| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 9, Number 1-2, June 2020, pages 21-24
Primary Fallopian Tube Carcinoma Preoperatively Diagnosed as Cervical Cancer
Misa Kobayashia, b, Hiroshi Adachia
aDepartment of Gynecology, Seirei Hamamatsu General Hospital, 2-12-12 Sumiyoshi, Naka-ku, Hamamatsu, Shizuoka 430-8558, Japan
bCorresponding Author: Misa Kobayashi, Department of Gynecology, Seirei Hamamatsu General Hospital, 2-12-12 Sumiyoshi, Naka-ku, Hamamatsu, Shizuoka 430-8558, Japan
Manuscript submitted March 8, 2020, accepted May 12, 2020, published online June 5, 2020
Short title: PFTC Diagnosed as Cervical Cancer
doi: https://doi.org/10.14740/jcgo630
| Abstract | ▴Top |
Primary fallopian tube carcinoma (PFTC) is an uncommon gynecologic malignancy that is often diagnosed in the advanced stage. We present herein a case of a 59-year-old female with PFTC diagnosed with an approximately 20-mm cervical tumor on visual inspection. Cervical biopsy showed carcinoma and systemic computed tomography demonstrated no evidence of metastasis. The patient was accordingly diagnosed with cervical adenocarcinoma stage IB1 (FIGO 2008). Abdominal radical hysterectomy including bilateral salpingo-oophorectomy and pelvic lymphadenectomy was performed. However, it was difficult to operate because of dense pelvic organ adhesions and pouch of Douglas obliteration accompanied with deep infiltrating endometriosis. There was no peritoneal dissemination. On histopathological examination, high-grade serous carcinomas arising from the left fallopian tube and metastasized to the endometrium, cervix, vagina and multiple pelvic lymph nodes and forming a tumor in the cervix were noted. The patient was diagnosed with PFTC stage IIIA1 (ii) (FIGO 2014), pT2aN1bM0 (eighth UICC). She received six cycles of docetaxel and carboplatin every 3 weeks and presented no evidence of disease for 6 months after the chemotherapy. In conclusion, this is a rare case in which PFTC was preoperatively diagnosed as cervical cancer.
Keywords: Primary fallopian tube carcinoma; Diagnosis; Cervical cancer
| Introduction | ▴Top |
Primary fallopian tube carcinoma (PFTC) is rare, accounting for only approximately 1% of all gynecologic malignancies [1]. Almost all PFTCs originate from the ampulla, and direct peritoneal implantation, lymphatic spread, and early metastases are common. Preoperative diagnosis of PFTC is challenging. We present herein a case of PFTC that was diagnosed preoperatively as cervical cancer with no evidence of metastasis.
| Case Report | ▴Top |
A 59-year-old postmenopausal woman (gravida: 3, para: 3) was diagnosed with one 20-mm cervical tumor on medical examination. She had no gynecologic complaints such as vaginal bleeding, pelvic pain, or vaginal discharge, and also had no positive history of malignancy. However, her mother had a history of breast cancer and her younger sister died due to primary peritoneal cancer.
Cervical biopsy showed carcinoma. Pelvic magnetic resonance imaging (MRI) demonstrated a 24-mm cervical mass without parametrial invasion. It had high signal intensity on T2-weighted images (T2WI), and high signal intensity on diffusion-weighted imaging (DWI) and showed moderate enhancement. Furthermore, it also demonstrated hematometra and left hematosalpinx with high signal intensity on T1-weighted imaging and T2W1 (Fig. 1). Systemic computed tomography demonstrated no evidence of metastasis. No tumor marker level was elevated (cancer antigen (CA)-125: 24.4 U/mL; CA-19-9 < 2.0 U/mL; carcinoembryonic antigen 1.4 U/mL; squamous cell carcinoma antigen 0.8 ng/mL).
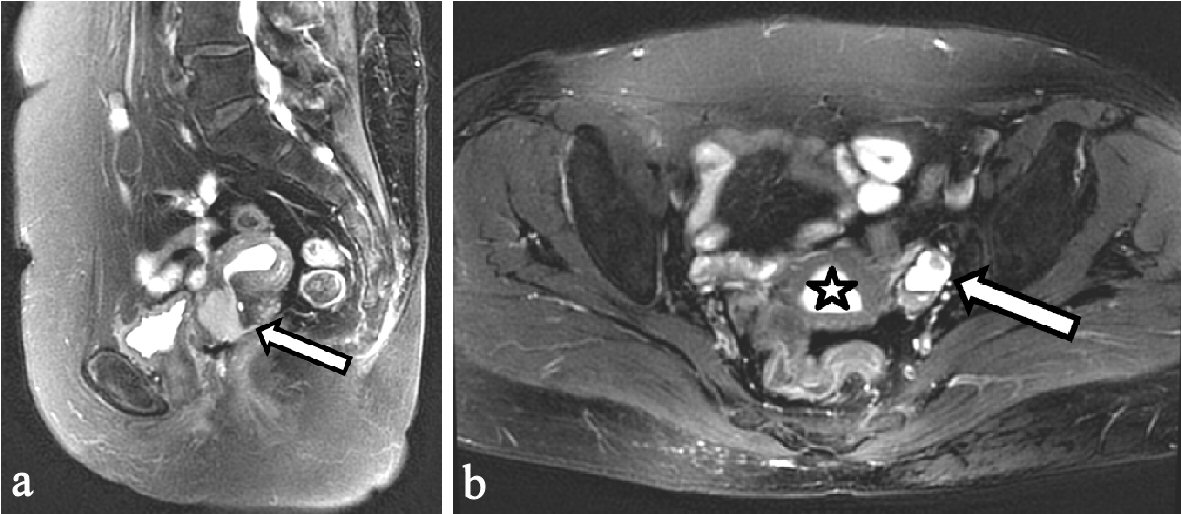 Click for large image | Figure 1. Preoperative pelvic MRI. (a) Sagittal T2-weighted imaging. A 24-mm cervical tumor showing high-intensity signal (arrow). (b) Axial T2-weighted imaging, hematometra (asterisk) and left hematosalpinx with mural nodule (arrow) showing high-intensity signal. MRI: magnetic resonance imaging. |
She was diagnosed with cervical cancer, cT1b1N0M0 (eighth UICC), stage IB1 (FIGO 2008). Abdominal radical hysterectomy including bilateral salpingo-oophorectomy and pelvic lymphadenectomy was performed (Fig. 2). It was difficult to operate because of dense pelvic organ adhesions, and the pouch of Douglas obliteration was accompanied with deeply infiltrating endometriosis. There was no peritoneal dissemination. Left common iliac nodes and left obturator nodes were swollen to approximately 2 cm.
 Click for large image | Figure 2. Surgical specimen showing a 35-mm cervical tumor (arrow) and left hematosalpinx (asterisk). |
On histopathological examination, high-grade serous carcinomas arising from the left fallopian tube and metastasized to the endometrium, cervix, vagina and multiple pelvic lymph nodes (bilateral common iliac nodes, left obturator nodes, and right external iliac nodes) and forming a tumor in the cervix were noted (Fig. 3). She was postoperatively diagnosed with PFTC, pT2aN1bM0 (eighth UICC), stage IIIA1 (ii) (FIGO 2014). She received six cycles of chemotherapy with docetaxel and carboplatin every 3 weeks and presented no evidence of disease for 15 months after chemotherapy.
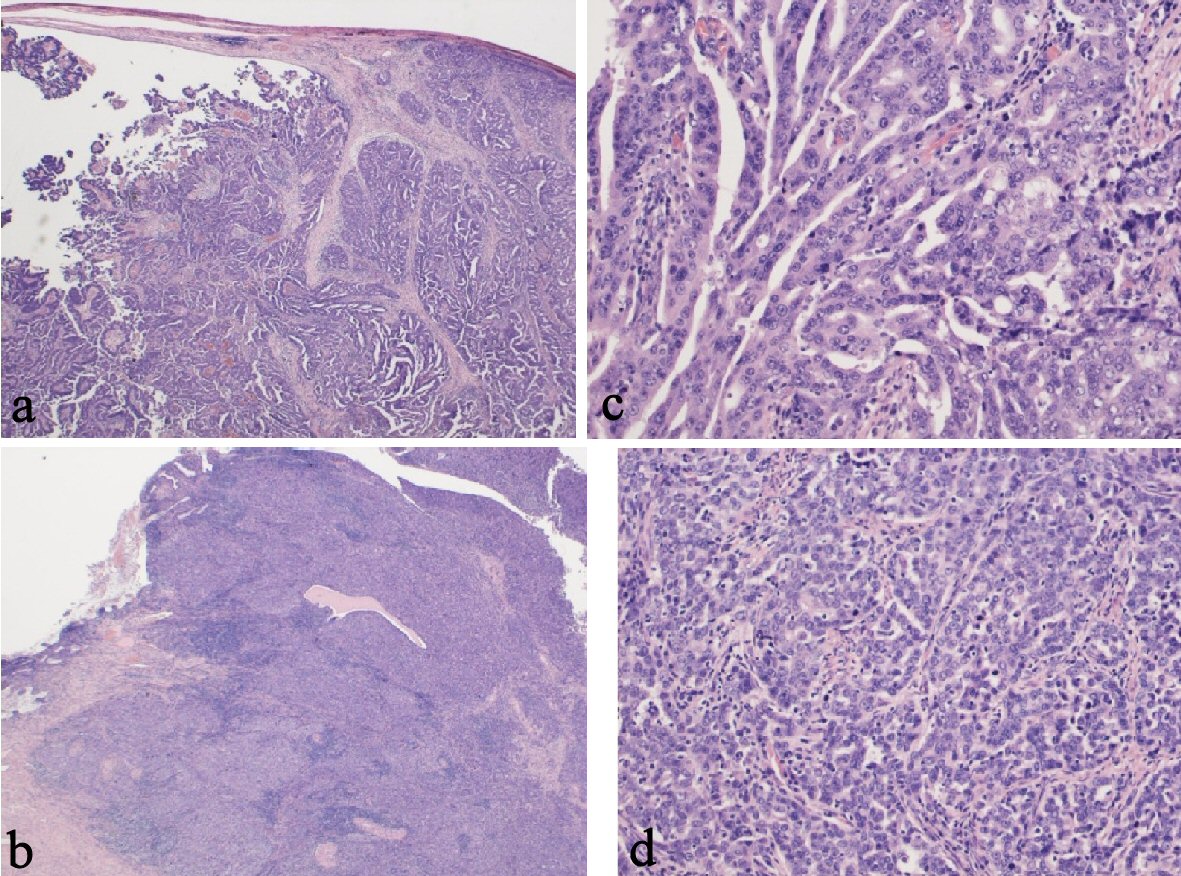 Click for large image | Figure 3. Pathological findings. (a) Left fallopian tube, carcinoma with infiltration into the tubal wall (H&E staining, × 15). (b) Left fallopian tube, papillary serous adenocarcinoma (H&E staining, × 150). (c) Cervix, carcinoma and remaining cervical glands (H&E staining, × 15). (d) Cervix, serous adenocarcinoma similar to a fallopian tube carcinoma (H&E staining, × 150). H&E: hematoxylin and eosin stain. |
| Discussion | ▴Top |
This is a rare case in which PFTC was preoperatively diagnosed as cervical cancer. PFTCs are rare, and are often detected in the advanced stage because of direct peritoneal implantation, lymphatic spread and early metastases. Approximately 45-65% of cases are diagnosed at stage III/IV [2]. The fallopian tube is richly supplied with lymphatic networks that drain into the pelvic and paraaortic lymph nodes, and pelvic and/or paraaortic lymph nodes involvements occurs in approximately 40% of all cancer stages [3]. Meanwhile, approximately 80% of tubal carcinomas are metastatic from ovarian, endometrial, and gastrointestinal cancers [4]. PFTC is difficult to diagnose, and only 4% are diagnosed correctly preoperatively [5].
Certain symptoms and serum CA-125 level may be helpful in diagnosis. The Latzko’s triad of symptoms, which includes profuse serosanguinous vaginal bleeding, abdominal or pelvic mass and colicky pain relieved by discharge is pathognomonic. However, there are no characteristic symptoms of PFTCs, and the Latzko’s triad was reported in only 15% of cases [5]. In the current case, the patient had no gynecologic complaints. Preoperative serum CA-125 level had been reported to increase beyond 35 U/mL in 75-85% of cases, and it increased in 33%, 50%, 89%, and 100% of patients with stage I, II, III, and IV disease, respectively [2, 3]. However, our patient has stage III disease, but the serum CA-125 level was not elevated (24.4 U/mL).
Atypical glandular cells and adenocarcinoma cells in Pap smear indicate the possibility of fallopian tube carcinomas [6]. In total, 88% of PFTCs are adenocarcinomas [7]. Almost all PFTCs originate from the ampulla, and spread primarily through the tubal fimbria and into the peritoneal cavity. Some sloughed tumor cells are transported to the uterine cavity through ciliary movement and fallopian tube peristalsis. These cells are then trapped in cervical mucus. A total of 5.2% of atypical glandular cells that test positive on Pap smear are malignant, and 6.4% of them are ovarian or fallopian tube carcinomas [8]. Positive Pap smear results are observed in 10-36% of PFTCs [5]. In our case, the patient was diagnosed of cervical cancer because of prominent tumor formation in the cervix and detection of carcinoma from cervical tumor. This is a similar case of PFTC with skip metastasis in the cervix, which was preoperatively diagnosed as cervical cancer [9].
Some characteristic MRI findings may also provide a diagnostic clue preoperatively [10]. A sausage-shaped mass is one of the most specific MRI findings seen in PFTC, which occurs when fallopian tubes are filled with a solid tumor. Hydrosalpinx occurs in PFTC because of the copious amounts of fluid produced by the tumor and the partial obstruction of the tubes. The dilated tubes contain incomplete folds and show a convoluted appearance, known as the “waist sign”. Extremely dilated tube folds upon itself, forming the “cogwheel sign”. Fallopian tube dilations can lead to fluid discharge into the intrauterine cavity. Hydrometra is specific to PFTC and can occur in up to 30% of cases. In our case, hematosalpinx with a mural nodule and hematometra were noted, and we believe that this was caused by the severe adhesions due to the endometriosis and the cervical mass, and these presentations were consistent with cervical cancer.
Although our case showed negative clinical and biochemical findings, assessing histopathological and radiological parameters could be valuable in the diagnosis of PFTC. Further, the family history indicated as possibility of hereditary cancer. The etiology of PFTC remains unclear. Some factors such as infertility, chronic tubal inflammation, endometriosis, nulliparity, smoking, and genetic predisposition have been reported to increase the risk of PFTC [11]. Because the fallopian tube and the peritoneum are embryologically derived from Mullerian structures, their neoplastic behavior is similar to that of ovarian cancer. Her younger sister’s history of primary peritoneal cancer even meets the BRCA testing criteria [12]. Women who have BRCA1 or BRCA2 gene mutation have higher risks of breast and ovarian cancer, and should undergo genetic counseling regardless of the onset of PFTC. The preoperative diagnosis might have been correct if we considered her family history.
In conclusion, PFTCs are extremely difficult to diagnose preoperatively. This is a rare case in which PFTC was preoperatively diagnosed as cervical cancer.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Informed Consent
The patient provided informed consent to publish the case.
Author Contributions
Misa Kobayashi contributed to diagnosis, treatment and follow-up of this case, literature research and article writing. Hiroshi Adachi contributed to revising the article.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Maeda D, Takazawa Y, Ota S, Takeuchi Y, Seta A, Nakagawa S, Yano T, et al. Bilateral microscopic adenocarcinoma of the fallopian tubes detected by an endometrial cytologic smear. Int J Gynecol Pathol. 2010;29(3):273-277.
doi pubmed - Lau HY, Chen YJ, Yen MS, Chen RF, Yeh SO, Twu NF. Primary fallopian tube carcinoma: a clinicopathologic analysis and literature review. J Chin Med Assoc. 2013;76(10):583-587.
doi pubmed - Gadducci A, Landoni F, Sartori E, Maggino T, Zola P, Gabriele A, Rossi R, et al. Analysis of treatment failures and survival of patients with fallopian tube carcinoma: a cooperation task force (CTF) study. Gynecol Oncol. 2001;81(2):150-159.
doi pubmed - Pardeshi SP, Kulkarni MM, Hishikar VA. Primary fallopian tube carcinoma. J Postgrad Med. 1996;42(2):59-61.
- Ajithkumar TV, Minimole AL, John MM, Ashokkumar OS. Primary fallopian tube carcinoma. Obstet Gynecol Surv. 2005;60(4):247-252.
doi pubmed - Mulvany NJ, Mitchell G, Allen DG. Adenocarcinoma cells in Pap smears. Pathology. 2009;41(5):411-418.
doi pubmed - Stewart SL, Wike JM, Foster SL, Michaud F. The incidence of primary fallopian tube cancer in the United States. Gynecol Oncol. 2007;107(3):392-397.
doi pubmed - Schnatz PF, Guile M, O'Sullivan DM, Sorosky JI. Clinical significance of atypical glandular cells on cervical cytology. Obstet Gynecol. 2006;107(3):701-708.
doi pubmed - Ali SS, Saeed O, Muzaffar S, Riaz T, Setna F, Ayub S. Fallopian tube carcinoma presenting as cervical growth: the dilemma of skip metastasis. Aust N Z J Obstet Gynaecol. 2003;43(1):82-84.
doi pubmed - Veloso Gomes F, Dias JL, Lucas R, Cunha TM. Primary fallopian tube carcinoma: review of MR imaging findings. Insights Imaging. 2015;6(4):431-439.
doi pubmed - Alvarado-Cabrero I, Young RH, Vamvakas EC, Scully RE. Carcinoma of the fallopian tube: a clinicopathological study of 105 cases with observations on staging and prognostic factors. Gynecol Oncol. 1999;72(3):367-379.
doi pubmed - NCCN guidelines version 1. 2018 genetic/familial high-risk assessment: breast and oarian.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
