| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Case Report
Volume 12, Number 3, December 2023, pages 102-105
Postpartum Spontaneous Adrenal Hematoma
Ana Claudia Lopesa, d , Andreia Miguelb, Eliana Teixeiraa, Tiago Alves Pachecoc, Maria de Lurdes Pinhoa, Ana Paula Lopesa
aGynecology and Obstetrics Department, Centro Hospitalar Barreiro-Montijo, Barreiro, Portugal
bCentro Hospitalar Lisboa Central-Maternidade Alfredo da Costa, Lisboa, Portugal
cUnidade de Saude Familiar Lavradio, Barreiro, Portugal
dCorresponding Author: Ana Claudia Lopes, Gynecology and Obstetrics Department, Centro Hospitalar Barreiro-Montijo, Barreiro, Portugal
Manuscript submitted October 5, 2023, accepted November 10, 2023, published online December 28, 2023
Short title: Postpartum Spontaneous Adrenal Hematoma
doi: https://doi.org/10.14740/jcgo917
| Abstract | ▴Top |
Adrenal hematoma refers to an acute hemorrhage originating from the adrenal gland. When it occurs spontaneously, without an associated traumatic event (the most common cause), it is categorized as spontaneous adrenal hematoma. Spontaneous adrenal hematoma is a very rare condition, particularly during the postpartum period. Although a few cases of adrenal hematoma during pregnancy have been documented in the literature, no cases have been reported during the puerperium. We present the case of a 43-year-old woman who experienced acute right-sided flank pain, fever, and fatigue 3 days after delivering a baby vaginally. Following an angiography-computed tomography (angio-CT) scan to rule out thromboembolism, the radiologist identified a unilateral hemorrhagic mass on the adrenal gland. The management of this adrenal hematoma involved a conservative approach, which included rest and close monitoring to prevent rupture and adrenal insufficiency. Clinical diagnosis of spontaneous adrenal hematoma presents a significant challenge due to its vague and nonspecific symptoms, especially during the puerperium, as these symptoms can overlap with other common postpartum complications. Diagnosis is often incidental and relies on imaging studies. In this particular case, a high degree of clinical suspicion and a thorough diagnostic workup were crucial in achieving the correct diagnosis. Through this case report, we aim to raise awareness and provide a review of the current literature on this exceedingly rare condition.
Keywords: Adrenal hematoma; Postpartum; Flank pain; Pregnancy; Spontaneous
| Introduction | ▴Top |
Adrenal hematoma is an extremely rare condition, with a prevalence of 0.14% to 1.8% based on autopsy studies [1, 2]. However, it is worth noting that extensive bilateral adrenal hemorrhage is observed in 15% of patients who have succumbed to shock [2]. Adrenal hematomas can have diverse etiologies and may manifest unilaterally or bilaterally.
The primary cause of adrenal hematomas is trauma, which predominantly results in unilateral hemorrhages [2]. These are often localized to the right side due to a higher risk of the gland becoming compressed between the liver and the spine, along with increased pressure on the right adrenal vein due to compression from the inferior vena cava. Traumatic adrenal hematomas are frequently associated with hematomas in the kidney, liver, and spleen and occur in isolation in less than 5% of abdominal traumas [1].
Another cause of unilateral adrenal hematomas is adjacent tumors, which can be either benign or malignant. In cases of spontaneous unilateral adrenal hematomas, it is imperative to rule out the presence of a concealed neoplasm. Consequently, post-diagnosis follow-up with computed tomography (CT) scans is recommended.
The most common benign tumor associated with adrenal hematoma is pheochromocytoma [1]. Myelolipomas, although exceedingly rare, can also cause adrenal bleeding. Among malignant tumors, metastases from bronchogenic, renal, breast carcinomas or melanomas are the most frequent, accounting for 20% of cases [1]. Adrenocortical carcinoma, a rare malignant tumor, can underlie adrenal hematoma, particularly when a tumor exceeds 6 cm in size [1].
Bilateral adrenal hematomas are less commonly attributed to trauma, except in cases of severe hemorrhagic shock, and are primarily linked to systemic conditions. Although the exact mechanism leading to adrenal hematoma remains incompletely understood, it is believed to involve the unique circulation of the suprarenal gland, with three arteries branching abruptly into a capillary network and only one vein [1]. The presence of elevated epinephrine levels, which increase platelet aggregation and vasoconstriction, may lead to elevated blood pressure within the gland’s circulation, resulting in hemorrhage [1]. This predisposition suggests that conditions such as coagulopathies, infections, stress, and pregnancy can cause adrenal hemorrhage.
Stress situations, such as pregnancy and the postpartum period, can also give rise to adrenal hematomas, with a prevalence ranging from 0.14% to 1.1% of pregnancies [3]. This condition is often characterized by fever in 42% of cases and abdominal pain in 43% of cases, with a higher incidence in the third trimester, posing a potential threat to both the mother and fetus [4, 5]. Major obstetric factors associated with adrenal hematoma include hypertensive disorders, pregnancy toxemia, spontaneous abortion, traumatic delivery, postpartum hemorrhage, and torsion of an adnexal tumor during pregnancy [2, 6].
In addition to its rarity, adrenal hematoma can present in various forms, from being asymptomatic to displaying nonspecific clinical symptoms such as diffuse abdominal pain, flank pain, fever, confusion, or hypotension [2]. The most consistent manifestation is a decrease in hemoglobin levels [1]. On the other hand, it can become a life-threatening event in the presence of massive bilateral hemorrhage or adrenal insufficiency. Due to its vague presentation, many diagnoses are made post-mortem or incidentally during imaging studies conducted while investigating other causes.
For diagnosis, ultrasound is often insufficient in most adult cases [1]. Contrast-enhanced CT scans are generally the preferred imaging modality, although magnetic resonance imaging (MRI) is more sensitive. MRI can be employed to rule out the presence of an underlying non-visible neoplastic mass not detectable by CT, or during pregnancy to avoid radiation exposure. Adrenal insufficiency should also be considered, although it is more common in cases of bilateral adrenal hematomas.
Treatment options include a conservative approach with observation and pain management, blood transfusions or invasive methods involving interventional radiology or surgery. The choice of approach depends on the severity of the condition regarding extent of hemorrhage, the patient’s condition, and the underlying cause.
| Case Report | ▴Top |
Our case involves a 43-year-old healthy postpartum woman with no significant prior medical history. She gave birth 11 days ago through a vaginal delivery with episiotomy and is currently breastfeeding. Her obstetric history includes a previous cesarean section and a vaginal delivery 9 and 6 years ago, respectively, with no pregnancy or postpartum complications associated. During this pregnancy, she was under the care of a private obstetrician and was diagnosed with pregnancy-induced hypertension at 34 weeks, which was not medicated. She spontaneously went into labor at 38 weeks, had a normal vaginal delivery without complications, and was discharged on the second day postpartum with normal postpartum parameters.
On the third day postpartum, she began experiencing persistent right-sided flank pain that worsened with respiratory movements, along with fever, with a peak temperature of 38.3 °C, and fatigue. She did not report any urinary or respiratory complaints and had no history of trauma. She was evaluated by her family physician and underwent a chest X-ray, abdominal ultrasound, and renal ultrasound, all of which were normal. The urine culture was also negative. Laboratory tests revealed a hemoglobin level of 11 g/dL, normal platelets, normal coagulation parameters, negative infectious markers, normal kidney and liver function and D-dimer levels of 3,599 ng/mL.
Due to the persistence of her symptoms, she was referred to our emergency department on the 11th day postpartum. Upon examination, she had a blood pressure of 148/94 mm Hg, a heart rate of 101 beats per minute (bpm), was afebrile, had an oxygen saturation of 99%, and showed no signs of respiratory distress. The gynecological examination and pelvic ultrasound were consistent with the postpartum phase, and a renal Murphy’s sign was negative. To rule out pulmonary embolism, a chest angiography-computed tomography (angio-CT) was performed, revealing a spontaneously hyperdense mass in the upper abdominal segments, in the right adrenal gland, measuring 45 × 32 × 37 mm, suggesting a possible hemorrhagic nature related to adrenal gland bleeding. Subsequently, an abdominal CT confirmed the diagnosis of unilateral adrenal hematoma (Fig. 1).
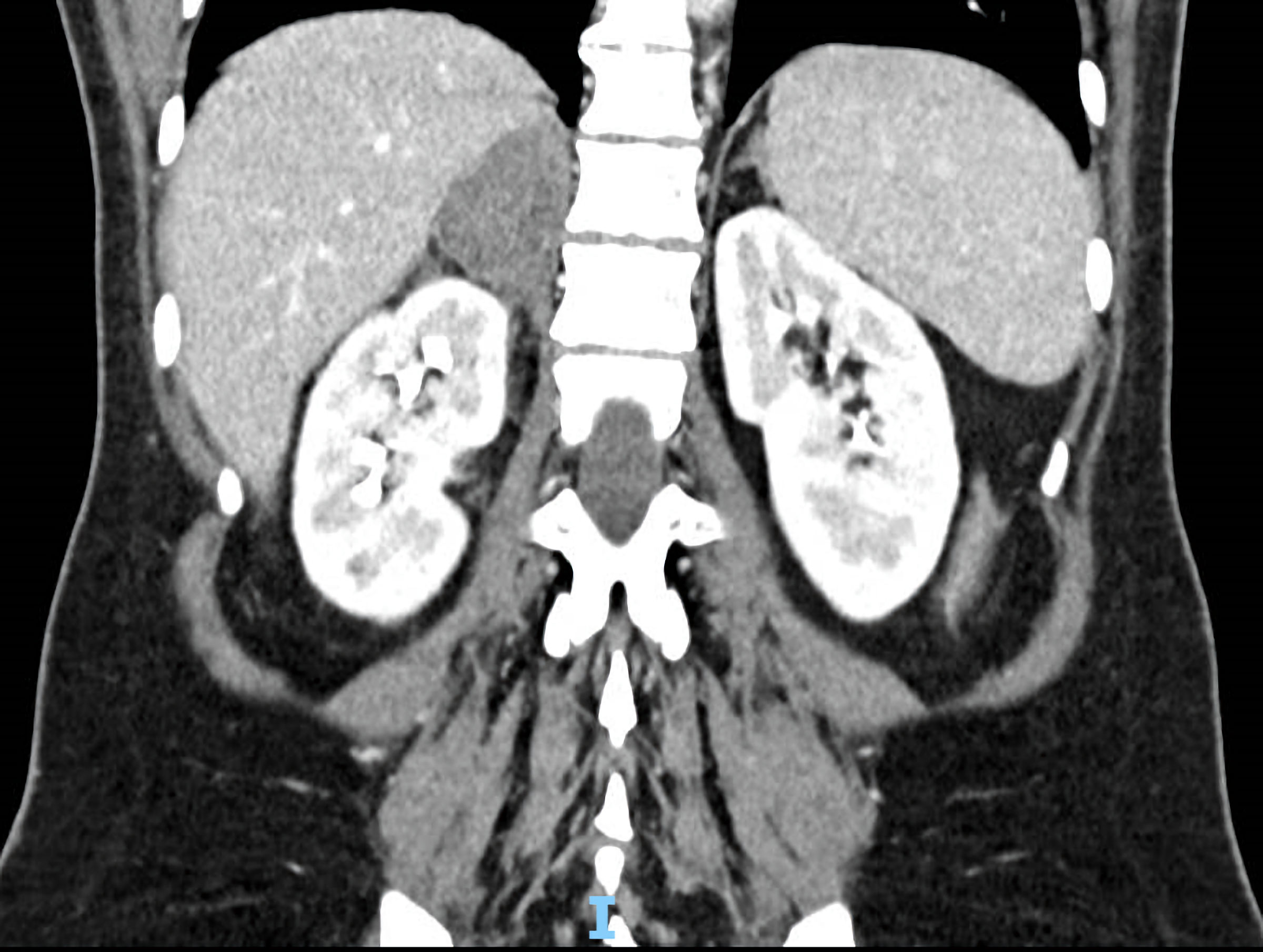 Click for large image | Figure 1. CT scan image of right adrenal hematoma at diagnosis. CT: computed tomography. |
The postpartum patient was then admitted for strict bed rest, pain management and close clinical and laboratory monitoring to prevent hematoma exacerbation, rupture, and the need for emergency surgical intervention. During her hospital stay, repeat laboratory tests and a follow-up CT scan performed 48 h after admission showed no significant changes. Adrenal insufficiency screening (early morning serum cortisol levels) also returned with normal results.
At the time of discharge the patient had clinically improved and the hematoma had slightly reduced in size. One month after discharge she underwent another CT scan which demonstrated a marked reduction in the hematoma’s dimensions (Fig. 2). At the 6-month follow-up a normal CT scan showed no signs of adjacent adrenal gland tumors.
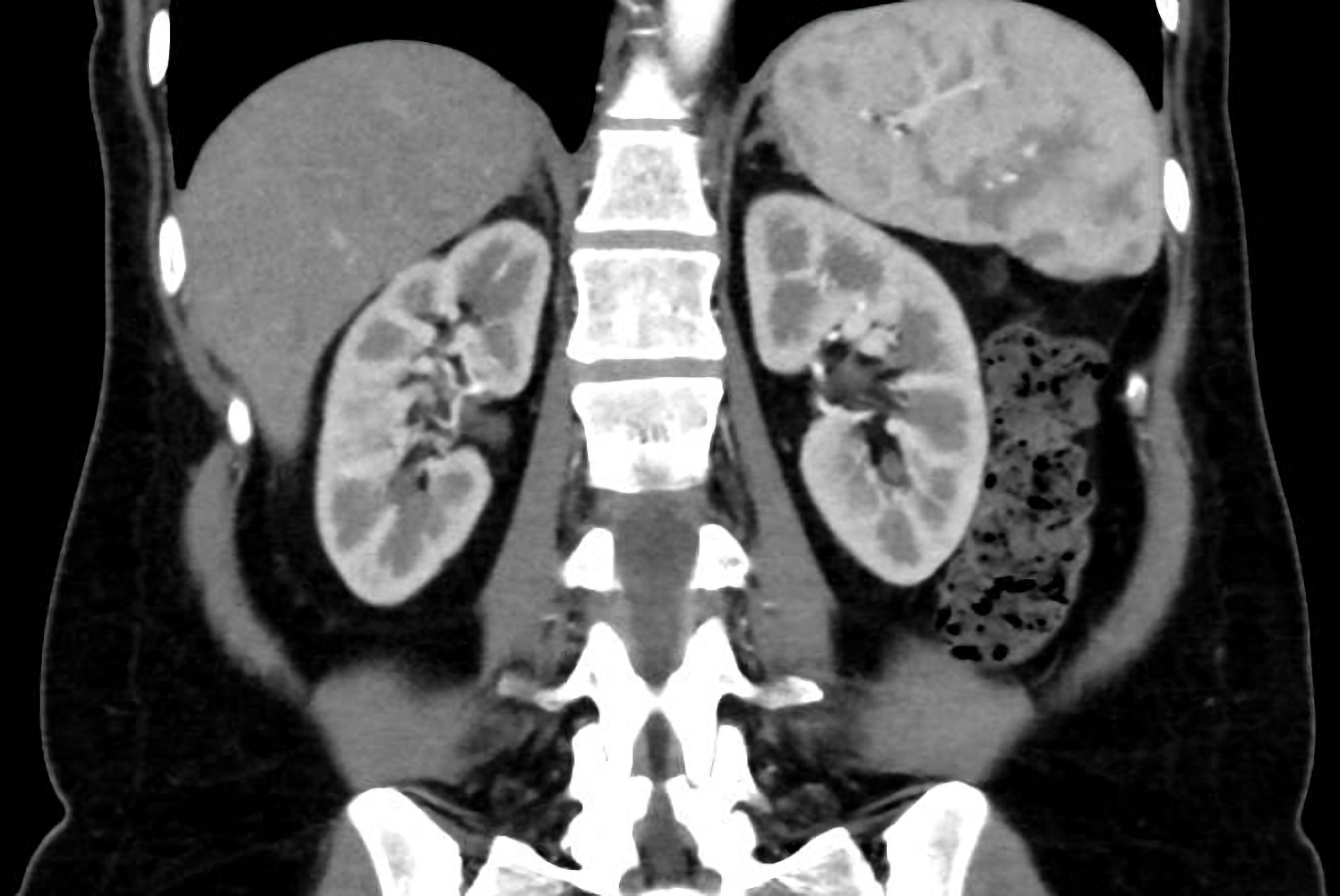 Click for large image | Figure 2. One-month follow-up CT scan image of right adrenal hematoma. CT: computed tomography. |
| Discussion | ▴Top |
Adrenal hematoma is an infrequent occurrence during pregnancy, with a prevalence of approximately 1%, and its documentation in the medical literature remains limited. The clinical presentations of adrenal hematomas are highly diverse, ranging from substantial retroperitoneal hematomas to incidental radiological findings. Their occurrence during the postpartum period is even more exceptional, with no defined prevalence estimates available.
While adrenal hematoma typically manifests with nonspecific symptoms that can be easily overlooked in the context of pregnancy, it should be considered in the diagnostic process due to its potential life-threatening consequences for both the mother and the fetus.
This condition is believed to arise from a complex interplay of physiological adaptations during pregnancy, including adrenal cortex hyperplasia, leading to increased blood flow to the gland and venous stasis. This hyperplasia, combined with the hypercoagulable state of pregnancy and the postpartum period, may serve as a trigger for adrenal bleeding, either independently or in conjunction with other risk factors [7]. This heightened susceptibility extends into the postpartum period, with adrenal hematomas being particularly prevalent following traumatic deliveries. In our presented clinical case, no traumatic birth was reported, and symptoms only emerged on the third postpartum day, without any identifiable precipitating trauma, supporting the diagnosis of spontaneous adrenal hematoma. Additionally, our patient had a known risk factor, pregnancy-induced hypertension, which was also present in the postpartum period, as indicated during the admission physical examination, potentially acting as a triggering factor for hemorrhage.
The diagnostic challenge of adrenal hematoma, especially during the postpartum phase, arises from symptom overlap with more common puerperal complications, such as preeclampsia, postpartum infections, uterine atony, and retained placental tissue. These conditions often present with similar clinical features, including fever, abdominal pain, and fatigue, leading to misdiagnosis or delayed recognition of adrenal hematomas.
The clinical presentation prompted consideration of various diagnostic hypotheses, including more prevalent postpartum complications like urinary tract infections, renal colic, adnexal torsion, and pulmonary embolism. The pursuit of diagnostic investigations for these possibilities unexpectedly led to the discovery of adrenal hematoma through imaging studies, a pattern observed in a significant proportion of reported cases. Notably, renal, abdominal, and pelvic ultrasounds failed to detect the hematoma in this case, highlighting the value of thoracic CT angiography, which initially raised suspicion, and was subsequently confirmed on abdominal CT scans.
Imaging studies, particularly contrast-enhanced CT scans and MRI, play a pivotal role in confirming the diagnosis of adrenal hematomas. However, even these advanced imaging modalities may not always yield a straightforward diagnosis, as the hematoma’s appearance can mimic other adrenal lesions or neoplasms [6]. Furthermore, in pregnant or breastfeeding individuals, minimizing radiation exposure is crucial, making MRI the preferred imaging modality in such cases.
Although a decline in hemoglobin levels is a consistent finding, it lacks specificity and becomes even more challenging to interpret in the postpartum period. As such, relying solely on laboratory parameters can yield inconclusive results and complicate the diagnostic process. Even if hemoglobin levels were measured prior to delivery, the expected normal blood loss during childbirth would not typically prompt further investigation. Nevertheless, a progressive decline in successive hemoglobin evaluations, coupled with additional symptoms, as observed in our patient, should raise suspicion. Elevated D-dimer levels, while potentially normal in the postpartum period, were crucial in our case, prompting thoracic CT angiography to rule out pulmonary embolism in light of fatigue.
This case underscores the complexity of diagnosing adrenal hematomas, particularly in the postpartum period. Factors such as the normal postpartum context, which may lead to symptom dismissal, and the numerous potential complications make the diagnosis challenging, especially when these complications are more prevalent. These nonspecific symptoms often overlap with those of more common postpartum complications, further complicating the clinical diagnosis. The subtle nature of these presentations necessitates a high index of suspicion among healthcare providers. However, adrenal hematoma should be included in the differential diagnosis for flank pain in postpartum, especially when risk factors are present, and after ruling out more common causes.
In cases of controlled bleeding and hemodynamically stable patients, as in our case, an expectant management approach is preferred [7]. During pregnancy, conservative therapy is the primary strategy, with preterm delivery indicated only in specific circumstances, such as when adrenal hematoma occurs in the context of eclampsia or preeclampsia or when maternal or fetal clinical status deteriorates [1, 4]. Vaginal delivery is not contraindicated provided the patient remains stable [1, 4]. Surveillance involves strict bed rest, serial hemoglobin and hematocrit assessments, and frequent imaging (MRI or CT) to document hematoma resolution or progression. Fetal monitoring is crucial during pregnancy [1, 4]. The optimal timing for imaging studies is not well defined in the literature. Symptomatic pain management is indicated, as well as transfusion of blood products in the case of a significant drop in hemoglobin. Rest and supportive care are essential to prevent worsening bleeding, shock or rupture requiring emergency surgery. In cases of refractory hemodynamic instability, suspected bleeding from neoplasms, or extensive retroperitoneal hematomas, arterial embolization by interventional radiology may be considered if available at the institution [1]. This approach is particularly favored in cases of bleeding from pheochromocytoma [1]. When conservative treatment fails, exploratory laparotomy is warranted. Surgical intervention should be the primary treatment for cases involving large, and suspicious neoplasms [1].
Adrenal insufficiency secondary to hematoma is unlikely if bleeding is controlled and unilateral, but screening is essential for bilateral hematomas [1]. In this case, the evaluation performed was unremarkable, as expected. Long-term follow-up in this patient was vital to rule out potential neoplasms concealed by the initial hematoma.
In summary, adrenal hematomas during pregnancy and the postpartum period introduce unique clinical challenges that complicate their recognition and diagnosis. These distinctive features contribute to the diagnostic difficulties associated with this condition and underscore the necessity of a comprehensive diagnostic workup.
The interplay between hormonal changes, increased blood volume, and the mechanical factors of pregnancy and postpartum contributes to the distinct clinical presentation of adrenal hematomas during this period. Healthcare providers must maintain a high degree of clinical suspicion and utilize advanced imaging modalities to confirm the diagnosis while considering the potential limitations and complexities associated with each case. Raising awareness of this rare condition, particularly in the context of pregnancy and the postpartum period, is essential to ensure prompt recognition and appropriate management. Further research and case reports are warranted to enhance our understanding of adrenal hematomas in these specific clinical settings and to develop more effective strategies for diagnosis and management.
Learning points
The diagnostic challenges in distinguishing adrenal hematoma from other puerperal complications underscore the importance of a multidisciplinary approach involving obstetricians, radiologists, and internists. Clinical suspicion and a comprehensive diagnostic workup are pivotal in achieving an accurate and timely diagnosis, which is crucial for optimizing patient outcomes.
Acknowledgments
The authors would like to thank the patient for giving her informed consent for publication of this case report.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from the patient for publication of this case report.
Author Contributions
Conceptualization: Ana Claudia Lopes, Andreia Miguel, Eliana Teixeira, and Tiago Alves Pacheco. Investigation: Ana Cluudia Lopes, Andreia Miguel, Eliana Teixeira, and Tiago Alves Pacheco. Formal analysis: Maria de Lurdes Pinho. Supervision: Maria de Lurdes Pinho, and Ana Paula Lopes. Writing - original draft: Ana Claudia Lopes. Writing - review and editing: Andreia Miguel, Eliana Teixeira, Tiago Alves Pacheco, and Maria de Lurdes Pinho.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
CT: computed tomography; MRI: magnetic resonance imaging
| References | ▴Top |
- Badawy M, Gaballah AH, Ganeshan D, Abdelalziz A, Remer EM, Alsabbagh M, Westphalen A, et al. Adrenal hemorrhage and hemorrhagic masses; diagnostic workup and imaging findings. Br J Radiol. 2021;94(1127):20210753.
doi pubmed pmc - Wani MS, Naikoo ZA, Malik MA, Bhat AH, Wani MA, Qadri SA. Spontaneous adrenal hemorrhage during pregnancy: review of literature and case report of successful conservative management. J Turk Ger Gynecol Assoc. 2011;12(4):263-265.
doi pubmed pmc - Imga NN, Tutuncu Y, Tuna MM, Dogan BA, Berker D, Guler S. Idiopathic spontaneous adrenal hemorrhage in the third trimester of pregnancy. Case Rep Med. 2013;2013:912494.
doi pubmed pmc - Gupta A, Minhas R, Quant HS. Spontaneous adrenal hemorrhage in pregnancy: a case series. Case Rep Obstet Gynecol. 2017;2017:3167273.
doi pubmed pmc - Singh M, Sinha A, Singh T. Idiopathic unilateral adrenal hemorrhage in a term pregnant primigravida female. Radiol Case Rep. 2020;15(9):1541-1544.
doi pubmed pmc - El-Gharib MN, Hakami OA, Al-Otaibi MF, et al. Adrenal gland hematoma during pregnancy and postpartum: a systematic review. Oman Med J. 2020;35(5):e140.
- Yang L, Zhu YC, Liu RB. Spontaneous adrenal hematoma in pregnancy: A case report. Medicine (Baltimore). 2018;97(47):e13329.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
