| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 8, Number 2, June 2019, pages 54-56
Grey Platelet Syndrome and Pregnancy: A Case Report and Literature Review
Francisco Ibarguengoitia-Ochoaa, Cintia Maria Sepulveda-Riveraa, c, Sergio Emmanuel Santoyo-Rosasa, Diego Arturo Gonzalez-Vazqueza, Jessica Aidee Mora-Galvana, Samuel Vargas-Trujillob
aDepartment of Obstetrics, Instituto Nacional de Perinatologia, Calle Montes Urales 800, Lomas-Virreyes, Lomas de Chapultepec IV Secc, Mexico City 11000, Mexico
bDepartment of Hematology, Instituto Nacional de Perinatología, Calle Montes Urales 800, Lomas-Virreyes, Lomas de Chapultepec IV Secc, Mexico City 11000, Mexico
cCorresponding Author: Cintia Maria Sepulveda-Rivera, Instituto Nacional de Perinatologia, Calle Montes Urales 800, Lomas-Virreyes, Lomas de Chapultepec IV Secc, Mexico City 11000, Mexico
Manuscript submitted June 10, 2019, accepted June 19, 2019
Short title: Grey Platelet Syndrome and Pregnancy
doi: https://doi.org/10.14740/jcgo555
| Abstract | ▴Top |
Grey platelet syndrome is an uncommon hereditary platelet disorder, and is characterized by thrombocytopenia and platelet dysfunction with a specific absence of alpha-granules. Electronic microscopy is a quick test that can confirm the diagnosis. We present perinatal results of a patient with diagnosed grey platelet syndrome. We reviewed the case of a patient with grey platelet syndrome at Instituto Nacional de Perinatologia. She is 26 years old, with 21 weeks’ gestation. It is noted in initial laboratories a platelet amount of 64,000/mm3, and grey platelet syndrome is suspected, so peripheral blood smear is carried out which showed pale platelets, and electronic microscopy was performed to confirm the disorder, which showed the absence of platelet alpha-granules. A female newborn was delivered at 38.4 week of gestation by abdominal cesarean section, weighing 2,588 g, with platelet count at birth of 119,000/mm3. There is no general consensus of treatment in patients with grey platelet syndrome, and management must be multi-disciplinary between obstetrics, hematology and anesthesiology services.
Keywords: Pregnancy; Thrombocytopenia; Syndrome; Grey platelet
| Introduction | ▴Top |
Grey platelet syndrome is an uncommon hereditary platelet disorder first described in 1971 [1]. It is characterized by thrombocytopenia and platelet dysfunction with absence of alpha-granules, resulting in grey color platelets in a peripheral blood smear with Wright stain. Pregnancy thrombocytopenia is not unusual, present in 6-15% of pregnant women by the end of the pregnancy; the most common causes are pregnancy itself (74%), pre-eclampsia (21%) and immune thrombocytopenic purpura (4%) [2]. Clinically patients present ecchymosis and mucocutaneous bleeding generally after surgical procedures [3, 4]. Most cases are diagnosed in childhood or early adolescence by a history of bleeding events. Common laboratory values are thrombocytopenia and platelet abnormalities in a peripheral blood smear; electronic microscopy is a quick test that can confirm the diagnosis [5]. Actually, there are 100 published cases and only three of them present during pregnancy [5, 6].
| Case Report | ▴Top |
Clinical record of a patient with grey platelet syndrome during pregnancy was reviewed, who was treated at Instituto Nacional de Perinatologia.
A 26-year-old patient without important personal and family background was reviewed. She has a prior pregnancy in 2013 delivered vaginally at 40 weeks of gestation apparently without complications. At the interview we noted abnormal uterine bleeding with menstrual periods increased in volume and frequency. Patient started prenatal care at Instituto Nacional de Perinatologia at 21 weeks of gestation. Among initial laboratory values, platelet count was 64,000/mm3, and serial platelet counts varied between 55,000 and 64,000/mm3. Associated clinical data do not present like hypertension or proteinuria. Grey platelet syndrome is suspected so that peripheral blood smear was conducted, which showed pale platelets (Fig. 1); electronic microscopy study was performed to confirm the diagnosis, which showed absence of alpha-granules (Fig. 2). An infant was delivered by abdominal cesarean section at 38.4 weeks of gestation; prior surgery one unit platelet apheresis was transfused. A female newborn was obtained weighing 2,588 g, and platelet count at birth was 119,000/mm3.
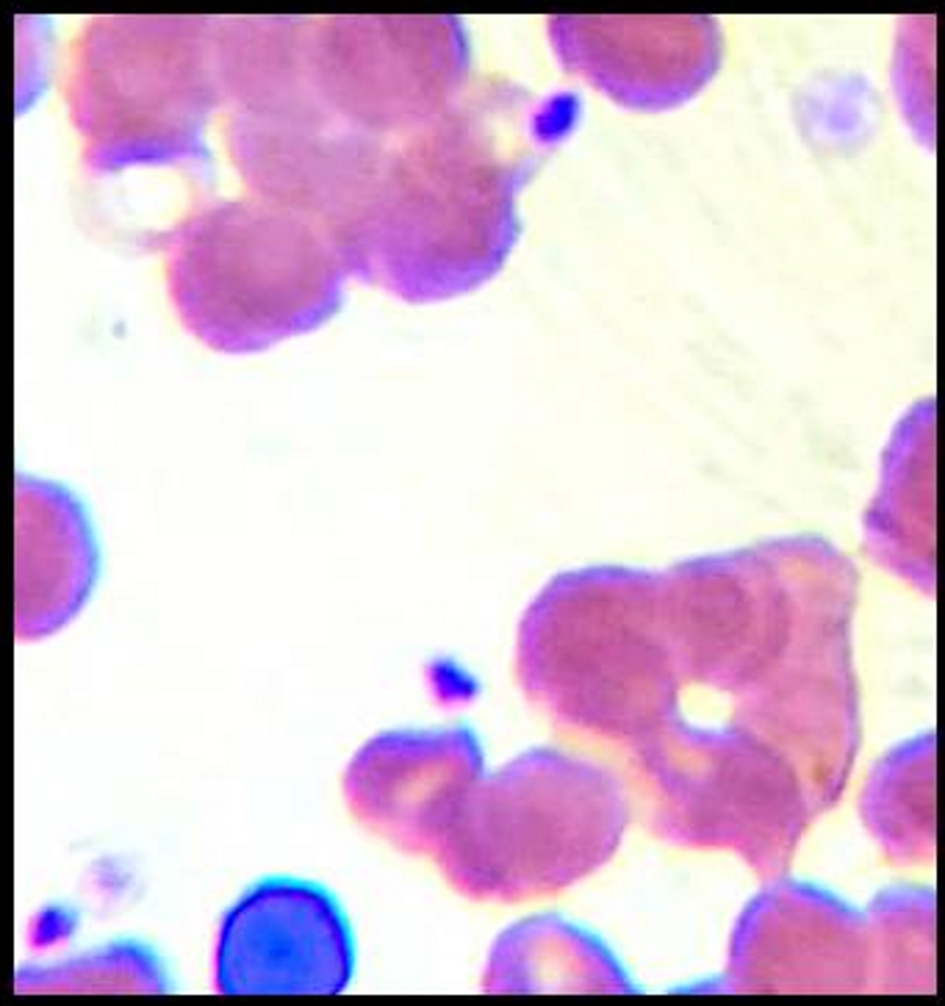 Click for large image | Figure 1. Pale platelets in peripheral blood smear. |
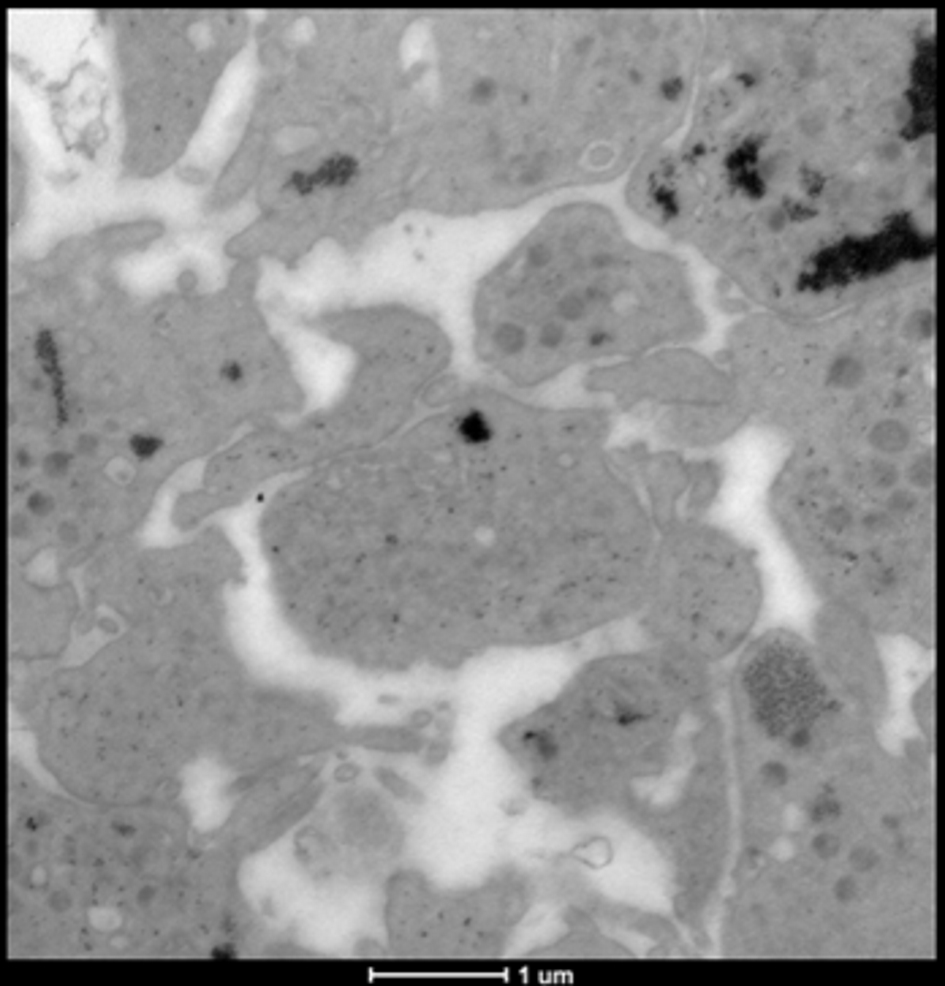 Click for large image | Figure 2. Electronic microscopy with absence of alpha-granules in platelets. |
| Discussion | ▴Top |
Grey platelet syndrome diagnosis is based on the absence of alpha-granules visible in an electron microscopy. A classic micrography shows virtually empty alpha-granules [7], such as the one realized in our patient. Alpha-granules contain abundant proteins including fibrinogen, VIII factor and V factor [8]. In most cases of grey platelet syndrome, there is a bleeding episode from moderate to severe, myelofibrosis and splenomegaly, like so rising levels of vitamin B12, clinical and biochemical features were not observed in our patient. Bleeding mechanism is not clearly elucidated, in the studied patient, and thrombocytopenia and abnormal uterine bleeding were observed. There is no general consensus about treatment, but opinions include desmopressin and platelet apheresis transfusion prior to surgical procedures, even when platelet count is above 10,000/mm3. Epidural and spinal anesthesia could not be recommended without demonstration of a normal bleeding time [5, 9], such as the one in the present case.
Conclusions
The incidence of congenital thrombocytopenia in pregnant women is unknown. Pregnancy course and delivery with congenital thrombocytopenia have not been described and there are no existent clear guides for management of these patients. The situation that is confronted is the risk of bleeding during pregnancy. Platelets must be prophylactically transfused to maximize hemorrhage control, using a one-donor-only platelet apheresis in order to reduce the alloimmunization risk. Close attention to any medication that can affect platelet function is suggested. Management must be multi-disciplinary between obstetrics, hematology and anesthesiology services.
Acknowledgments
We thank all the personnel at Instituto Nacional de Perinatologia.
Financial Disclosure
None.
Conflict of Interest
None.
Informed Consent
The signed informed consent from the patient was obtained.
Author Contributions
All the authors actively participated in the present work.
| References | ▴Top |
- Raccuglia G. Gray platelet syndrome. A variety of qualitative platelet disorder. Am J Med. 1971;51(6):818-828.
doi - Dolberg OJ, Ellis M. Successful pregnancy and delivery in a woman with gray platelet syndrome. Isr Med Assoc J. 2011;13(2):117-118.
- Levy-Toledano S, Caen JP, Breton-Gorius J, Rendu F, Cywiner-Golenzer C, Dupuy E, Legrand Y, et al. Gray platelet syndrome: alpha-granule deficiency. Its influence on platelet function. J Lab Clin Med. 1981;98(6):831-848.
- Nurden AT, Nurden P. The gray platelet syndrome: clinical spectrum of the disease. Blood Rev. 2007;21(1):21-36.
doi pubmed - Perez Botero J, Im R, Chen D, Patnaik MM. Grey platelet syndrome misdiagnosed as ITP. Br J Haematol. 2016;173(5):662.
doi pubmed - Laskey AL, Tobias JD. Anesthetic implications of the grey platelet syndrome. Can J Anaesth. 2000;47(12):1224-1229.
doi pubmed - Di Paola J, Johnson J. Thrombocytopenias due to gray platelet syndrome or THC2 mutations. Semin Thromb Hemost. 2011;37(6):690-697.
doi pubmed - Freson K, Wijgaerts A, van Geet C. Update on the causes of platelet disorders and functional consequences. Int J Lab Hematol. 2014;36(3):313-325.
doi pubmed - Balduini CL, Savoia A. Genetics of familial forms of thrombocytopenia. Hum Genet. 2012;131(12):1821-1832.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
