| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Review
Volume 8, Number 2, June 2019, pages 33-38
Are Pelvic Stabilizing Exercises Effective for Postpartum Pelvic Girdle Pain? A Literature Review
Asuka Sakamotoa, b, Kazuyoshi Gamadaa, c
aGraduate School of Medical Technology and Health Welfare Sciences, Hiroshima International University, 555-36 Kurosegakuendai Higashihirsoshima-shi, Hiroshima, 739-2631, Japan
bFaculty of Rehabilitation Sciences, Nishikyushu University, 4490-9 Ozaki, Kanzaki, Saga, 842-8585, Japan
cCorresponding Author: Kazuyoshi Gamada, Graduate School of Medical Technology and Health Welfare Sciences, Hiroshima International University, 555-36 Kurosegakuendai Higashihirsoshima-shi, Hiroshima, 739-2631, Japan
Manuscript submitted May 16, 2019, accepted June 13, 2019
Short title: Pelvic Stabilizing Exercises for Postpartum PGP
doi: https://doi.org/10.14740/jcgo552
| Abstract | ▴Top |
The effectiveness of exercises to prevent or relieve postpartum pelvic girdle pain (PGP) has been investigated for decades. Although multiple treatment options are available, evidence supporting specific forms of intervention for PGP remains limited. Thus, the effectiveness of exercises and treatments for persistent postpartum PGP has not yet been established. The aim of this literature review was to clarify the effectiveness of exercises based on a review of randomized controlled trials including postpartum women with persistent PGP. We performed a broad search for eligible studies published before May 1, 2018 using the following electronic databases; PubMed, Medline, Pedro, Sage Journal, Google Scholar and the Cochrane Library. Comprehensive combinations of key words were utilized for these searches. Data were evaluated using a review process. The initial online search identified 184 potential studies and six of these studies met the specified criteria. All studies investigated the interventional effects of pelvic stabilizing exercises by assessing pain intensity, physical examination and disability questionnaires. In terms of effectiveness, a significant positive impact on pelvic pain intensity was reported as a result of stabilizing exercise programs for postpartum PGP. There were no adverse events reported in any of these studies. This review demonstrates the paucity of methodologically rigorous research to help healthcare practitioners make reliable decisions regarding the effectiveness of physical exercises for postpartum PGP. An individually tailored program with stabilizing exercises involving all relevant muscles delivered under the guidance of a therapist achieved high patient compliance and was shown to be effective for PGP.
Keywords: Postpartum women; Pelvic girdle pain; Pelvic stabilizing exercises
| Introduction | ▴Top |
Relieving pain and preventing progression to a chronic condition is of great interest for health practitioners involved with women’s postpartum health. The effectiveness of exercises to prevent or relieve postpartum pelvic girdle pain (PGP) has been investigated for decades. European guidelines for PGP support individualized physical therapy, exercises, acupuncture and massage for the treatment of postpartum PGP [1], although the positive impact of physical therapy and exercises, and the effectiveness of the various components of these programs remain unclear. Currently there are indications that acupuncture and stabilizing exercises are effective treatments during pregnancy and postpartum. Elden et al [2] concluded that stabilizing exercise and acupuncture caused a reduction of PGP in the great majority of women within 12 weeks after delivery. Passive treatment options include acupuncture, manual therapy and pelvic belts [3]. More active treatment options include specific exercises [4], exercises with strategies to either increase or decrease muscle activation [5], as well as more general exercises such as hydrotherapy. Specific education related to PGP is also an important aspect of physiotherapy [5]. Although multiple treatment options are available, evidence supporting specific forms of intervention for PGP remains limited [6]. Thus, evidence showing the effectiveness of exercises and treatments for persistent postpartum PGP has not yet been established.
The effectiveness of treating pelvic alignment also remains controversial in clinical practice, evidence or guidelines. The theoretical model of lumbopelvic pain describes a self-locking mechanism of the pelvic joints based on the principles of form closure and force closure [7]. Local stabilizing muscles (the transverse abdominal muscle, lumbar multifidus, and pelvic floor muscles) are reported to play important roles in load transfer in the lumbopelvic region [8]. It has been suggested that improving the activation pattern of these local stabilizing muscles results in functional improvement in patients with lumbopelvic pain [1]. For women with PGP during pregnancy, treatment including specific stabilizing exercises for local muscles may effectively prevent persistent PGP after delivery [9]. The aim of this literature review was to clarify the effectiveness of exercises based on a review of randomized controlled trials among postpartum women with persistent PGP.
| Literature Search | ▴Top |
This literature review followed the preferred reporting items listed in review guidelines [10]. For this literature review, we performed a broad search for eligible studies published before May 1, 2018 using the following electronic databases: PubMed, Medline, Pedro, Sage Journal, Google Scholar and the Cochrane Library. The following key words were utilized for these searches: comprehensive combinations of key words including (“pelvic girdle pain” or “pelvic pain”) plus (“exercise” or “treatment” or “physical therapy” or “physiotherapy”) plus (“postpartum women” or “postnatal women” or “after delivery” or “childbirth”). Articles reviewed were published or available online between January 1, 2000 and April 30, 2018. The following eligibility criteria were applied to all papers found in order to ensure that the studies used were relevant: 1) The articles were written in English; 2) Publication type was a prognostic study, longitudinal study or prospective cohort study; 3) Study population consisted of women experiencing PGP in the postpartum period or pregnancy and postpartum periods; 4) Outcomes included the effect of stabilizing exercise. Exclusion criteria were: 1) Publication type was a tutorial review, anecdotal report, abstract form, systematic review or case report; 2) Study population was a mixed sample comprised of women with PGP and LBP or women with LBP only; 3) Study period was limited to pregnancy only; 4) Outcomes focused on other symptoms such as incontinence, diastasis recti abdominis, fracture and pelvic fusion; 5) Type of delivery was cesarean section; 6) Treatment included acupuncture, surgery, pharmaceutical agents, injection, yoga or Pilates. Prior to data collection, the titles and abstracts were initially screened to identify potentially relevant studies. Each article was screened for the relevance of the study in relation to the eligibility criteria and the study aim. Duplicate articles were excluded.
| Literature Retrieved | ▴Top |
Results of the search
The initial online search identified 184 potential studies and six of these studies met the specified criteria [4, 11-15]. The flow diagram is presented in Figure 1.
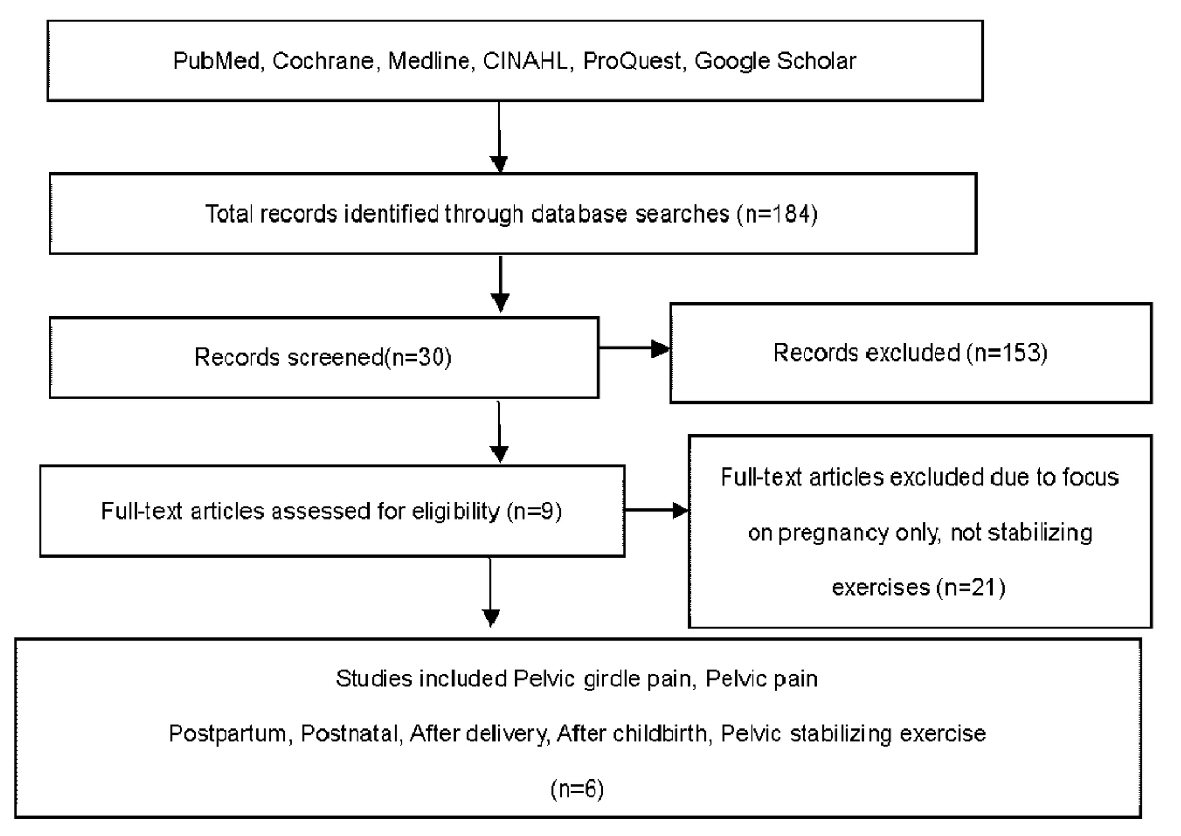 Click for large image | Figure 1. Literature search flow diagram. |
Included studies
All six of the included studies were designed as randomized controlled trials with sample sizes ranging from 16 [14] to 88 [13] (Table 1, [4, 11-15]). All studies investigated the interventional effects of pelvic stabilizing exercises by assessing pain intensity, physical examination and disability questionnaires.
 Click to view | Table 1. Studies of Pelvic Stabilizing Exercise |
Outcome measures
Responses on disability questionnaires were the primary outcome measure in all of these studies. Pain intensity on visual analogue scale (VAS), provocation tests, mobility of pelvic joints (palpation), active straight leg raising (ASLR) test, physical endurance and health-related quality of life (HRQOL) were also measured to compare with those in control groups and to observe the effects of the intervention program.
Intervention duration
The study periods ranged from 8 weeks to 2 years follow-up (Table 1). The participants performed pelvic stabilizing exercises for 4 to 16 weeks after delivery. Three of six studies recruited women with PGP 3 months after delivery [11, 13, 14].
Frequency of stabilizing exercises
Most studies set the duration of exercises at around 30 min per exercise session with a frequency of at least two times per day and 3 days a week. One study provided individual physical therapy sessions and set the exercise duration from 1 h to 90 min per session once a week. Minimum duration was 10 min per exercise [15]. The frequency of the exercises was not reported in three studies [4, 11, 12].
Adverse events
There were no reports of adverse events in any of the studies. However, 13 of 115 participants dropped out of the pelvic stabilizing exercise intervention due to new pregnancy or a preference to discontinue the exercises [11, 13]. Eighteen of 114 participants dropped out of the control group for the same reasons [11, 13]. Two of six studies did not report the number of participants who discontinued the exercises [12, 14]. One study found that three participants experienced worsening pain [11]. However, these researchers suggested that there were no risks of increased pain [11].
Intervention of stabilizing exercises
The interventions consisted of various exercise programs as indicated in Table 1. Interventions in three of the trials used stabilization exercises for either specific or core muscles, while the training program in the third trial focused on the diagonal trunk muscle system. The core stabilizing exercise program used by Stuge et al [4] focused on training the deep local muscles (transverse abdominal wall muscles with co-activation of the lumbar multifidus in the lumbosacral region) and global muscles (gluteus maximus, latissimus dorsi, oblique abdominal muscles, erector spinae, quadratus lumborum, and hip adductors and abductors). The initial focus of this exercise was on specific contraction of the transverse abdominal muscles. In addition to stabilizing exercises, postural correction techniques in different positions such as supine, crook lying, half sitting and prone were also employed for the intervention group in another trial. The specific pelvic stabilizing exercises reported by Gutke et al [13] focused on strengthening the transverse abdominal muscles, lumbar multifidus and the pelvic floor muscles, and on improving motor control and stability. Four of six studies had a physical therapist provide instructions regarding the specific pelvic stabilizing exercises [4, 12-14] and one study conducted a home exercise program that included individual guidance by a physical therapist every second week [13]. The remaining study used a 30-min video tape instruction for specific stabilizing exercises to investigate the value of graded exercises for the diagonal trunk muscle systems [11]. One study utilized exercise with a pelvic realignment device for attaining a more symmetrical pelvis [15].
The effects of stabilizing exercises
In terms of effectiveness, a significant positive impact on pelvic pain intensity was reported as a result of stabilizing exercise programs for postpartum PGP. One study found significant reductions in pain intensity in the morning and decreased fatigue in the evening during the intervention period and at 1- and 2-year follow-ups, with a better reduction of PGP in the intervention group compared to that in the control group [12]. In two studies utilizing home exercises, there were no significant differences in the results obtained by the group performing specific stabilizing exercises compared to control group outcomes [11, 13]. Gutke et al reported that pain frequency was significantly lower in the intervention group compared to that in the control groups at 3-month follow-up, but there were no significant differences with respect to pain intensity or other related variables such as HRQOL and wellbeing [13]. Mens et al (2000) [11] did not find any significant difference with respect to the severity of pain in the morning and evening or fatigue levels between the experimental group and either of the control groups. However, the intervention group scored better than the control groups with respect to changes in gluteal pain provoked by the posterior pelvic pain provocation (PPPP) test on the right side. Individual physical therapy focusing on specific stabilizing exercises with instruction by a physical therapist can contribute to decreasing pain and improving disability.
| Discussion | ▴Top |
This purpose of this literature review was to clarify the effectiveness of pelvic stabilizing exercise based on randomized controlled trials among postpartum women with persistent PGP. Six of 184 articles met the inclusion criteria and all of these studies examined the effectiveness of pelvic stabilizing exercises for persistent PGP in postpartum women. They encouraged patient compliance with their exercise program by emphasizing: 1) exercises designed to not provoke pain; 2) exercises performed under the supervision of a therapist; 3) use of a training diary; 4) gradually increased resistance of individually adapted exercises; and 5) the integration of muscle control into functional tasks. Although VAS was used to measure pain intensity in all six studies, a range of pain-related outcome measures was found across trials. The duration and frequency of intervention, adverse events, contents of specific stabilizing exercises and the effects of stabilizing exercises were noted in each of these six randomized controlled studies.
Compared to conventional exercises, specific pelvic stabilizing exercises more effectively relieved postpartum PGP that had persisted for more than 3 months after delivery. In the study by Stuge et al (2004) [4], a treatment program utilizing specific stabilizing exercises was compared to physical therapy without specific stabilizing exercises. The stabilizing exercise was meant to improve dynamic control of the lumbar segments and pelvic joints by activating local muscles in coordination with global muscles [4]. Greater effects were achieved when the participants were encouraged to compress the sacroiliac joints using forces acting across the joint during loading to ensure stability. However, activation of local muscles in coordination with global muscle was not examined in this study [4]. The anatomical structures responsible for stabilization are the ligaments and abdominal and pelvic muscles [7]. Compared to physical therapies without specific stabilizing exercises, the treatment program that included specific stabilizing exercises showed both statistically and clinically significant effects on pain, functional status, HRQOL and physical tests measured after 20 weeks of intervention and at 1 year postpartum. A 2-year follow-up study showed that low levels of pain and disability persisted in the exercise group and significant differences were noted between the physical therapy with specific stabilizing exercise and without specific exercising groups [12]. A treatment program with specific exercises that include both local and global muscle systems, individually adapted and guided by a physical therapist showed the greatest benefits [13, 14]. Those findings demonstrated that specific pelvic stabilizing exercises reduced pain intensity in the morning and decreased fatigue in the evening as well as improving disability. However, effects on the musculoskeletal system remain unclear. Further investigations are needed to identify the most effective elements in this type of individual intervention program and the extent of effects on the musculoskeletal mechanism.
The style of exercise instruction might have influenced the outcomes of these exercise programs as well as the number of participants who dropped out. Among the studies included in this review, only two thoroughly instructed and regularly supervised patients to ensure that exercises were correctly performed to involve all relevant muscles of the pelvic girdle [4, 14]. There were also marked differences across studies with respect to the type of exercises, frequency and duration, as well as the way the exercises and instructions were administered. In our review, the use of a video-tape and home exercise settings did not appear to contribute to the effectiveness of the program compared to that of patients receiving regular instruction from physical therapists. Compliance with the intervention is also likely to significantly influence the outcomes and is an important indicator of an intervention’s feasibility for future implementation. Among the trials included in our review, only one trial reported good compliance with zero participants dropped out [4]. In the study by Mens et al (2000) [11], 25% of the subjects terminated their exercise program due to pain, probably because the exercises were too intense. The types of instruction, frequency and intensity of exercises might have impacted the outcome of the stabilizing exercise program. Although most studies set 16 - 20 weeks, Mens et al set 8 weeks. The intervention programs in our review lasted for at least 6 weeks after delivery, inducing no significant adverse events. Thus, patient compliance should be considered in planning the style of instruction and the frequency and intensity of exercises.
Despite the comprehensive search, we identified only six randomized controlled trials that met our inclusion criteria. Three of the six selected trials demonstrated good methodological quality with blinded assessments and used standardized and validated data collection tools to ensure internal validity and robustness of the findings. However, there is a possibility that important studies were overlooked because we selected English language articles only. However, journals in another language might have published additional studies. Further studies are needed to provide conclusive evidence on the effects of pelvic stabilizing exercise to prevent persistent PGP in the postpartum period.
| Conclusions | ▴Top |
Although exercise is routinely recommended to postpartum women, this review demonstrates the paucity of methodologically rigorous research to help healthcare practitioners make reliable decisions regarding the effectiveness of physical exercises for postpartum PGP. We only included interventions with stabilization exercises and we excluded studies utilizing an intervention intended to optimize pelvic alignment, range of motion of the hip and/or thoracic spine, or the other elements. Further high-quality randomized trials with controlled co-interventions and/or standardized outcome measures are needed to identify the most effective combination of exercises as well as interventions for other physical elements that can reduce PGP and associated factors affecting health and well being.
Acknowledgments
None to declare.
Financial Disclosure
This work was supported by JSPS KAKENHI Grant Number 16K20807.
Conflict of Interest
The authors indicated no potential conflicts of interest.
| References | ▴Top |
- Stuge B. Pelvic girdle pain: examination, treatment, and the development and implementation of the European guidelines. Journal of the Association of Chartered Physiotherapists in Women's health. 2012;111:5-12.
- Elden H, et al. Predictors and consequences of long-term pregnancy-related pelvic girdle pain: a longitudinal follow-up study. BMC Musculoskelet Disord. 2016;17(276):1-13.
doi pubmed - Hilde G, Gutke A, Slade SC, Stuge B. Physical therapy interventions for pelvic girdle pain (PGP) after pregnancy. Cochrane Database of Systematic Reviews. 2016;11:1-24.
doi - Stuge B, Laerum E, Kirkesola G, Vollestad N. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: a randomized controlled trial. Spine (Phila Pa 1976). 2004;29(4):351-359.
doi - O'Sullivan PB, Beales DJ. Diagnosis and classification of pelvic girdle pain disorders—Part 1: a mechanism based approach within a biopsychosocial framework. Man Ther. 2007;12(2):86-97.
doi pubmed - Vleeming A, Albert HB, Ostgaard HC, Sturesson B, Stuge B. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J. 2008;17(6):794-819.
doi pubmed - Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567.
doi pubmed - Cohen SP. Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg. 2005;101(5):1440-1453.
doi pubmed - Liddle SD, Pennick V. Interventions for preventing and treating low-back and pelvic pain during pregnancy (Review). Cochrane Database of Systematic Reviews. 2015;(9):1-118.
doi pubmed - Burns PB, Rohrich RJ, Chung KC. The levels of evidence and their role in evidence-based medicine. Plast Reconstr Surg. 2011;128(1):305-310.
doi pubmed - Mens JM, Snijders CJ, Stam HJ. Diagonal trunk muscle exercises in peripartum pelvic pain: a randomized clinical trial. Phys Ther. 2000;80(12):1164-1173.
- Stuge B, Veierod MB, Laerum E, Vollestad N. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: a two-year follow-up of a randomized clinical trial. Spine (Phila Pa 1976). 2004;29(10):E197-203.
doi - Gutke A, Sjodahl J, Oberg B. Specific muscle stabilizing as home exercises for persistent pelvic girdle pain after pregnancy: a randomized, controlled clinical trial. J Rehabil Med. 2010;42(10):929-935.
doi pubmed - Unsgaard-Tondel M, Vasseljen O, Woodhouse A, Morkved S. Exercises for Women with Persistent Pelvic and Low Back Pain after Pregnancy. Glob J Health Sci. 2016;8(9):54311.
doi pubmed - Sakamoto A, Nakagawa H, Nakagawa H, Gamada K. Effects of exercises with a pelvic realignment device on low-back and pelvic girdle pain after childbirth: A randomized control study. J Rehabil Med. 2018;50(10):914-919.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
