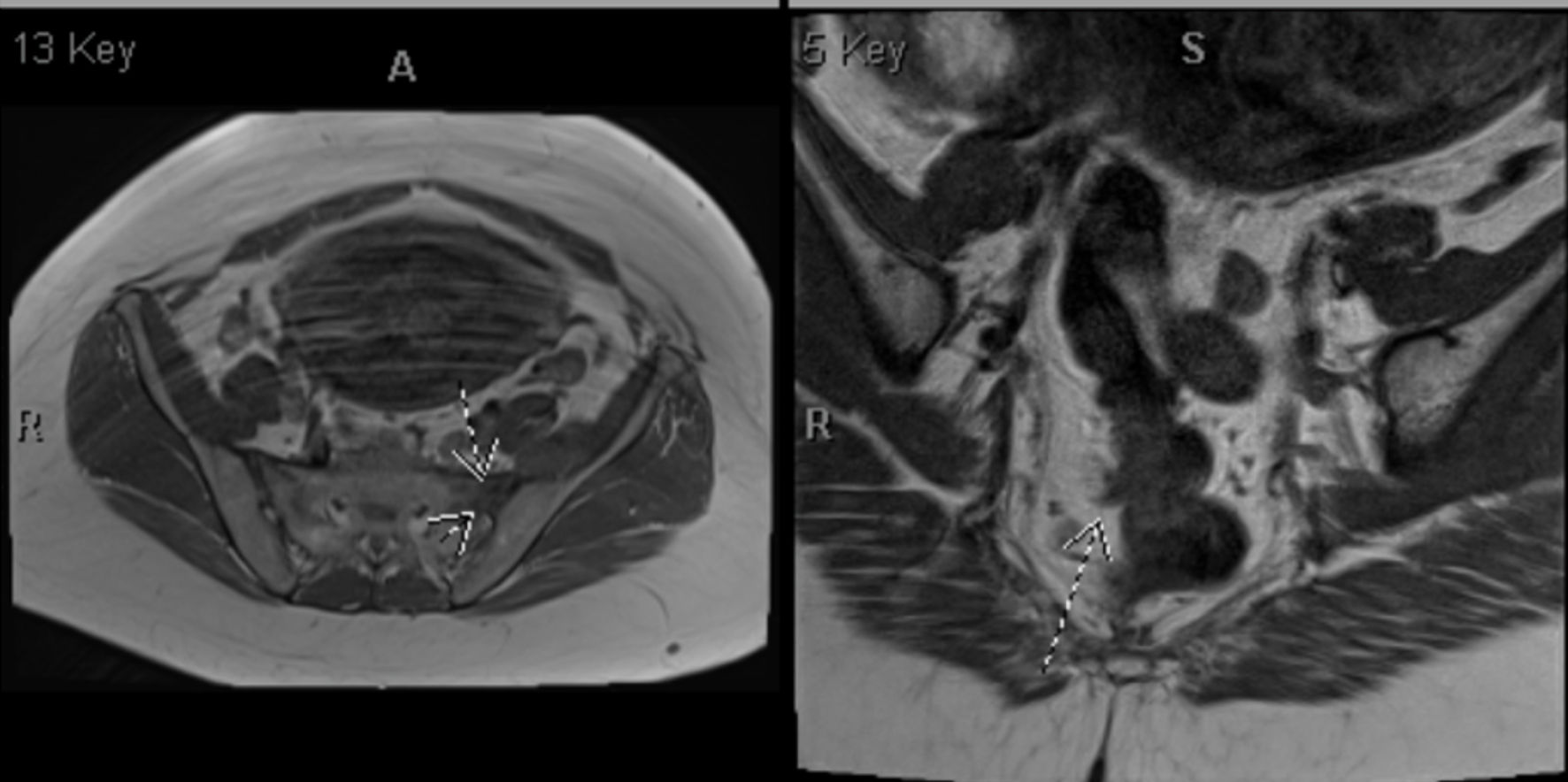 Click for large image | Figure 1. MRI of the pelvis without contrast demonstrating the development of edema within the left sacral ala (arrows in left panel) along with associated areas of decreased signal on T1-weighted images, consistent with developing stress fracture. No evidence of osseous metastatic disease is present. The right panel shows a solid rectal mass along the right anterior rectal wall (arrow) with adjacent abnormal lymph nodes. MRI: magnetic resonance imaging. |
During her final month of neoadjuvant therapy, the patient was induced and gave birth via cesarean section to a healthy boy at 35 weeks. A restaging MRI the following month revealed stable rectal wall thickening, stable to minimally decreased lymph node size, and continued bilateral sacral fractures. The patient underwent 6 weeks of external beam radiation to the rectal mass and pelvic lymph nodes with capecitabine as a radiation sensitizer. She reported that her hip pain was improving at this time.
Approximately 2 months after completion of external beam radiation, the patient underwent successful surgical resection of her rectal mass with a diverting loop ileostomy and lateral pelvic node dissection without complication. She recovered well but was experiencing pelvic pain during this time. A non-contrast MRI of the pelvis revealed a new insufficiency fracture of the right inferior sacroiliac joint along with the established healing of bilateral sacral alar fractures. An initial dual-energy X-ray absorptiometry (DXA) scan was significant for a Z-score of -2.5 of the lumbar spine, consistent with low bone mass, and a Z-score of -1.4 of the total proximal femur. The decision to initiate antiresorptive therapy was deferred at this time due to the patient’s pending ileostomy reversal surgery, which she tolerated well. She continued to be monitored clinically and radiographically without evidence of recurrent malignant disease.
Regarding her bone health, initial consideration was given to bisphosphonate therapy after delivery given her history of multiple sacral fractures. However, after chemotherapy, the patient’s menses did not resume, and her gynecologist established a diagnosis of premature menopause. Thus, hormone replacement therapy was initiated with daily estradiol/norethindrone tablets, and the patient continued on daily calcium and vitamin D supplementation to maintain her bone health. The follow-up DXA scan showed an increase in bone density at the spine and significant improvement at the hip 1 year after initiation of hormone replacement therapy. Bone turnover has decreased appropriately.
| Discussion | ▴Top |
Multiple sacral fractures in a young pregnant female with a history of rectal cancer raised concern for metastases to the bone. Per a 2019 Centers for Disease Control and Prevention (CDC) report, rectal cancer is the fourth most lethal cancer in the United States and generally develops over the course of several years [2]. It typically occurs in patients over age 50 but can also occur in young adults, such as the patient we present here. Apart from advanced age, other risk factors include inflammatory bowel disease, family history of colorectal cancer, physical inactivity, alcohol use and smoking, and a diet high in processed meat [3]. Though 60% of patients with colorectal cancer develop metastases within 5 years of diagnosis, metastases to the bone are rare with the peritoneum and liver being the most common sites [4, 5]. One population-based study found that the incidence of bony metastases in patients diagnosed with colorectal cancer was 6%, and patients with rectal cancer had a higher incidence of metastases to the bone compared to patients with right- or left-sided colon cancer [6]. Despite our patient’s multiple sacral fractures, there was no evidence of osseous lesions on imaging, making bony metastases a less likely diagnosis. It should be noted that the patient’s history of pelvic radiation therapy itself is a risk factor for pelvic fracture as radiation interferes with the osteoblast cell cycle, resulting in apoptosis [7]. Insufficiency fractures resulting from radiation can appear anywhere from months to several years after radiation but most often occur within 2 years of completion of treatment [7].
A more plausible explanation for this patient’s multiple sacral fractures was pregnancy-associated osteoporosis, which is also a relatively rare condition that typically occurs during the last trimester or early postpartum period. Pregnancy is associated with decreased bone mass as the growing fetus requires a significant source of maternal calcium for proper skeletal development [8]. Additionally, decreased bone mineral density has been associated with the postpartum state and breastfeeding as it is a hypoestrogenic state due to postpartum amenorrhea. Furthermore, maternal calcium is lost through breast milk. Decreased serum estrogen after delivery may also contribute to an increased risk of fragility fractures [8]. Risk factors for pregnancy-associated osteoporosis include low BMI, physical inactivity, decreased calcium intake, vitamin D deficiency, glucocorticoid use, and smoking. Since the condition is typically self-resolving, treatment is generally conservative and entails calcium and vitamin D supplementation as well as regular, weight-bearing physical activity [9]. There is limited evidence for medical therapy. However, if a patient fails conservative management, medications such as denosumab and teriparatide may be used [8]. Bisphosphonates may cross the placenta and can be detrimental to the fetus, restricting their use. In contrast, a literature review by Kovacs et al [10] found that bisphosphonates posed no harm to the fetus. In this case, our patient was treated conservatively with calcium and vitamin D along with the estradiol/norethindrone tablets prescribed by her gynecologist for premature menopause. Her bone health has since been monitored regularly with DXA scans and labs. Given her most recent DXA scan demonstrating stable or improved bone density without further fractures, the patient will continue with hormone replacement therapy.
A differential diagnosis to consider in this patient is transitory osteoporosis of the hip (TOH), a condition characterized by temporary bone loss of the femur along with bone marrow edema. This is an underestimated disease process that most commonly affects middle-aged males and females in the third trimester of pregnancy and breastfeeding period [8]. Most patients do not present with a clear inciting incident, but factors that can predispose a patient to TOH include prior trauma, gout, arthropathies, osteomyelitis, surgery, vascular damage, radiation, and neoplasms [11]. The pathogenesis of TOH is not clear, but it is thought that metabolic stress during pregnancy and breastfeeding contributes to increased bone turnover. Subsequent edema, caused by microvascular damage of the bone marrow, results in vasodilation and hyperemia, which raise intraosseous pressure that is perceived as pain by the patient [12].
Patients with TOH present with acute-onset hip pain or mild, progressively worsening pain that radiates to the groin and thigh, classically exacerbated by weight-bearing and physical activity [11]. The diagnosis of TOH is made with MRI, which can detect bone marrow edema as early as 48 h after symptom onset [10, 12]. Edema appears as a high-intensity signal on T2-weighted images located at the femoral head with possible extension into the femoral neck and intertrochanteric region [11]. Given the lack of marrow edema on MRI and a pain pattern not consistent with TOH, this diagnosis was less likely in our patient. With regards to prognosis, TOH typically self-resolves within a few months, and management is centered around analgesia [8]. Other differential diagnoses of TOH include septic arthritis, sacroiliac strain, sciatica, avascular necrosis of the femoral head, and less commonly, malignancy.
This case demonstrates a rare instance of pregnancy-associated osteoporosis and fractures in a young woman with stage IIIB rectal cancer, raising concern for skeletal metastatic disease. Although rare, pregnancy-associated osteoporosis and TOH should be considered in women who sustain fractures in the setting of cancers that have a predilection for bone.
Acknowledgments
The authors thank the patient for her willingness to participate in the making of this case report as well as the providers who worked to diagnose and treat this patient.
Financial Disclosure
The authors did not receive any funding for this project.
Conflict of Interest
None to declare.
Informed Consent
In accordance with the 2013 CARE Checklist, the patient has provided informed consent for the authors of this manuscript to submit and publish the case report and its findings in a medical journal. No patient identifiers have been used.
Author Contributions
AI and PT collectively composed the manuscript text and reviewed the case report in its entirety. PT and AI prepared Figure 1 and its description. Both authors have reviewed the manuscript.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
Abbreviations
MRI: magnetic resonance imaging; FOLFOX: folinic acid, fluorouracil, and oxaliplatin; IVF: in vitro fertilization; BMI: body mass index; NTx: N-telopeptide cross-links; DXA: dual-energy X-ray absorptiometry; CDC: Centers for Disease Control and Prevention; TOH: transitory osteoporosis of the hip
| References | ▴Top |
- Gulson B, Taylor A, Eisman J. Bone remodeling during pregnancy and post-partum assessed by metal lead levels and isotopic concentrations. Bone. 2016;89:40-51.
doi pubmed - U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. (2022, November). U.S. Cancer Statistics Data Visualizations Tool, based on 2021 submission data (1999-2019).
- Hossain MS, Karuniawati H, Jairoun AA, Urbi Z, Ooi J, John A, Lim YC, et al. Colorectal cancer: a review of carcinogenesis, global epidemiology, current challenges, risk factors, preventive and treatment strategies. Cancers (Basel). 2022;14(7):1732.
doi pubmed pmc - Pretzsch E, Bosch F, Neumann J, Ganschow P, Bazhin A, Guba M, Werner J, et al. Mechanisms of metastasis in colorectal cancer and metastatic organotropism: hematogenous versus peritoneal spread. J Oncol. 2019;2019:7407190.
doi pubmed pmc - Baek SJ, Hur H, Min BS, Baik SH, Lee KY, Kim NK. The characteristics of bone metastasis in patients with colorectal cancer: a long-term report from a single institution. World J Surg. 2016;40(4):982-986.
doi pubmed - Lei S, Ge Y, Tian S, Cai B, Gao X, Wang N, Wang G, et al. Colorectal cancer metastases to brain or bone and the relationship to primary tumor location: a population-based study. J Gastrointest Surg. 2020;24(8):1833-1842.
doi pubmed - Kang YM, Chao TF, Wang TH, Hu YW. Increased risk of pelvic fracture after radiotherapy in rectal cancer survivors: a propensity matched study. Cancer Med. 2019;8(8):3639-3647.
doi pubmed pmc - Galanis A, Dimopoulou S, Karampinas P, Vavourakis M, Papagrigorakis E, Sakellariou E, Karampitianis S, et al. The correlation between transient osteoporosis of the hip and pregnancy: A review. Medicine (Baltimore). 2023;102(41):e35475.
doi pubmed pmc - Chaniotakis C, Koutserimpas C, Raptis K, Zafeiris E, Alpantaki K, Effraimidis G. Pregnancy associated osteoporotic vertebral fractures: an underdiagnosed condition of back pain. J Musculoskelet Neuronal Interact. 2021;21(2):332-334.
pubmed pmc - Kovacs CS, Ralston SH. Presentation and management of osteoporosis presenting in association with pregnancy or lactation. Osteoporos Int. 2015;26(9):2223-2241.
doi pubmed - Khan MM, Imtiaz M, Cheema FE, Bacani N, Anwar S, Ismail U. Transient osteoporosis of the hip: a radiologist's perspective. Cureus. 2022;14(9):e29384.
doi pubmed pmc - Maisi N, Patoulias D, Tsagkaris C, Tsagatakis M, Goules D. Transient hip osteoporosis: etiopathogenetic, clinical, and imaging approach. Mediterr J Rheumatol. 2022;33(2):196-200.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
