| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 7, Number 3-4, November 2018, pages 72-75
Advanced Diabetic Eye Disease in Pregnancy
Puspha Ramana, b, Bethel Indira Livingstonea
aHospital Tuanku Jaafar Seremban, Negeri Sembilan, Malaysia
bCorresponding Author: Puspha Raman, Ophthalmology Department, Hospital Tuanku Jaafar Seremban, Negeri Sembilan, Malaysia
Manuscript submitted March 31, 2018, accepted July 19, 2018
Short title: Diabetic Retinopathy in Pregnancy
doi: https://doi.org/10.14740/jcgo487w
| Abstract | ▴Top |
Women with pre-gestational diabetes are at risk of progression of diabetic retinopathy during the pregnancy. The adverse effects of pregnancy on retinal status persist into the first year postpartum. Diabetic eye disease may develop for the first time during pregnancy, and visual impairment at this stage has serious implications for both the patient and her family. Established sight-threatening retinopathy should be treated at an earlier stage in pregnant women compared to non-pregnant diabetics with a similar disease. This case report highlights a case of diabetic retinopathy in pregnancy which progressed rapidly and was successfully treated with timely surgical intervention resulting in good final visual outcome.
Keywords: Diabetic retinopathy; Pregestational diabetes; Vitrectomy; Advanced diabetic eye disease
| Introduction | ▴Top |
Retinopathy affects 20% to 27% of women with diabetes mellitus in the reproductive age group. Women with pre-gestational diabetes are at risk of progression during the pregnancy. The adverse effects of pregnancy on retinal status persist into the first year postpartum [1]. Diabetic eye disease may develop for the first time during pregnancy, and visual impairment at this stage has serious implications for both the patient and her family. Established sight-threatening retinopathy should be treated at an earlier stage in pregnant women compared to non-pregnant diabetics with a similar disease.
In the past, prognosis for pregnancy in diabetic women with microvascular changes was so poor that many physicians advised either avoidance or termination of pregnancy in high risk patients. Currently, meticulous control of the glycemic levels during pregnancy has been shown to decrease in the incidence of fetal malformations and maternal complications. The risk factors for the progression of retinopathy in pregnancy are severity of retinopathy at conception, adequacy of treatment, duration of diabetes, metabolic control before pregnancy, and the presence of additional vascular damage, such as nephropathy and hypertension [2].
This case report highlights a case of diabetic retinopathy in pregnancy which progressed rapidly and was successfully treated with timely surgical intervention and achieved good final visual outcome.
| Case Report | ▴Top |
Madam G, a 31-year-old primigravida, with underlying type 2 diabetes mellitus was referred for diabetic retinopathy assessment by her antenatal care provider in her first trimester. However, patient did not attend any diabetic retinopathy screening until her 22nd week of gestation due to logistics problem.
Upon presentation on her first diabetic retinopathy screening, she was complaining of floaters in her both her eyes. She said the floaters started about 2 weeks prior to the visit and slowly improving over the time. She also was complaining of bilateral mild blurring of vision. No history flashes of lights, redness or ocular pain. No history of preceding trauma.
She was diagnosed to have type 2 diabetes mellitus 2 years ago. She initially presented with diabetic ketoacidosis which required intubation and intensive care unit admission for 2 weeks. She was on oral Glucovance (Glyburide and Metformin HCl) 5/500 mg BD till her pregnancy. She had been having fluctuating glycemic control. Her serum glycosylated hemoglobin level (HbA1C) at her first antenatal visit was 8.5%. Her antenatal care provider has switched her into insulin regime during this pregnancy and her blood sugar profile was within acceptable range till the current visit. No evidence of other end target organ damage. Her antenatal scans were normal. Her blood pressure was within normal limits.
Patient was a low myope with other no significant ocular comorbidity. According to her, she has been on yearly diabetic retinopathy screening prior to the pregnancy and was told to have normal fundus with no retinopathy changes. She had been married for 5 years and was investigated before for primary infertility. She denied of smoking and alcohol intake. Her visual acuity was 6/36 in her right eye and 6/60 in her left eye. Anterior segment examination was unremarkable with IOP of 13mm Hg and 15mm Hg in her right and left eye respectively. Fundus examination of right eye revealed presence of dense preretinal hemorrhage below the inferior vascular arcade, in association with florid disc neovascularisation (Fig. 1). There was also diffuse vitreous hemorrhage with minimal obscuration for fundus visualisation. Examination of left eye also revealed multiple dots and flamed shaped hemorrhages, together with neovascularisation at superotemporal arcade. Arteriovenous ratios were 1:2 bilaterally with peripapillary cotton wool spots.
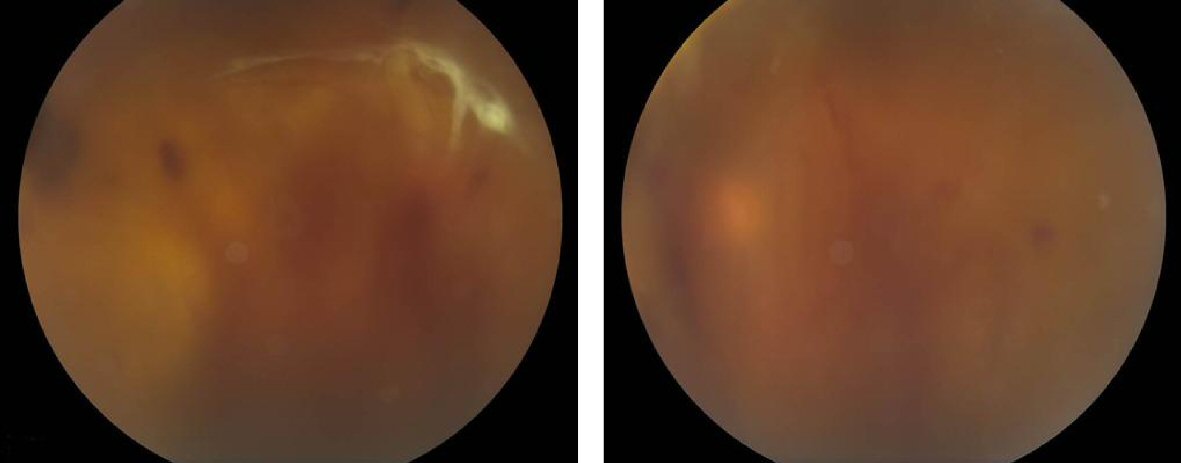 Click for large image | Figure 1. Bilateral colour fundus photograph showing diffuse vitreous hemorrhage with no fundus details. Figure on right shows right eye dense vitreous hemorrhage centrally with tractional retinal detachment inferiorly. Superior rhegmatogenous retinal detachment with subretinal fluid can be seen. Figure on left showing left eye with moderately dense, dispersed vitreous hemorrhage. No retinal detachment detected. |
Urgent pan retinal photocoagulation (PRP) was performed in her both eyes on the same day and at subsequent weekly visits. Her diabetic control has improved with the HbA1c of 6.5%. Evidence of regression was seen as early as 2 weeks after PRP. The right eye received a total of 2,100 spots of laser burns and the left eye 1,795 of laser burns.
However, in her third trimester she developed recurrent vitreous hemorrhages with the right eye vision deteriorated to hand movement (HM). At 33 weeks of gestation, the fundus examination revealed tractional retinal detachment (TRD) in her right eye, which was threatening the macula (2). Vitrectomy was proposed for non-clearing vitreous hemorrhage and TRD. However, patient was not keen to perform vitrectomy during pregnancy, although she was aware of the blinding complications. After careful counselling and discussion, it was proposed to defer vitrectomy till the delivery. She underwent elective Cesarean section at the 37th week for suspected big baby. She delivered a healthy 3.8 kg baby boy with no postnatal complication. At 2 weeks postpartum, right eye developed inferior combined rhegmatogenous and TRD with a tear identified at 2 o’clock position.
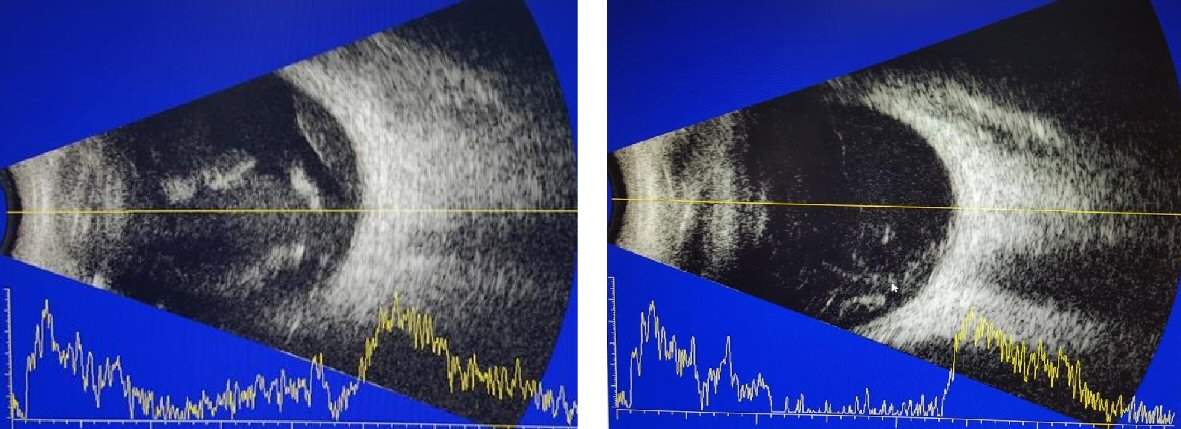 Click for large image | Figure 2. B scan prior to vitrectomy. |
She underwent pars plana vitrectomy, epiretinal membrane removal, indirect laser photocoagulation and sclera buckling with a No.42 silicone encircling band. The vitreous cavity was filled with 14% C3F8.
She underwent vitrectomy for her left eye for nonclearing vitreous hemorrhage in 1-month interval. At 12 months after the first vitrectomy, the retina remained attached with a corrected vision of 6/9 in the right eye and 6/6 in the left eye (Fig. 3).
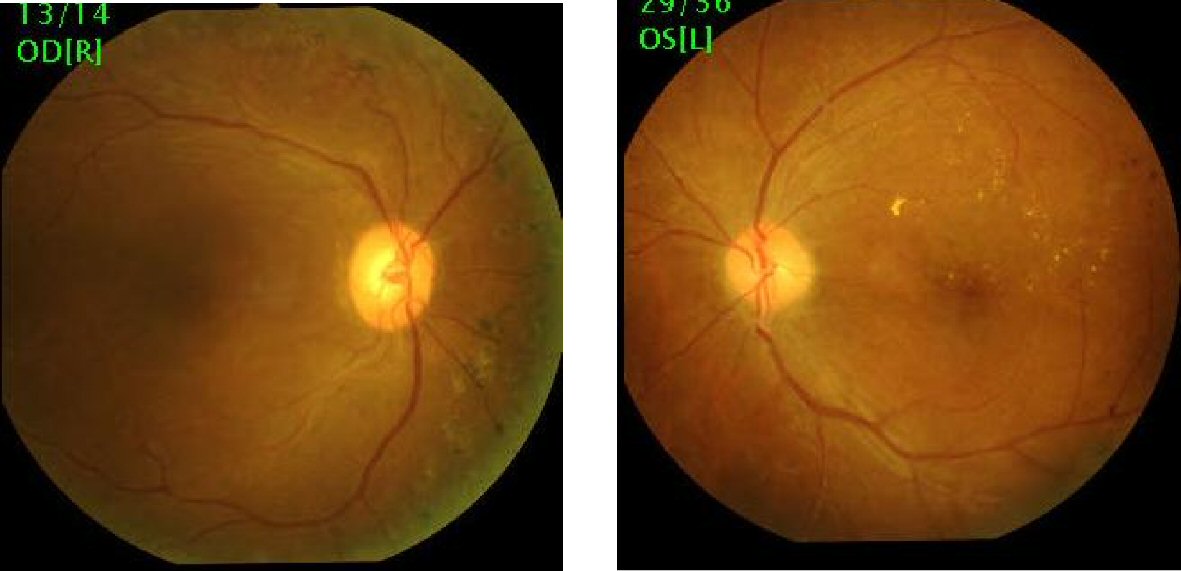 Click for large image | Figure 3. Post vitrectomy colour fundus photographs showing flat retina. |
| Discussion | ▴Top |
Diabetic retinopathy may develop for the first time during pregnancy, and visual loss at this stage has serious implications for both the patient and her family. The results of the Diabetes in Early Pregnancy Study (DIEP) demonstrated that women with mild or more severe retinopathy at the time of conception were at high risk for progression of retinopathy during pregnancy [3]. The adverse effects of pregnancy on retinal status can persist into the first year postpartum.
Several important risk factors can contribute to the aggravation of diabetic retinopathy, including the pregnancy itself, duration of diabetes, elevated glycohemoglobin level, rapid normalisation of blood glucose level, hypertension, renal disease and the degree of retinopathy at the beginning of pregnancy [2]. In our patient, the important risk factor was poorly controlled diabetes prior to pregnancy and the rapid normalisation of sugar with the insulin commencement in the first trimester. DIEP study has shown that those women with the greatest reduction in HbA1C over the first 14 weeks of pregnancy were at an increased risk of progression of retinopathy [3]. The National Institute for Health and Clinical Excellence (NICE) in the United Kingdom recommends that rapid optimisation of poor glycemic control should be deferred at least until after retinal assessment [4].
The screening and management of diabetic retinopathy in pregnancy is challenging. Close cooperation and communication among patient and her obstetrician, ophthalmologist and physician is essential in developing an individual-based management plan.
Ideally, diabetic women should be examined comprehensively by an ophthalmologist prior to conception. If this window of opportunity is missed, the examination must be performed as soon as possible in the first trimester. According to NICE guidelines, pregnant women with pre-existing diabetes should be offered retinal assessment by digital imaging following their first antenatal clinic appointment and again at 28 weeks if the first assessment is normal. If any diabetic retinopathy is present, additional retinal assessment should be performed at 16 - 20 weeks. It is also recommended that women who have preproliferative diabetic retinopathy or any form of referable retinopathy diagnosed during pregnancy have ophthalmological follow-up for at least 6 months after the birth of the baby (2008, amended 2015) [4].
In our case, patient has missed her diabetic retinopathy screening early in the pregnancy. Patient was not aware of the possibility of retinopathy progression in pregnancy. Although missing appointments are individual choice, the attending obstetricians also must ensure that his or her patients are screened for diabetic retinopathy and create awareness among patient regarding the blinding complications of diabetic retinopathy. The value of prepregnancy counselling regarding the potential risks and consequences to vision should not be overlooked and greater patient education would be beneficial.
Treatment of diabetic retinopathy during pregnancy is guided by the same criteria as applied to patients who are not pregnant. Studies have suggested that delaying treatment because of the hope that DR will regress after delivery, may lead to worse outcome. All pregnant patients with DR need close ophthalmic follow-up and early intervention. The standard of care for treatment of proliferative diabetic retinopathy is laser photocoagulation therapy [5]. PRP also recommended in the setting of severe NPDR because of the chance of rapid progression in pregnancy. The diagnosis of sight threatening retinopathy can be usually made with dilated fundus examination alone. Mydriasis is best achieved using tropicamide or phenylephrine HCl, both of which are category C drugs. Although fluorescein angiography is not teratogenic, most ophthalmologists defer its use after delivery.
Our patient was not given the option of anti-vascular endothelial growth factor (anti-VEGF) injection prior to the surgery. The effects of intravitreal anti-VEGF injections during pregnancy are unknown. There are reports of uncomplicated cases who have received anti VEGF in pregnancy [6]. However, there are also a few case reports of early miscarriages in patients who received anti-VEGF injections during early pregnancy [7]. It is hypothesized that although anti-VEGF formulations, such as bevacizumab and ranibizumab, do not likely cross the placental barrier in large quantities, they may act on placental circulation by inhibiting VEGF-A; and the long terms effects are unknown. If an anti-VEGF injection is recommended, the patient must be well-educated about the potential risks and the pregnancy must be closely monitored.
Vitrectomy can be performed during pregnancy if there are clinical indications. The most common indications for surgery are nonclearing vitreous hemorrhage, TRD, and neovascular glaucoma. It is imperative to ensure the assistance of an experienced anesthetist to anticipate pregnancy-related anesthetic complications. It is also possible to carry out vitrectomy under local anesthesia in high risk patients. There is little information in the literature regarding the surgical management of diabetic retinopathy associated with pregnancy and its outcome. Chan et al identified that the presence of combined rhegmatogenous and TRD and neovascular glaucoma associated with the worst outcome [8].
In summary, sight-threatening diabetic retinopathy associated with pregnancy is rare, but it can have dire consequences for mothers and their children. In addition, PDR may not regress in the postpartum period and close follow-up should be extended in the postpartum period in this subgroup of patients until retinopathy is stabilised.
Conflict of Interest
All authors declare no conflict of interest.
| References | ▴Top |
- Diabetes C, Complications Trial Research G. Effect of pregnancy on microvascular complications in the diabetes control and complications trial. The Diabetes Control and Complications Trial Research Group. Diabetes Care. 2000;23(8):1084-1091.
doi - Mallika P, Tan A, S A, T A, Alwi SS, Intan G. Diabetic retinopathy and the effect of pregnancy. Malays Fam Physician. 2010;5(1):2-5.
pubmed - Chew EY, Mills JL, Metzger BE, Remaley NA, Jovanovic-Peterson L, Knopp RH, Conley M, et al. Metabolic control and progression of retinopathy. The Diabetes in Early Pregnancy Study. National Institute of Child Health and Human Development Diabetes in Early Pregnancy Study. Diabetes Care. 1995;18(5):631-637.
doi pubmed - [CG63] NICE guidelines. Diabetes in pregnancy: management of diabetes and its complications from pre-conception to the postnatal period. http://www.nice.org.uk/guidance/cg63/chapter/guidance, 2015.
- Cheung A, Scott UI, Fekrat S. Ocular changes during pregnancy. Eyenet. American Academy of Ophthamology. 2013.
- Rosen E, Rubowitz A, Ferencz JR. Exposure to verteporfin and bevacizumab therapy for choroidal neovascularization secondary to punctate inner choroidopathy during pregnancy. Eye (Lond). 2009;23(6):1479.
doi pubmed - Petrou P, Georgalas I, Giavaras G, Anastasiou E, Ntana Z, Petrou C. Early loss of pregnancy after intravitreal bevacizumab injection. Acta Ophthalmol. 2010;88(4):e136.
doi pubmed - Chan WC, Lim LT, Quinn MJ, Knox FA, McCance D, Best RM. Management and outcome of sight-threatening diabetic retinopathy in pregnancy. Eye (Lond). 2004;18(8):826-832.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
