| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 3, Number 3, September 2014, pages 105-107
The Feasibility of In-Clinic Ultrasound-Guided Removal of Contraceptive Implants: A Case Series
Pooja R. Patela, Sandra R. Herreraa, Toy G. Leea, Flor M. Galdameza, Kathleen L. Vincenta, b
aDepartment of Obstetrics and Gynecology, The University of Texas Medical Branch in Galveston, TX, USA
bCorresponding Author: Kathleen L. Vincent, Department of Obstetrics and Gynecology, The University of Texas Medical Branch, 301 University Boulevard, Galveston, TX 77555-0587, USA
Manuscript accepted for publication May 21, 2014
Short title: Ultrasound-Guided Removal of Contraceptive Implants
doi: https://doi.org/10.14740/jcgo256w
| Abstract | ▴Top |
The removal of a non-palpable subdermal contraceptive implant can be difficult and dangerous. We report on three cases in which the gynecologist herself performs real-time ultrasonography in the clinic, instead of referring the patient to a radiologist, to locate and remove non-palpable implants. This approach allows the clinician to offer a potentially safer and more convenient alternative to patients.
Keywords: Feasibility; Ultrasound; Removal; Contraceptive implants
| Introduction | ▴Top |
The single-rod subdermal contraceptive implant provides effective, long-term contraception and is easy to place. Although removal is usually effortless, there are occasions where removal of a non-palpable implant can be difficult and potentially dangerous for the patient. In such cases, the patient is frequently given a separate appointment with a radiologist who uses ultrasonography to locate the implant and mark the borders [1]. The patient then returns to the gynecologist who attempts removal again [2]. The logistics between an ultrasound in radiology and removal in the gynecology clinic can pose a challenge for patient care. In this case series, we propose the use of real-time ultrasonography by a gynecologist familiar with ultrasonography, to locate and remove these implants in a single clinic visit.
| Case Reports | ▴Top |
Case 1
A 26-year-old female with a BMI of 37 kg/m2 was referred to our clinic for removal of a non-palpable implant. She was seen by a gynecologist familiar with ultrasonography who successfully removed the implant using real-time ultrasonography (see Table 1 for procedure details).
 Click to view | Table 1. Detailed Description of Procedure |
Case 2
A 30-year-old female with a BMI of 29 kg/m2 presented to the gynecologist from the previous case for implant removal. The clinician used real-time ultrasonography to locate the implant, which was noted to be only 3.8 mm below the skin surface, and remove it successfully.
Case 3
A 20-year-old female with a BMI of 31 kg/m2 presented to the gynecologist from the previous cases for implant removal. The clinician again used real-time ultrasonography to locate the implant only 4.9 mm below the skin surface and successfully remove it.
| Discussion | ▴Top |
Non-palpable subdermal implants can result from suboptimal placement, the development of a dense fibrous sheath, or an increase in subcutaneous fat since the time of placement [3]. We present cases in which the gynecologist uses ultrasound guidance to both locate and remove non-palpable subdermal contraceptive devices. Gynecologists are typically trained in ultrasonography and routinely remove contraceptive implants; therefore, the simple combination of these two skills and familiarization with this process may help in achieving the removal of a non-palpable contraceptive implant in a single clinic visit. Through the experience of these cases, we noted that we were more comfortable and confident with our removal attempts when we were able to intermittently visualize the device via ultrasonography.
Table 1 gives a step-by-step account of our approach towards using real-time ultrasonography for localization and guidance in the removal of a non-palpable subdermal contraceptive implant. The literature supports the utilization of high-resolution linear probes (10 MHz) when using ultrasonography to localize subdermal contraceptive implants [2, 4, 5]. As these types of probes are not typically found in their clinic, gynecologists usually have the option between a vaginal or abdominal probe in their clinic. We used the vaginal (8 - 5 MHz) instead of the abdominal (5 - 2 MHz) probe as the higher frequency vaginal probe allows for better resolution of the shallow tissue. We found that transverse views were ideal for initial identification of the implant and delineation of the edges due to enhanced acoustic shadowing (Fig. 1, 2). In the longitudinal view, it was more challenging to initially identify the implant due to the thin width and similarity of the signal to surrounding tissue planes. However, once the implant location is identified, both transverse and longitudinal views allow for direct visualization of instrument depth and proximity to the implant during removal (Fig. 3).
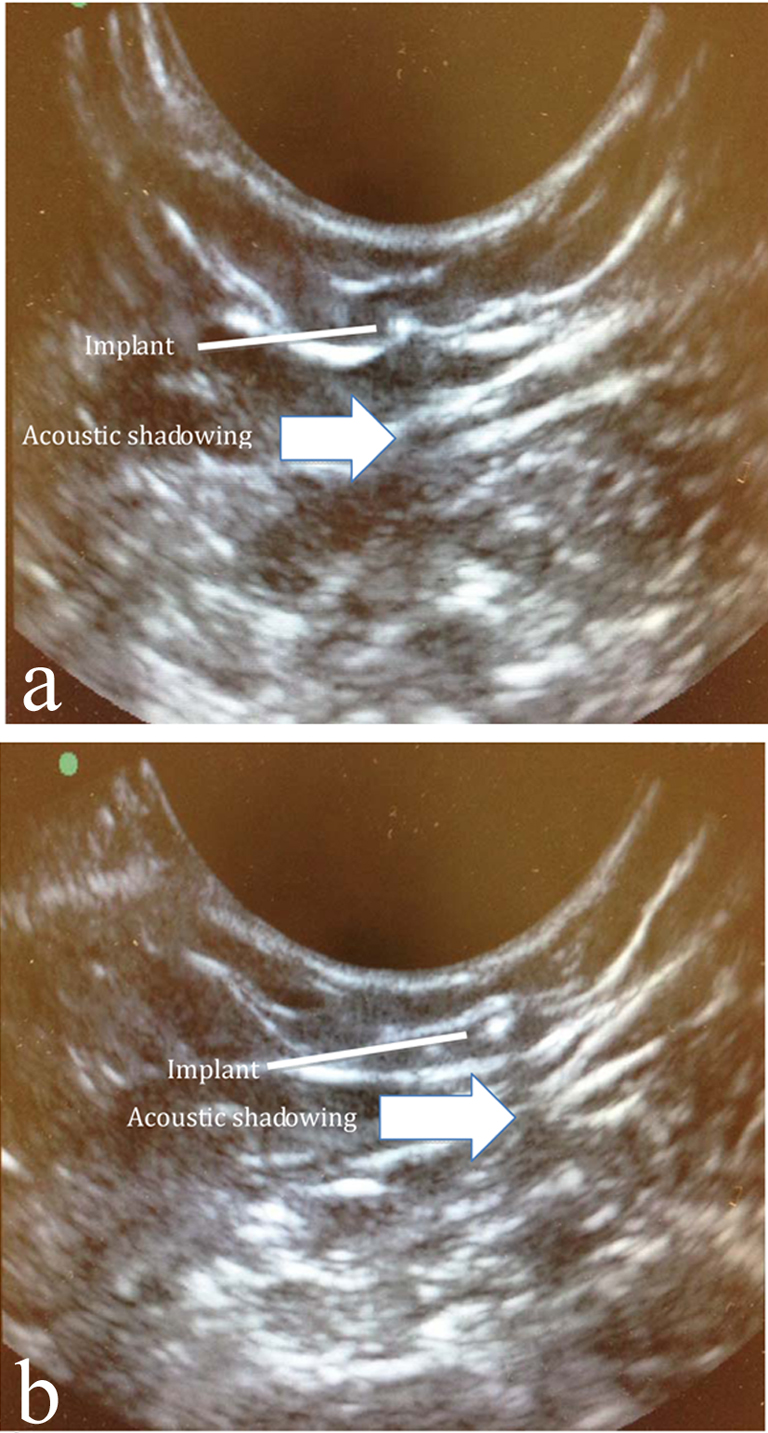 Click for large image | Figure 1. Acoustic shadowing of implant. In order to better see the acoustic shadowing behind the implant, two separate images of the implant are depicted. Note the movement of the acoustic shadowing as the image of the implant moves. |
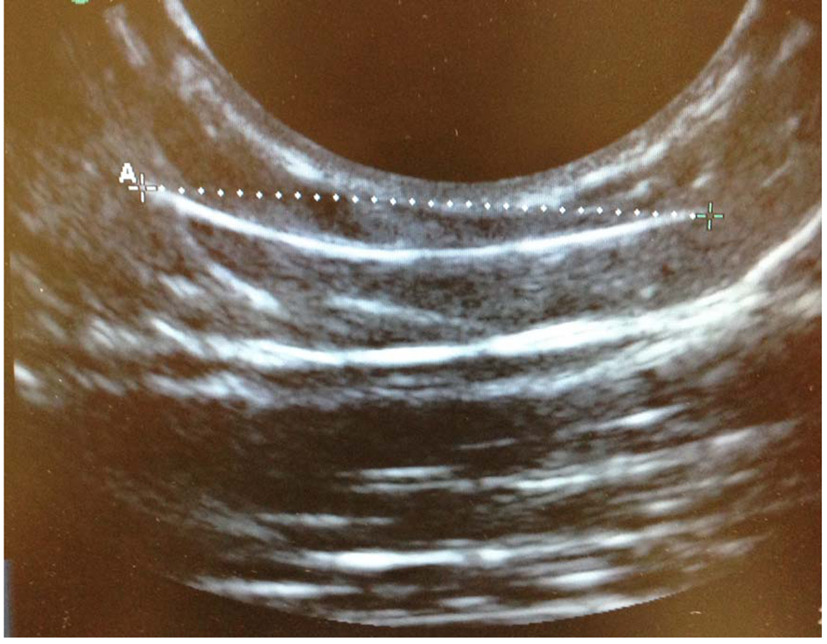 Click for large image | Figure 2. Longitudinal view of implant. The depth of the implant in this view matches that of Figure 1. Of note, care must be taken when using a longitudinal view of the implant as it can look similar to tissue planes and the acoustic shadowing is less prominent. |
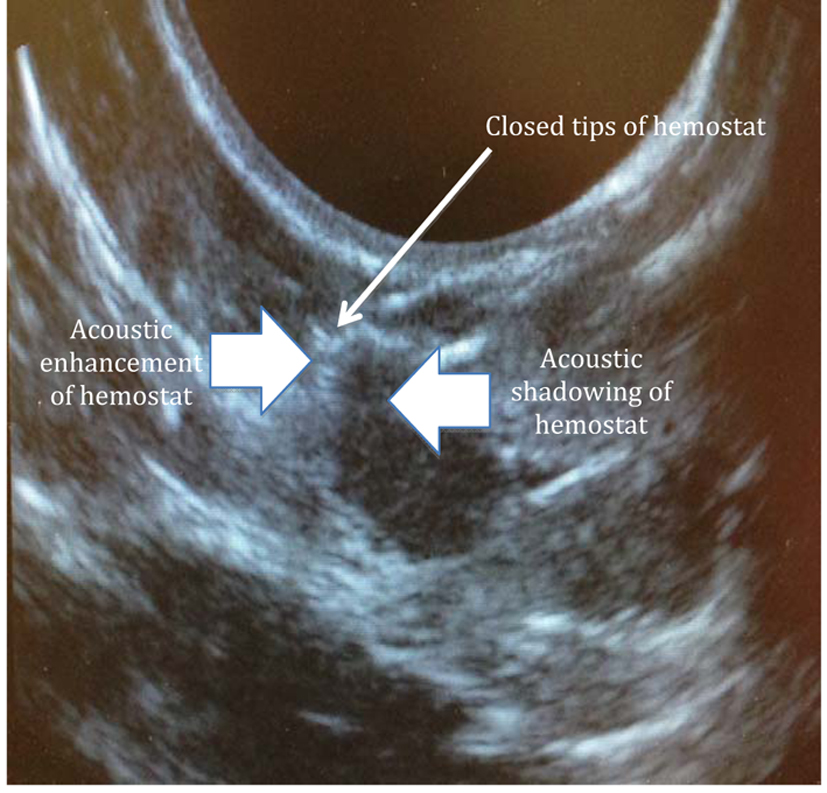 Click for large image | Figure 3. Acoustic shadowing of hemostat. Note the column of acoustic enhancement below hemostat and surrounding acoustic shadowing. This column and adjacent shadowing moves as the hemostat moves. |
We were surprised to find that the implants in these cases were difficult to palpate despite being so close to the skin surface. Had we not used real-time ultrasonography, we might have explored the tissue deeper than necessary.
To the best of our knowledge, this is the first report on the use of real-time ultrasonography to locate and remove the single-rod subdermal contraceptive implants in a single gynecologic clinic visit. Most of the reports on implant removals are by radiologists [2, 3, 6]. Removal by the gynecologist, on the other hand, may result in increased patient comfort as she is in the presence of her familiar gynecologist. In addition, a two-step process that involves movement of the patient from the time of image-guided localization of the device to the removal procedures is susceptible to inaccuracies.
In conclusion, ultrasound-guided removal of a non-palpable subdermal contraceptive implant by a gynecologist is a feasible in-clinic procedure. This approach may offer the gynecologist more comfort and confidence in attempting removal of non-palpable subdermal contraceptive implants.
| References | ▴Top |
- Shulman LP, Gabriel H. Management and localization strategies for the nonpalpable Implanon rod. Contraception. 2006;73(4):325-330.
doi pubmed - Singh M, Mansour D, Richardson D. Location and removal of non-palpable Implanon implants with the aid of ultrasound guidance. J Fam Plann Reprod Health Care. 2006;32(3):153-156.
doi pubmed - Persaud T, Walling M, Geoghegan T, Buckley O, Stunell H, Torreggiani WC. Ultrasound-guided removal of Implanon devices. Eur Radiol. 2008;18(11):2582-2585.
doi pubmed - Nelson AL, Sinow RM. Real-time ultrasonographically guided removal of nonpalpable and intramuscular Norplant capsules. Am J Obstet Gynecol. 1998;178(6):1185-1193.
doi - Merck. Nexplanon. Revised 2013; Available from: http://www.merck.com/product/usa/pi_circulars/n/nexplanon/nexplanon_pi.pdf.
- James P, Trenery J. Ultrasound localisation and removal of non-palpable Implanon implants. Aust N Z J Obstet Gynaecol. 2006;46(3):225-228.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
