| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 2, Number 1, June 2013, pages 42-44
Cesarean Scar Ectopic Pregnancy
Natasha Guptaa, c, Haas Barbaraa, Ekechukwu Kennethb, Blankstein Josefa
aDepartment of Obstetrics and Gynecology, Mount Sinai Hospital, 1500 S California Ave, Chicago, Illinois, 60608, USA
bDepartment of Radiology, Mount Sinai Hospital, 1500 S California Ave, Chicago, Illinois, 60608, USA
cCorresponding author: Natasha Gupta, 1618 S Washtenaw Ave, Unit 1, Chicago, Illinois, 60608, USA
Manuscript accepted for publication March 14, 2013
Short title: Cesarean Scar Ectopic Pregnancy
doi: https://doi.org/10.4021/jcgo98w
| Abstract | ▴Top |
This case illustrates the importance of considering a diagnosis of ectopic pregnancy at previous cesarean scar in a patient with pregnancy of unknown location. Pregnancy of unknown location is a term used by sonographers when a live intrauterine pregnancy consisting of gestational sac, fetal pole and or yolk sac cannot be visualized, in presence of sufficiently elevated quantitative serum chorionic gonadotropin (β-HCG). Modern obstetrician needs to be aware of the diagnosis of cesarean scar ectopic pregnancy and consider evaluation of scar with ultrasound or magnetic resonance imaging (MRI). We present here such a patient with pregnancy of unknown location, in whom cesarean scar pregnancy was accurately diagnosed and appropriately treated.
Keywords: Ectopic pregnancy; Previous cesarean
| Introduction | ▴Top |
Cesarean scar is a rare site for implantation of a pregnancy. Ectopic pregnancy overall is the leading cause of death in first trimester [1]. The incidence of pregnancy implantation at unusual sites like cesarean scar, cervix or ovaries is on rise due to increase in incidence of various risk factors like cesarean sections [2], dilatation and curettages and pelvic inflammatory diseases respectively. Diagnosis of these rare types of ectopic pregnancies is difficult and cesarean scar ectopic pregnancy as well as cervical pregnancy can be easily confused with each other or with an incomplete abortion enroute to expulsion. Most of the cases of cesarean scar present with vaginal bleeding, abdominal pain, serum β-HCG level elevated above the cut-off value and empty uterine cavity with a mass near the lower uterine segment or cervix. This patient was also diagnosed as incomplete abortion on initial scan in the emergency room and was treated as such. We describe here the steps taken to correctly diagnose and treat this patient.
| Case Report | ▴Top |
A 32-year-old female, gravida 3 para 2, presented to emergency room with vaginal spotting, occasional passage of clots and mild abdominal pain for last 5 days. Her quantitative serum chorionic gonadotrophin was 38,548 mIU/mL. She had history of two previous cesarean sections and had no other significant medical or social history. She was noted to have 2 cm dilated cervix on pelvic examination, with small amount of dark blood in vaginal vault and no active vaginal bleeding. All other examination was unremarkable. An emergency ultrasound showed no intrauterine pregnancy or adnexal masses, except a small hypoechoic mass noted in the lower uterine segment. This was considered to be the products of conception enroute to expulsion and patient was diagnosed with incomplete abortion. However, a detailed transvaginal scan was performed the next day which noted this lower uterine segment mass to be embedded in the previous cesarean scar. It appeared to be a heterogenous mass measuring 4.4 × 4.1 × 1.5 cm within the lower uterine segment, with increased vascularity in the periphery and within the previous cesarean scar (Fig. 1, 2). We performed a magnetic resonance imaging (MRI) which was consistent with the diagnosis of cesarean scar pregnancy. We successfully treated her with transvaginal ultrasound guided intragestational Methotrexate injection and uterine artery embolization (UAE) [3]. Her symptoms subsided and β-HCG was noted to be trending down adequately. She was discharged home and her follow up MRI revealed no residual mass at the scar and a β-HCG level less than 5 mIU/mL within 40 days of her treatment.
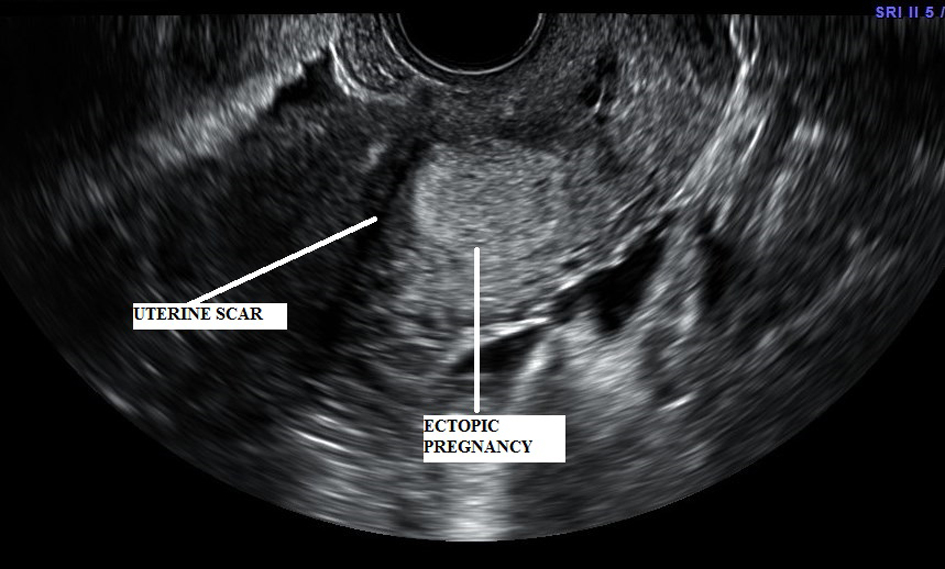 Click for large image | Figure 1. Transvaginal Scan showing uterine scar with gestational sac implanted at the scar. |
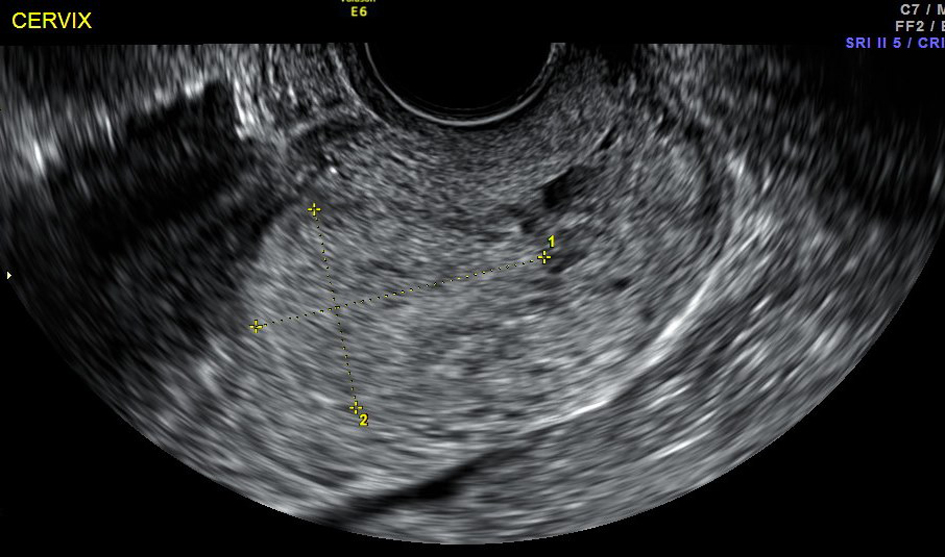 Click for large image | Figure 2. Ultrasound shows cesarean scar in the lower uterine segment and a gestational sac just above the cervix. |
| Discussion | ▴Top |
Cesarean scar ectopic pregnancy is a rare but lethal variant of ectopic pregnancy, where gestational sac implants at the previous uterine scar [4]. Cesarean scar ectopic pregnancy is often misdiagnosed as incomplete abortion, in process of expulsion and patients mistakenly undergo curettage leading to life threatening hemorrhage. Diagnosis of cesarean scar pregnancy requires a high degree of suspicion, especially when no intrauterine gestational sac can be identified and a pregnancy of unknown location is suspected. Differential diagnosis of cesarean scar ectopic pregnancy includes cervical pregnancy, early placenta accreta and incomplete abortion. Timor et al concluded in their review that cesarean scar ectopic pregnancy and early pregnancy placenta accreta are the consequences of increasing rate of cesarean deliveries [2]. They explored the similarities in symptomatology, diagnosis and treatment of these two conditions. Cesarean scar pregnancy can be diagnosed with transvaginal ultrasound which can identify a gestational sac or mass located in the lower uterine segment, within the cesarean scar. MRI can accurately detect the exact location of pregnancy, thus confirming the diagnosis [1, 4]. There is no unique treatment modality available to effectively terminate this pregnancy. However, a combination of different techniques including UAE and intragestational Methotrexate [3, 5]; intramuscular and intragestational Methotrexate [6]; hysteroscopic or laparoscopic resection after uterine artery embolization or curettage after intragestational methotrexate or UAE have all been attempted with varied success rates by different authors. Shao et al reported shorter curettage duration after local methotrexate injection and shorter hysterectomy duration with lowest operative blood loss as well as shorter length of hospital stay after UAE [7]. They also noted shortest time in β-HCG level returning to normal in patients that underwent laparoscopic or hysteroscopic resection after a local methotrexate injection or UAE [7]. Curettage alone may lead to excessive blood loss, thus necessitating hysterectomy [8]. Therefore, a combination of different modalities is preferred by most authors. Shen et al found bilateral uterine artery chemoembolization and local methotrexate injection to be a safe and effective treatment for cesarean scar pregnancy, with minimal morbidity [3]. In their study, the mean time until normalization of serum β-HCG was 37.7 days, and the mean time until cesarean scar mass disappearance was 33.3 days [3]. We employed the same approach for treatment of our patient and found similar time in normalization of β-HCG level and disappearance of cesarean scar mass. Wang et al described a newer transvaginal approach in removal of ectopic tissue from the cesarean scar via transvaginal hysterotomy [9, 10]. They reported no significant complications, a faster time to return to normal menstrual cycles and a rapid decline of β-HCG to normal than reported with the current techniques [10]. They also combined methotrexate injection with transvaginal hysterotomy for improved results [9]. This technique needs to be further evaluated for its safety and efficacy.
Early diagnosis and early treatment of cesarean scar ectopic pregnancy is essential to prevent maternal morbidity and mortality. Early diagnosis is possible by early clinical suspicion on behalf of the physician in a patient with pregnancy of unknown location and an early recognition of sonographic findings [4]. Several medical and surgical modalities are available for the treatment of cesarean scar pregnancy, but most authors have reported the combination of 2 - 3 different techniques more useful than any method used alone. Especially, curettage alone without a prior uterine artery embolization or local methotrexate injection may lead to life threatening bleeding [8]. Also, a close follow up with serial quantitative β-HCG levels is needed until level falls to < 5 mIUs/mL. Modern obstetricians need to be aware of the increasing incidence of this condition due to increase in cesarean section rates [4] and evaluate patients at risk with ultrasound, before undertaking curettage which can lead to hemorrhage and loss of fertility.
Acknowledgments
None.
Conflicts of Interest
None.
Grant Support
None.
Financial Disclosures
None.
| References | ▴Top |
- Koroglu M, Kayhan A, Soylu FN, Erol B, Schmid-Tannwald C, Gurses C, Karademir I, et al. MR imaging of ectopic pregnancy with an emphasis on unusual implantation sites. Jpn J Radiol. 2013;31(2):75-80.
doi pubmed - Timor-Tritsch IE, Monteagudo A. Unforeseen consequences of the increasing rate of cesarean deliveries: early placenta accreta and cesarean scar pregnancy. A review. Am J Obstet Gynecol. 2012;207(1):14-29.
doi pubmed - Shen L, Tan A, Zhu H, Guo C, Liu D, Huang W. Bilateral uterine artery chemoembolization with methotrexate for cesarean scar pregnancy. Am J Obstet Gynecol. 2012;207(5):386 e381-386.
- Osborn DA, Williams TR, Craig BM. Cesarean scar pregnancy: sonographic and magnetic resonance imaging findings, complications, and treatment. J Ultrasound Med. 2012;31(9):1449-1456.
pubmed - Frishman GN, Melzer KE, Bhagavath B. Ectopic pregnancy in a cesarean-section scar: the patient >6 weeks into an ectopic pregnancy, underwent local treatment. Am J Obstet Gynecol. 2012;207(3):238 e231-232.
- Timor-Tritsch IE, Monteagudo A, Santos R, Tsymbal T, Pineda G, Arslan AA. The diagnosis, treatment, and follow-up of cesarean scar pregnancy. Am J Obstet Gynecol. 2012;207(1):44 e41-13.
- Shao HJ, Ma JT, Xu LP, Yang CL, Fu YQ, Su XF. [Comprehensive analysis of therapeutic methods and effect on cesarean scar pregnancy]. Zhonghua Yi Xue Za Zhi. 2012;92(31):2191-2194.
pubmed - Zhang Y, Gu Y, Wang JM, Li Y. Analysis of cases with cesarean scar pregnancy. J Obstet Gynaecol Res. 2013;39(1):195-202.
doi pubmed - Wang Z, Le A, Shan L, Xiao T, Zhuo R, Xiong H, Shen Y. Assessment of transvaginal hysterotomy combined with medication for cesarean scar ectopic pregnancy. J Minim Invasive Gynecol. 2012;19(5):639-642.
doi pubmed - Le A, Shan L, Xiao T, Zhuo R, Xiong H, Wang Z. Transvaginal surgical treatment of cesarean scar ectopic pregnancy. Arch Gynecol Obstet. 2013;287(4):791-796.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
