| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Case Report
Volume 9, Number 4, December 2020, pages 108-111
Left Diaphragmatic Hernia After Diaphragmatic Peritonectomy for Peritoneal Cancer
Hitomi Sakaguchia, b, Kumi Masudaa, Mariya Kobayashia, Yukako Oia, Akiko Fujishiroa, Asuka Tanakaa, Katsumi Kozasaa, Hirokazu Naoia, Hirofumi Otsukaa, Takeshi Yokoia
aDepartment of Obstetrics and Gynecology, Kaizuka City Hospital, Osaka, Japan
bCorresponding Author: Hitomi Sakaguchi, Department of Obstetrics and Gynecology, Kaizuka City Hospital, 3-10-20 Hori, Kaizuka-shi, Osaka 597-0015, Japan
Manuscript submitted September 13, 2020, accepted October 28, 2020, published online December 15, 2020
Short title: Left Diaphragmatic Hernia
doi: https://doi.org/10.14740/jcgo693
| Abstract | ▴Top |
Peritoneal cancer is often treated as advanced ovarian adenocarcinoma, with cytoreduction as the surgical procedure. For peritoneal cancer with extensive peritoneal spread, peritonectomy including diaphragmatic peritonectomy is often performed for optimal surgery. The most common complications are pleural effusion, pneumothorax, and endoabdominal collections. However, diaphragmatic hernia is a rare complication. We report here, a case of left diaphragmatic hernia, a rare complication that occurred nine months post-surgery that included diaphragmatic peritonectomy after neoadjuvant chemotherapy for peritoneal cancer.
Keywords: Diaphragmatic hernia; Diaphragmatic peritonectomy; Peritoneal cancer
| Introduction | ▴Top |
Peritoneal cancer is often treated histologically as advanced ovarian adenocarcinoma [1-3] and the major clinical feature is that majority of peritoneal cancer cases are in stage III - IV (International Federation of Gynecology and Obstetrics (FIGO) 2014) [4]. Peritoneal spread is a common feature in patients with advanced or recurrent ovarian cancer or peritoneal cancer. The recommended surgical procedure is extensive standard cytoreduction. Since the first report by Griffith et al [5], multiple retrospective series have shown that survival is inversely proportional to residual lesions. A meta-analysis showed that maximal cytoreduction improves prognosis and the maximum residual tumor diameter should be ideally reduced to the microscopic level.
Many reports also show that a diameter of residual disease that is less than 1 cm has a significantly better prognosis than that of 1 cm or more. Furthermore, the prognosis would be extremely good when the residual disease is reduced to the microscopic level [6-10].
With the goal of better cytoreduction and improved prognosis, extensive upper abdominal surgical procedure, such as omentectomy, splenectomy, distal pancreatectomy, diaphragmatic peritonectomy, and peritonectomy for pelvic and peritoneal lesions are recommended [7-11]. While the optimal surgery extent is thus increased, the operation then becomes quite invasive, with a concomitant increase in risk of perioperative complications such as prolonged operation time, increased blood loss, and pleural effusion. Specific complications associated with diaphragmatic peritonectomy include pleural and pulmonary complications (pleural effusion, pneumothorax, lung infection, chest drainage, etc. [10-12]. However, there are fewer complications compared with upper abdominal surgery associated with diaphragmatic peritonectomy such as splenectomy or distal pancreatectomy leading to pancreatitis, digestive fistulas or abdominal collections [13-15]. Here, we report a diaphragmatic hernia with gastric volvulus nine months after surgery in advanced peritoneal cancer.
| Case Report | ▴Top |
A 47-year-old woman complained of abdominal fullness, malaise, and anorexia. The patient’s weight was 49 kg (body mass index (BMI) 19.1 kg/m2) and she wasn’t obesity. She had no medical history. Abdominal computed tomography showed a pelvic mass, ascites, peritoneal spread, bilateral internal iliac lymph nodes and para-aortic lymph nodes enlargement. Dyspnea due to accumulation of pleural fluid and ascites was observed, and cell-free and concentrated ascites reinfusion therapy was performed. Adenocarcinoma was detected from ascites and pleural effusion, and the peritoneal cancer was diagnosed as clinical progression classification cT3cN1M1a FIGO stage IVa (FIGO 2014).
Neoadjuvant chemotherapy was administered with four cycles of Taxol (175 mg/m2) and carboplatin (area under the curve (AUC) 5) and bevacizumab (15 mg/kg). Radiological studies showed decrease of peritoneal cancer and ascites after chemotherapy, which was classified as partial response (PR) under the response evaluation criteria in solid tumors (RECIST) classification. The patient received a debulking surgery, comprising total hysterectomy, bilateral adnexectomy, right hemicolectomy, low anterior resection, and peritonectomy including diaphragmatic peritonectomy as extensive peritoneal spread was found. Pathological staging classified the tumor as ypT3cN1Ma FIGO stage IVa. Thereafter, pan-peritonitis due to rectal anastomotic leakage was observed 7 days after the operation, and relaparotomy was required. Abdominal irrigation and colostomy were performed. Antibiotic treatment and several abscess drainages were subsequently required. On the 34th day after the first surgery, the patient became afebrile with no signs of persistent infection and her weight was 43.5 kg (BMI 17.0 kg/m2). She was discharged on the 41st day.
Thereafter, adjuvant chemotherapy was administered with only one cycle of a Taxol (175 mg/m2) and carboplatin (AUC5) because alcohol hypersensitivity to Taxol was observed, and subsequently four cycles of chemotherapy with doxorubicin (30 mg/m2) and carboplatin (AUC5) was given.
However, about 2 weeks after the final hospitalization, she was re-admitted to the hospital due to abdominal pain and vomiting. Abdominal X-rays did not show any apparent intestinal obstruction and fasting infusion management was given. As her symptoms improved from the third day after hospitalization, she resumed an oral diet, but she vomited and complained of abdominal pain after 2 days. Abdominal computed tomography was then carried out.
Computed tomography examination revealed that the left diaphragm was raised in the thorax and the stomach was straying into the thorax (Fig.1). Neutrophils had decreased to 300/µL due to bone marrow suppression as side effects of the final chemotherapy. Therefore, emergency operation was considered dangerous. On the same day, an upper endoscopy was attempted to the left diaphragmatic hernia with gastric volvulus to restore the stomach to the abdominal cavity, but this was difficult.
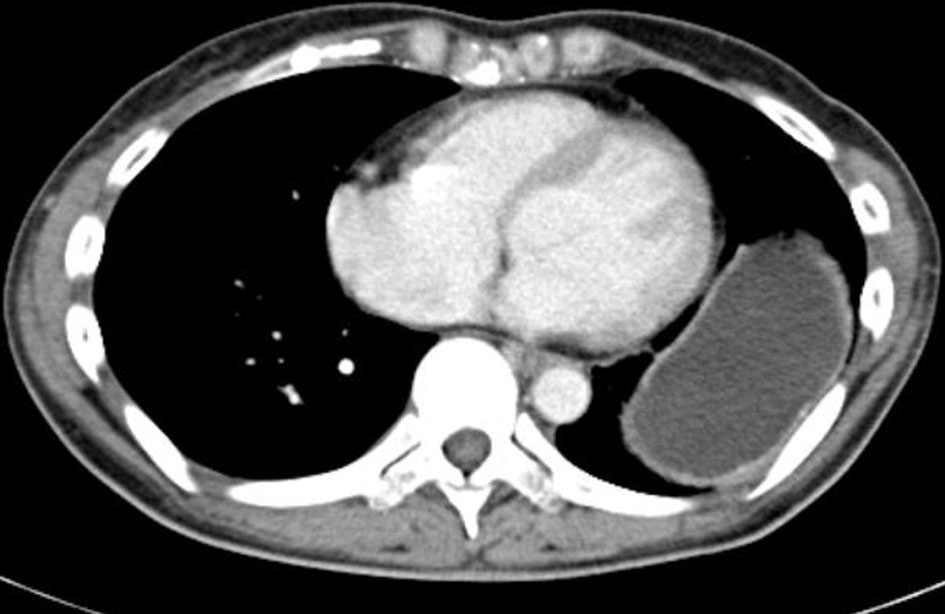 Click for large image | Figure 1. CT scan showing the stomach and left diaphragm raised in the thorax. CT: computed tomography. |
A gastric tube was inserted, and fasting infusion was extended until recovery from bone marrow suppression. Finally, the operation was performed 15 days from hospitalization. During the operation, left diaphragmatic hernia with gastric volvulus into the thorax was observed, but there was no cancer recurrence. The stomach was restored to the abdominal cavity and we could observe the left lung through the diaphragm (Fig. 2). The diaphragmatic hiatus hernia was repaired directly with non-absorbent suture (Fig. 3). At the same time, closure of colostomy was performed. Recurrence were not observed from the ascites collected during the operation. After the operation, she recovered well and was discharged from the hospital in about 2 weeks.
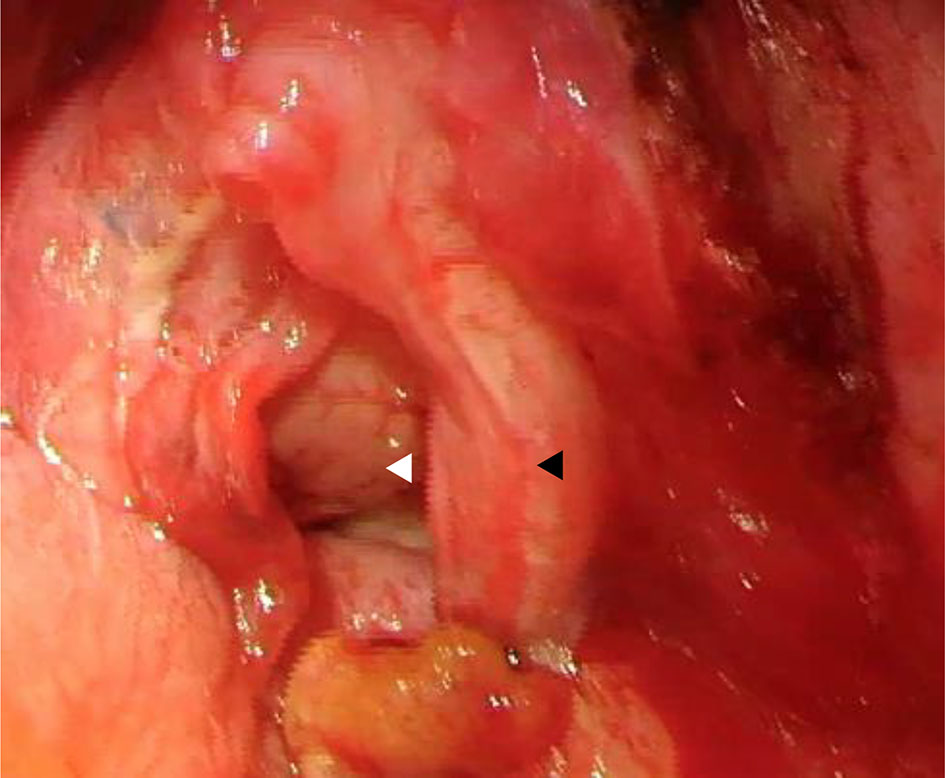 Click for large image | Figure 2. Left lung (white arrowhead) was observed through left diaphragm (black arrowhead). |
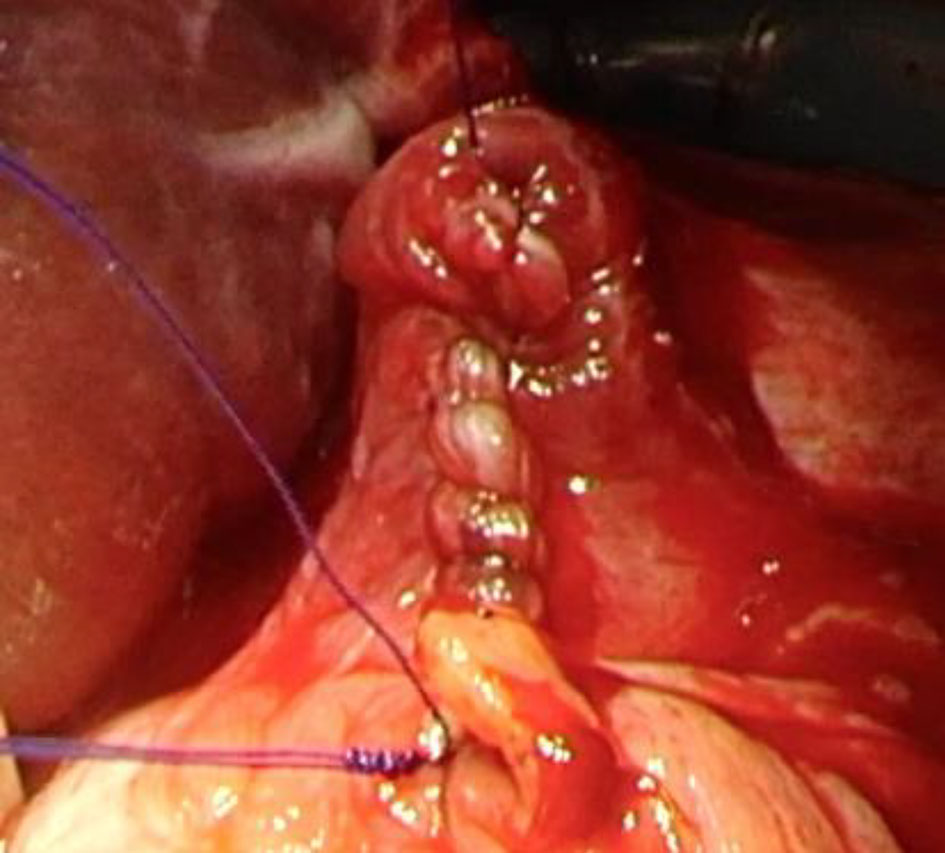 Click for large image | Figure 3. The diaphragmatic hiatus hernia was repaired directly with non-absorbent suture. |
| Discussion | ▴Top |
For advanced ovarian cancer and peritoneal cancer, delayed diaphragmatic hernia is rare as a postoperative complication in an extensive upper abdominal surgical procedure for cytoreduction and few cases have been reported. Furthermore, there have been three similar cases of left diaphragmatic hernia in the literature. Right diaphragmatic hernia is rare because of the liver and diaphragmatic hernia is believed to occur on the left side [16, 17].
In the report by Lampl et al [17], after cytoreduction including diaphragmatic peritonectomy, diaphragmatic hernia subsequently developed while other complications were not reported. The cause of diaphragmatic hernia is often related to cytoreduction including diaphragmatic peritonectomy and intraperitoneal hyperthermia (HIPEC) [18]. There have been few reports on an increased risk of diaphragmatic hernia due to intravenous adjuvant chemotherapy alone [19]. Increased abdominal pressure in conditions such as obesity may result in the development of a diaphragmatic hernia.
In this present case, obesity was not observed. However, multiple causes led to abdominal pressure increase may be considered. First, adjuvant chemotherapy was performed for several months and her condition was generally good during and after chemotherapy. The patient’s gastrointestinal symptom, such as nausea and vomiting, was controlled very well with antiemetics, and these symptoms were therefore classified as grade 1 or lower under the Common Terminology Criteria for Adverse Events (CTCAE) classification. The patient's increase in weight from additional food intake could have led to abdominal pressure increase. Consequently, abdominal pressure increase was not caused by adjuvant chemotherapy alone.
Furthermore, during diaphragmatic peritonectomy in the first surgery, the diaphragm had been damaged and the left lung could be seen through a hiatus hernia. While the hiatus hernia was repaired with 3-0 Prolene suture during the operation, the possibility remains that the diaphragm was fragile. In addition, as adjuvant chemotherapy was performed, this could have led to poor healing of the diaphragm, resulting in vulnerability of the diaphragm to increased abdominal pressure. Diaphragmatic hernia should be recognized as a possible complication which may arise during and after chemotherapy in patients who have undergone diaphragmatic peritonectomy. In our opinion, there is no revolutionary method for preventing diaphragmatic hernia, which is a late postoperative complication, but if there are similar symptoms in similar cases, strategies for earlier detection are needed.
We report here, a case of delayed left diaphragmatic hernia after surgery that included diaphragmatic peritonectomy after neoadjuvant chemotherapy for peritoneal cancer. It is a complication that is difficult to predict, however, knowledge of its symptoms such as abdominal pain or vomiting can aid in early detection of this rare complication.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Author Contributions
HS, KM, MK, YO, and TY contributed to diagnosis, treatment and follow-up of this case. HS wrote the first draft. KM contributed to revising the article. All authors read and approved the final manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Piura B, Meirovitz M, Bartfeld M, Yanai-Inbar I, Cohen Y. Peritoneal papillary serous carcinoma: study of 15 cases and comparison with stage III-IV ovarian papillary serous carcinoma. J Surg Oncol. 1998;68(3):173-178.
doi - Bloss JD, Brady MF, Liao SY, Rocereto T, Partridge EE, Clarke-Pearson DL, Gynecologic Oncology Group S. Extraovarian peritoneal serous papillary carcinoma: a phase II trial of cisplatin and cyclophosphamide with comparison to a cohort with papillary serous ovarian carcinoma-a Gynecologic Oncology Group Study. Gynecol Oncol. 2003;89(1):148-154.
doi - Jaaback KS, Ludeman L, Clayton NL, Hirschowitz L. Primary peritoneal carcinoma in a UK cancer center: comparison with advanced ovarian carcinoma over a 5-year period. Int J Gynecol Cancer. 2006;16(Suppl 1):123-128.
doi pubmed - Halperin R, Zehavi S, Langer R, Hadas E, Bukovsky I, Schneider D. Primary peritoneal serous papillary carcinoma: a new epidemiologic trend? A matched-case comparison with ovarian serous papillary cancer. Int J Gynecol Cancer. 2001;11(5):403-408.
doi pubmed - Griffiths CT. Surgical resection of tumor bulk in the primary treatment of ovarian carcinoma. Natl Cancer Inst Monogr. 1975;42:101-104.
- Eisenhauer EL, Sonoda Y, Levine DA, Abu-Rustum NR, Gemignani ML, Sabbatini PJ, Barakat RR, et al. Platinum resistance and impaired survival in patients with advanced primary peritoneal carcinoma: matched-case comparison with patients with epithelial ovarian carcinoma. Am J Obstet Gynecol. 2008;198(2):213 e211-217.
doi pubmed - Chi DS, Franklin CC, Levine DA, Akselrod F, Sabbatini P, Jarnagin WR, DeMatteo R, et al. Improved optimal cytoreduction rates for stages IIIC and IV epithelial ovarian, fallopian tube, and primary peritoneal cancer: a change in surgical approach. Gynecol Oncol. 2004;94(3):650-654.
doi pubmed - Zivanovic O, Eisenhauer EL, Zhou Q, Iasonos A, Sabbatini P, Sonoda Y, Abu-Rustum NR, et al. The impact of bulky upper abdominal disease cephalad to the greater omentum on surgical outcome for stage IIIC epithelial ovarian, fallopian tube, and primary peritoneal cancer. Gynecol Oncol. 2008;108(2):287-292.
doi pubmed - Chi DS, Eisenhauer EL, Zivanovic O, Sonoda Y, Abu-Rustum NR, Levine DA, et al. Improved progression-free and overall survival in advanced ovarian cancer as a result of a change in surgical paradigm. Gynecol Oncol 2006; 103:871-877.
- Eisenhauer EL, D'Angelica MI, Abu-Rustum NR, Sonoda Y, Jarnagin WR, Barakat RR, Chi DS. Incidence and management of pleural effusions after diaphragm peritonectomy or resection for advanced mullerian cancer. Gynecol Oncol. 2006;103(3):871-877.
doi pubmed - Aletti GD, Powless C, Bakkum-Gamez J, Wilson TO, Podratz KC, Cliby WA. Pattern of retroperitoneal dissemination of primary peritoneum cancer: basis for rational use of lymphadenectomy. Gynecol Oncol. 2009;114(1):32-36.
doi pubmed - Kehoe SM, Eisenhauer EL, Abu-Rustum NR, Sonoda Y, D'Angelica M, Jarnagin WR, Barakat RR, et al. Incidence and management of pancreatic leaks after splenectomy with distal pancreatectomy performed during primary cytoreductive surgery for advanced ovarian, peritoneal and fallopian tube cancer. Gynecol Oncol. 2009;112(3):496-500.
doi pubmed - Chereau E, Rouzier R, Gouy S, Ferron G, Narducci F, Bergzoll C, Huchon C, et al. Morbidity of diaphragmatic surgery for advanced ovarian cancer: retrospective study of 148 cases. Eur J Surg Oncol. 2011;37(2):175-180.
doi pubmed - Chi DS, Zivanovic O, Levinson KL, Kolev V, Huh J, Dottino J, Gardner GJ, et al. The incidence of major complications after the performance of extensive upper abdominal surgical procedures during primary cytoreduction of advanced ovarian, tubal, and peritoneal carcinomas. Gynecol Oncol. 2010;119(1):38-42.
doi pubmed - Terauchi F, Okamoto A, Wada Y, Hasegawa E, Sasaki T, Akutagawa O, Sagawa Y, et al. Incidental events of diaphragmatic surgery in 82 patients with advanced ovarian, primary peritoneal and fallopian tubal cancer. Oncol Lett. 2010;1(5):861-864.
doi pubmed - Laterza B, Baratti D, Cozzi G, Kusamura S, Oliva GD, Gavazzi C, Fumagalli L, et al. Colobronchial fistula: an unusual complication after peritonectomy and hyperthermic intra-peritoneal chemotherapy (HIPEC). In Vivo. 2009;23(1):151-153.
- Lampl B, Leebmann H, Mayr M, Piso P. Rare diaphragmatic complications following cytoreductive surgery and HIPEC: report of two cases. Surg Today. 2014;44(2):383-386.
doi pubmed - Caronna R, Sammartino P, Framarino ML, Sollazzo BM, Meniconi RL, Chirletti P. Intrathoracic gastric volvulus as a severe, delayed surgical complication after left subphrenic peritonectomy and hyperthermic intraperitoneal chemotherapy (HIPEC) for advanced ovarian cancer. World J Surg Oncol. 2013;11:239.
doi pubmed - Sun Y, Yin L, Xue H, Wang H, Li Z, Yu J. Unusual delayed presentation of diaphragmatic hernia complicated by transverse colon and total small-bowel obstruction after postoperative chemotherapy of esophageal cancer. Ther Clin Risk Manag. 2017;13:691-695.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
