| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 5, Number 1, March 2016, pages 41-44
Delayed Ureteral Insufficiency After Ureteral Obstruction During Total Laparoscopic Hysterectomy: Utility of Cystoscopy for the Intraoperative Detection of Obstruction, and for the Avoidance of Postoperative Surgical Intervention
Takashi Miyatakea, c, Takeya Haraa, Shinnosuke Komiyaa, Naoko Komuraa, Asuka Tanakaa, Serika Kanaoa, Masumi Takedaa, Ai Miyoshia, Mayuko Mimuraa, Masaaki Nagamatsua, Kazuhide Ogitab, Takeshi Yokoia
aDepartment of Obstetrics and Gynecology, Senshu Regional Medical Center for Women’s and Children’s Health, Kaizuka City Hospital, Kaizuka, Osaka, Japan
bDepartment of Obstetrics and Gynecology, Senshu Regional Medical Center for Women’s and Children’s Health, Rinku General Medical Center, Osaka, Japan
cCorresponding Author: Takashi Miyatake, Department of Obstetrics and Gynecology, Kaizuka City Hospital, 3-10-20, Hori, Kaizuka, Osaka 5970015, Japan
Manuscript accepted for publication December 10, 2015
Short title: Ureteral Insufficiency After Hysterectomy
doi: http://dx.doi.org/10.14740/jcgo376w
| Abstract | ▴Top |
Urinary tract injury after laparoscopic hysterectomy is a serious complication that necessitates surgery if it is detected late. We report a case of a 47-year-old woman who had a delayed diagnosis of ureteral stenosis after total laparoscopic hysterectomy. Intraoperative cystoscopy contributed to injury management.
Keywords: Laparoscopic hysterectomy; Urinary tract injury; Ureteral stenosis
| Introduction | ▴Top |
Total laparoscopic hysterectomy has become a standard procedure for uterine diseases of benign and of low-risk malignancy [1-3]. Urinary tract injuries are currently serious complications of hysterectomy [4], because of the anatomical proximity between the uterus and lower urinary tract.
Recently, the incidence of ureteral injury on total laparoscopic hysterectomy is estimated to be 0.73% and this is lower than that of previous publications [5, 6]. Intraoperative management of ureteral injury is preferable and late detection of urinary tract injury requires further intervention [7-9]. For the detection of bladder and ureteral injuries, intraoperative cystoscopy is proposed and the utility has been reported [10, 11].
Here, we present a case of delayed ureteral insufficiency due to ureteral ligation during total laparoscopic hysterectomy, and intraoperative cystoscopy was effective for the detection of the ureteral obstruction and for avoidance of surgical intervention after the delayed diagnosis.
| Case Report | ▴Top |
A 47-year-old woman, with no specific clinical history, was referred to our hospital, suffering from hypermenorrhea. MRI described uterine myoma with a diameter of 3 cm and thickening of the anterior uterine wall, indicating uterine adenomyosis (Fig. 1). A total laparoscopic hysterectomy was performed. During the operation, the right ureter was dissected from the pelvic brim to the root of the cardinal ligament by blunt dissection. There was endometriotic adhesion around the right cardinal ligament and the dissection was slightly difficult with stiffness. The uterus was maneuvered to the opposite side with a manipulator, and the right uterine vessels and cardinal ligament were sutured, coagulated and cut, while maintaining an adequate distance from the right ureter (Fig. 2). After removal of the uterus and closure of the vaginal cuff, intravenous dye (indigo carmine) was administered. Cystoscopy was performed for the assessment of ureteral patency. Thirty minutes of observation on the cystoscopy did not prove the right-side urinary flow and the right hydroureter was detected by laparoscopic abdominal inspection (Fig. 3). This indicated that the ligation of the right ureter was caused by the cardinal ligament suture. The suture was cut, the right ureter nearer the cardinal ligament was dissected, and no bleeding from uterine vessels was confirmed. Urinary flow from the right ureteral orifice was confirmed with a repeat cystoscopy, and the operation was completed. The total operation time was 260 min, and the time interval from the cardinal ligation to the release of the suture was estimated to be 134 min.
 Click for large image | Figure 1. Preoperative MRI of the lower abdomen and pelvis; T2 weighted sagittal section image. Protruded tumor at the uterine fundus 3 cm in diameter and thickening of uterine anterior wall. |
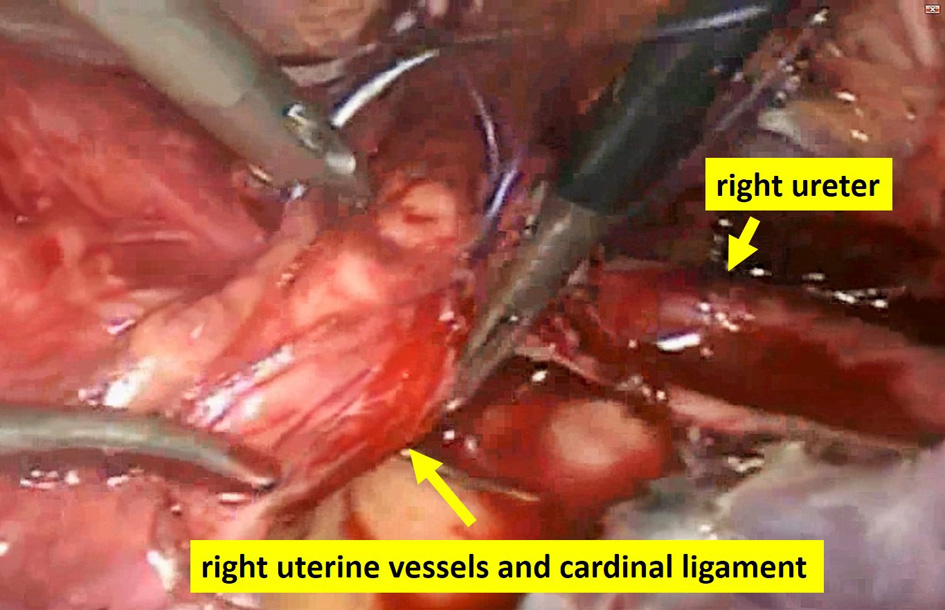 Click for large image | Figure 2. Suturing uterine vessels and cardinal ligament; uterine cervix is maneuvered up with the uterine manipulator. With a sufficient distance from the right ureter, right uterine vessels and cardinal ligament were sutured and cut. |
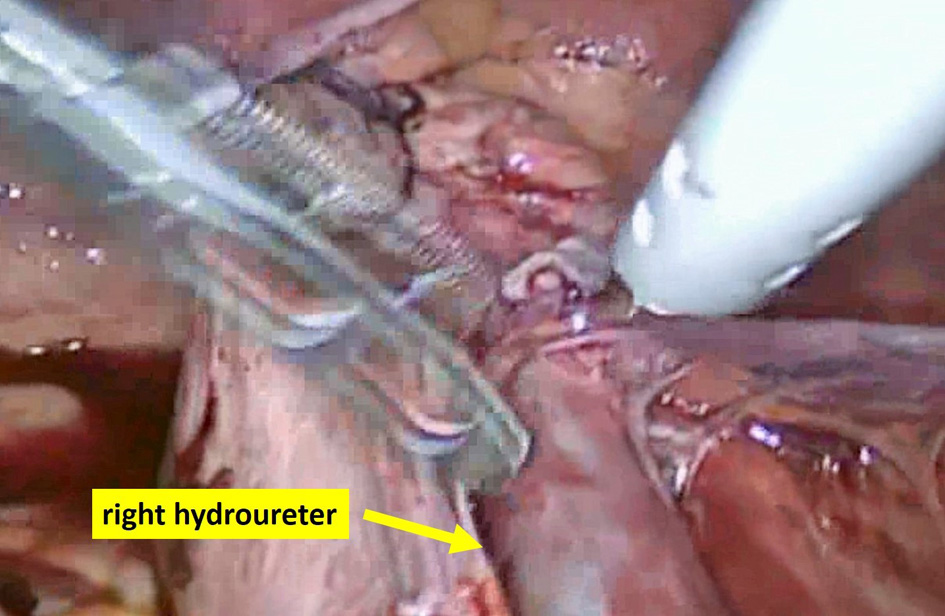 Click for large image | Figure 3. Laparoscopic findings of the right hydroureter; obstruction of the ureter may have occurred with suture of the cardinal ligament. |
On postoperative day 2, the patient reported a pain in the right lower back and serum creatinine was elevated to 1.0 mg/dL. Trans-abdominal ultrasonography and abdominal CT scan revealed a dilatation of the right ureter from the right renal pelvis to the vesicoureteral transitional region (Fig. 4). Initial management was intended to be conservative, as there was no urinary overflow seen in the CT image, and abdominal X-ray imaging just after CT scan showed urinary flow from the right side to the bladder. We considered that there was transient ureteral insufficiency, and not ureteral obstruction, and expected spontaneous recovery of ureteral function.
 Click for large image | Figure 4. CT scan of the abdomen, with contrast agent injection, on postoperative day 2; dilatation of the right ureter and renal pelvis indicates ureteral obstruction. |
On postoperative day 4, abdominal CT scan showed urinary overflow from the right renal pelvis. Right ureteral stenosis was diagnosed and a double-J stent was inserted to the right ureter for the maintenance of ureteral patency. Additionally, two sutures on the right side of the vaginal cuff were transvaginally removed for the release of tension at the right parametrium region.
An attempt to remove the right double-J stent was made on postoperative day 18. Intravenous pyelogram after the removal showed obstruction and stenosis at the right ureter. Ureteral patency was considered to be impossible without the double-J stent. Therefore, the right double-J stent was inserted again. She was discharged on day 21.
Four months after surgery, removal of the right double-J stent was attempted again. Prior to the removal, no stenosis was observed with the ureteroscope. The double-J stent was removed and intravenous pyelogram after 4 days described good urinary flow with no obstruction (Fig. 5).
 Click for large image | Figure 5. Intravenous pyelogram after the removal of double-J stent; 15-min X-ray; good bilateral ureteral flows with no obstruction. |
It has been over 20 months since the surgery and the patient has been free from symptoms and the urologic parameters have been normal. Neither hydroureter nor urinary overflow has been detected with ultrasonography.
| Discussion | ▴Top |
In a recent systemic review on laparoscopic hysterectomy, overall urinary tract injury occurs in 0.73% of laparoscopic hysterectomy and ureteral injury rate ranges from 0.02% to 0.4% [6]. The earlier publication reports that the incidence of ureteral injury during gynecologic laparoscopy ranges from 1% to 2% [12]. Although there is no statistical review, the incidence of ureteral injury appears to have fallen and is now comparable to abdominal hysterectomy. The technical issues of laparoscopic hysterectomy have improved with the spread and standardization of laparoscopic hysterectomy.
The reported risk factors of ureteral injuries are anatomic distortion, such as previous pelvic surgery, endometriosis, pelvic adhesions, enlarged uteri, adnexal masses, cervical and broad ligament fibroids, as well as congenital anomalies [12]. Ureteral injuries during laparoscopic hysterectomy occur most frequently on the right side [12, 13]. The present case includes the risk factors of pelvic adhesions, enlarged uteri and similarly to other reports, ureteral injury occurred at the right side. We have dissected the right ureter to the caudal ligament and sutured the ligament with sufficient distance from the ureter; however, endometriotic adhesion leads to the insufficient separation of the ureter and causes an unexpected route of the ureter within the caudal ligament. It is not clear whether the suture of the caudal ligament directly ligated the ureter, or an adjacent suture caused the ureter to be intensely flexed.
For the ureteral injury, the literature reports the importance of intraoperative management. When injury is discovered during surgery, correction of the injury can be repaired with minimal risk of long-term consequences [9]. Retrograde stenting and deligation are recommended intraoperative options for the ureteral injury [14]; however, in cases, neoureterocystostomy, transureteroureterostomy or nephrectomy are necessary. Sakellariou et al reported that, in postoperatively diagnosed ureteral injuries, catheterization failed in 28/44 (65.9%) cases and surgical re-exploration was necessary [8]. In the present case, suture removal improved the hydroureter. The suture of the caudal ligament for 134 min critically influenced ureteral obstruction and the delayed ureteral insufficiency. Even if urinary flow was confirmed with cystoscopy after the suture removal, we should have considered additional intraoperative retrograde stenting. However, there is little information for the estimation of ureteral function after injury, and the apparent recovery of ureteral function was confirmed by cystoscopy. It is possible that, without the intraoperative removal of the suture, postoperative surgical intervention for ureteral obstruction would have been necessary.
The intraoperative utility of cystoscopy has been reported in laparoscopic hysterectomy [10, 11]. Ribeiro et al detected ureteral obstruction which occurred in 3.4% (4/118) of laparoscopic hysterectomies [10]. All complications were found with cystoscopy and immediately resolved, and there were no postoperative ureteral problems. With the improvement of laparoscopic techniques and lowered incidence of urinary tract injuries, it is not clear if cystoscopy should be done routinely. The value of intraoperative cystoscopy in laparoscopic hysterectomy should be further argued. At our hospital, we routinely perform intraoperative cystoscopy on all laparoscopic hysterectomies, and it has contributed to the detection and management of ureteral obstruction in the present case.
In conclusion, we encountered a case of delayed ureteral insufficiency after laparoscopic hysterectomy. Management was done with a double-J stent and surgical intervention was avoided. Cystoscopy is considered to be useful for the intraoperative detection and management of ureteral injury.
| References | ▴Top |
- Bijen CB, Vermeulen KM, Mourits MJ, de Bock GH. Costs and effects of abdominal versus laparoscopic hysterectomy: systematic review of controlled trials. PLoS One. 2009;4(10):e7340.
doi pubmed - Jonsdottir GM, Jorgensen S, Cohen SL, Wright KN, Shah NT, Chavan N, Einarsson JI. Increasing minimally invasive hysterectomy: effect on cost and complications. Obstet Gynecol. 2011;117(5):1142-1149.
doi pubmed - Pawlowicz PS, Ajdacka U. The role of laparoscopy in the surgical treatment of endometrial cancer. Wideochir Inne Tech Maloinwazyjne. 2015;10(1):44-48.
doi pubmed - Cordon BH, Fracchia JA, Armenakas NA. Iatrogenic nonendoscopic bladder injuries over 24 years: 127 cases at a single institution. Urology. 2014;84(1):222-226.
doi pubmed - Mamik MM, Antosh D, White DE, Myers EM, Abernethy M, Rahimi S, Bhatia N, et al. Risk factors for lower urinary tract injury at the time of hysterectomy for benign reasons. Int Urogynecol J. 2014;25(8):1031-1036.
doi pubmed - Adelman MR, Bardsley TR, Sharp HT. Urinary tract injuries in laparoscopic hysterectomy: a systematic review. J Minim Invasive Gynecol. 2014;21(4):558-566.
doi pubmed - Goris-Gbenou MC, Arfi N, Mitach A, Rashed S, Lopez JG. A case of delayed diagnosis of bilateral ureteral and bladder injury after laparoscopic hysterectomy: an unusual complication. Case Rep Urol. 2012;2012:817010.
doi - Sakellariou P, Protopapas AG, Voulgaris Z, Kyritsis N, Rodolakis A, Vlachos G, Diakomanolis E, et al. Management of ureteric injuries during gynecological operations: 10 years experience. Eur J Obstet Gynecol Reprod Biol. 2002;101(2):179-184.
doi - Chan JK, Morrow J, Manetta A. Prevention of ureteral injuries in gynecologic surgery. Am J Obstet Gynecol. 2003;188(5):1273-1277.
doi pubmed - Ribeiro S, Reich H, Rosenberg J, Guglielminetti E, Vidali A. The value of intra-operative cystoscopy at the time of laparoscopic hysterectomy. Hum Reprod. 1999;14(7):1727-1729.
doi pubmed - Indraratna PL, Walsh CA, Moore KH. Intra-operative cystoscopy in gynaecological surgery: a brief overview. Aust N Z J Obstet Gynaecol. 2011;51(3):272-275.
doi pubmed - Manoucheri E, Cohen SL, Sandberg EM, Kibel AS, Einarsson J. Ureteral injury in laparoscopic gynecologic surgery. Rev Obstet Gynecol. 2012;5(2):106-111.
pubmed - Wattiez A, Soriano D, Cohen SB, Nervo P, Canis M, Botchorishvili R, Mage G, et al. The learning curve of total laparoscopic hysterectomy: comparative analysis of 1647 cases. J Am Assoc Gynecol Laparosc. 2002;9(3):339-345.
doi - Aslan P, Brooks A, Drummond M, Woo H. Incidence and management of gynaecological-related ureteric injuries. Aust N Z J Obstet Gynaecol. 1999;39(2):178-181.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
