| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Original Article
Volume 10, Number 1, March 2021, pages 11-17
Prospective Study of Fractional Carbon Dioxide Laser Therapy for Symptoms of Genitourinary Syndrome of Menopause: One-Year Follow-Up
Jeffrey S. Schachara, Hemikaa Devakumara, Laura Martina, Eric A. Hurtadoa, G. Willy Davilab, c
aDepartment of Gynecology, Section of Female Pelvic Medicine and Reconstructive Surgery, Cleveland Clinic Florida, Weston, FL, USA
bHoly Cross Medical Group, Fort Lauderdale, FL, USA
cCorresponding Author: G. Willy Davila, Dorothy Mangurian Comprehensive Women’s Center, Holy Cross Medical Group, 1000 NE 56th St., Fort Lauderdale, FL 33334, USA
Manuscript submitted February 21, 2021, accepted March 10, 2021, published online March 17, 2021
Short title: CO2 Laser Therapy for Symptoms of Menopause
doi: https://doi.org/10.14740/jcgo729
| Abstract | ▴Top |
Background: Our objective is to prospectively evaluate pixelated carbon dioxide (CO2) laser therapy for the treatment of symptomatic genitourinary syndrome of menopause (GSM) over 1 year using both subjective and objective assessment methods.
Methods: Subjects with symptomatic GSM completed pre-treatment evaluations. Subjects underwent three standardized pixelated CO2 laser treatments 4 weeks apart. Use of other treatments during the study period was prohibited. Subjects completed five subjective GSM questionnaires (visual analog grading scale for vaginal atrophy symptoms (VAS-VA), Symptoms of Atrophic Vaginitis Questionnaire (SAVQ), and a modified Vulvovaginal Symptom Questionnaire (mVSQ), Urinary Distress Inventory (UDI-6) and the Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire (PISQ-12)) and physical assessments (Bachmann Vaginal Health Index (BVHI) and Vaginal Health Assessment (VHA)) 2 weeks after each treatment, and at 1 year. Vaginal cytologic maturation assessment was performed before and after each treatment. Three random subjects also underwent vaginal biopsy after treatments were completed. A P value of less than 0.05 was considered statistically significant.
Results: Fifteen subjects were recruited with an average age of 58.3 years (range 43 - 70). Subjects had significant improvements on four of the five subjective assessments of GSM and on the two objective indices, from baseline to shortly after the third treatment, and were maintained at 1-year follow-up, with no worsening of the improvements. Subjects did not have significant improvement in urinary symptoms. Histologically, the surface epithelium ranged from within normal limits to mild squamous atrophy. There was mild submucosal vascular congestion in all specimens, with evident neovascularization.
Conclusions: Clinically significant improvement was noted in subjective and objective assessments of GSM, and was sustained for 1 year following pixelated CO2 laser therapy. Histologic changes were consistent with mild submucosal neovascularization rather than estrogen-like epithelial squamous maturation.
Keywords: CO2 laser; Genitourinary syndrome of menopause; Mechanism of action; Vulvovaginal atrophy
| Introduction | ▴Top |
As life expectancy continues to increase, women will spend more time in menopause. Genitourinary syndrome of menopause (GSM) is a constellation of symptoms that result from vulvovaginal atrophic changes that occur following the decline in circulating estrogen levels after menopause [1, 2]. These symptoms include vulvovaginal burning, decreased lubrication, dyspareunia and urinary symptoms, such as dysuria, frequency, or recurrent urinary tract infections. Fifty percent of women are affected by GSM, which can negatively impact their quality of life, yet only 7% of women request treatment of their symptoms [2-5].
There are a wide range of treatment options for GSM. Options include non-hormonal lubricants and moisturizers which may alleviate some of the mild symptoms. Selective estrogen receptor modulators, such as ospemifene, are well tolerated and are somewhat effective in decreasing the symptoms related to hypoestrogenism. Steroids, such as prasterone, have also been shown to be effective for treatment of vulvovaginal atrophy. The gold standard treatment has been local estrogen therapy, which has been shown to be superior to systemic therapy for vulvovaginal atrophy. However, local estrogen has poor compliance due to weekly self-applications and increased vaginal discharge. In addition, there has been controversy over the use of estrogen for women with hormone-dependent cancers or history of venous thromboembolic events [2, 3, 6, 7]. The American College of Obstetrics and Gynecology (ACOG) recently recommended that non-hormonal options should be used as first-line treatment for women with a history of hormone-dependent breast cancer. Although current data do not show an increased risk of cancer recurrence when using vaginal estrogen, ACOG recommends coordinating with the patient’s oncologist, as well as counseling the patients about the potential risks before initiating treatment [8].
In the field of gynecology, CO2 laser treatments have been used for vaporizing condyloma and intraepithelial neoplasia for almost 30 years [2]. In 2014, the Food and Drug Administration approved fractional CO2 lasers for use in skin resurfacing as well [9]. Since then, there has been a renewed interest in other clinical uses of CO2 lasers. Since then, several small case series and prospective studies with short-term follow-up have demonstrated that CO2 lasers improve symptoms of GSM and have high satisfaction rates [3-5, 10-15]. Studies with longer follow-up have highlighted that most of the improvements are sustained for about 1 year [1, 16, 17]. However, these studies utilized limited clinical evaluation methods and a visual analog scale of satisfaction to determine their primary outcomes.
Objective
Our objective is to prospectively evaluate pixelated CO2 laser therapy for the treatment of symptomatic GSM over 1 year, using both subjective and objective assessment methods.
| Materials and Methods | ▴Top |
The study was designed as a prospective non-randomized study to assess the efficacy of pixelated CO2 laser therapy (FemiLift Pixel CO2 laser, Alma Lasers; Caesarea, Israel). Subjects with symptoms of GSM were recruited. This study was approved by the Cleveland Clinic Florida Institutional Review Board (FLA15-110), and registered on Clinicaltrials.gov (NCT02747641). Inclusion criteria were healthy, non-smoking women between the ages of 35 and 70 years old. Subjects were required to have normal Papanicolaou testing within the past year, negative urine cultures, and a vaginal canal free of any lesions or abnormalities. Subjects were excluded if they had a positive pregnancy test, planned pregnancy during the study period, or used photosensitive drugs. They were also excluded if they had undergone pelvic surgical procedures within 6 months prior to treatment, vaginal prolapse greater than or equal to stage two, a body mass index greater than 30, any prior reconstructive pelvic floor surgery, active human papillomavirus, active herpes simplex virus infections, or undiagnosed vaginal bleeding.
Once recruited, subjects provided informed consent and underwent baseline assessments. Assessments included a review of medical history and medications, a pre-treatment pelvic exam, and a pregnancy test. Subjects underwent two standardized physician assessments of vaginal atrophy: the Bachmann Vaginal Health Index (BVHI) and Vaginal Health Assessment (VHA) [18, 19]. These instruments include a visual assessment of vaginal estrogenization including moisture, rugation, color, and pH. Each subject then completed five subjective questionnaires to assess the symptoms associated with GSM. These questionnaires included a visual analog grading scale for vaginal atrophy symptoms (VAS-VA), which was graded from 0 to 10, where 0 signified “no distress” and 10 signified “unbearable distress”. Subjects also completed the Symptoms of Atrophic Vaginitis Questionnaire (SAVQ), and a modified Vulvovaginal Symptom Questionnaire (mVSQ) [19, 20] (Supplementary Material 1, www.jcgo.org). Subjects also completed the Urinary Distress Inventory (UDI-6) to assess symptoms of urinary dysfunction and the Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire (PISQ-12) to assess sexual function [21, 22].
Subjects underwent pixelated CO2 laser treatments every 4 weeks for a total of three treatment sessions. Each treatment was administered by a member of the study staff who had undergone standardized training. The hand piece diffuses the laser beam using a 9 × 9 mm template into an 81-pixel beam. The hand piece was inserted to the apex of the vagina. The laser was triggered in 12 increments circumferentially and then withdrawn 1 cm at a time, triggering 12 circumferential pulses at each level until 2 cm cephalad to the introitus. This process was then repeated twice more. The first treatment used the “medium” mode, and was set to 80 mJ/pixel and single pulses. For the second and third treatments, the same process was repeated, however the laser intensity was increased to the “high” mode and was set 100 mJ/pixel. Subjects were instructed about post-treatment care, including vaginal rest for 3 days, and discontinuation of any prescriptions or over the counter vaginal medications throughout the study period.
Two weeks after each treatment session, subjects returned for evaluation, which included the same two physician assessments and the five questionnaires that were completed at the baseline assessment. Additionally, at baseline and at 1 year, vaginal samples were collected for cytologic maturation index assessment, and representative vaginal biopsies were obtained from three random subjects. The three subjects were chosen by random number generator which identified three unique subjects ID numbers between 1 and 15 prior to the initiation of the study, and each consented to the biopsies.
The selected primary outcome was the change in signs and symptoms of GSM as measured by the seven assessment methods from baseline to 1-year follow-up. Secondary outcomes included short-term follow-up assessment scores, as well as a change in vaginal histology. Short-term follow-up was assessed by comparing the pre-treatment assessment scores with the post-treatment assessment scores 2 weeks after the third treatment session (approximately 10 weeks after the first session).
Descriptive statistics were calculated for the 15 subjects. Quantitative continuous data were reported using mean and standard deviations, while quantitative discrete data were reported using median and interquartile ranges. Qualitative variables were summarized using absolute numbers and percentages. Pre-treatment and post-treatment scores for each of the assessments were calculated and compared. The Shapiro-Wilks test was used to test for normality of continuous data. Student’s paired t-test was used for normally distributed data and the Wilcoxon signed-ranks test for skewed data. Categorical data were analyzed using Pearson’s Chi-square test or Fisher’s exact test where appropriate. A P value of less than 0.05 was considered statistically significant. All analyses were performed using JMP version 13.0.0 (SAS Institute Inc., Cary, NC).
| Results | ▴Top |
Fifteen postmenopausal women were prospectively enrolled in the study from May 2016 to August 2016. The average age of the subjects was 58.3 ± 8.75 years (range 43 to 70 years) and average body mass index was 25.5 ± 3.39 kg/m2. Forty percent (n = 6) had a history of breast cancer and 33.3% (n = 5) had previously tried vaginal estrogen for GSM. One subject complained of stress urinary incontinence and three of urinary urge incontinence (Table 1). Subjects had an average study follow-up of 11.2 ± 0.50 months (range 11 - 12 months). No significant adverse events were reported throughout the entire study. Some patients reported a mild blood-tinged vaginal discharge for a few days, but no overt bleeding or pain following treatment. During each treatment session, patients reported discomfort with probe insertion (despite application of a small amount of baby oil) and a sensation of heat with firing of the laser, but only one patient reported mild pain which responded to pre-treatment with 2% local lidocaine jelly, which was washed out prior to each session. Almost uniformly, patients reported some discomfort with turning of the vaginal probe due to labial dryness.
 Click to view | Table 1. Baseline Characteristics of Subjects Undergoing Laser Treatment for GSM |
Short-term follow-up at 3.5 months demonstrated significant improvements in both of the physician assessments, as well as significant improvements in all of the patient subjective assessments except the UDI-6 (Table 2). For all of the assessments, a lower score indicated fewer or less severe symptoms in GSM, except for the BVHI where a higher score indicated improvement in symptoms. For the six significantly improved assessments, there appeared to be a linear progressive improvement with each treatment session (Fig. 1), with significant improvement seen in the BVHI, VHA, VAS-VA, SAVQ, and mVSQ after just one treatment session (P ≤ 0.001, P = 0.001, P = 0.039, P = 0.008, P = 0.034, respectively).
 Click to view | Table 2. Short-Term Follow-Up Comparing GSM Assessments From Baseline to 2 Weeks After the Third Treatment Session |
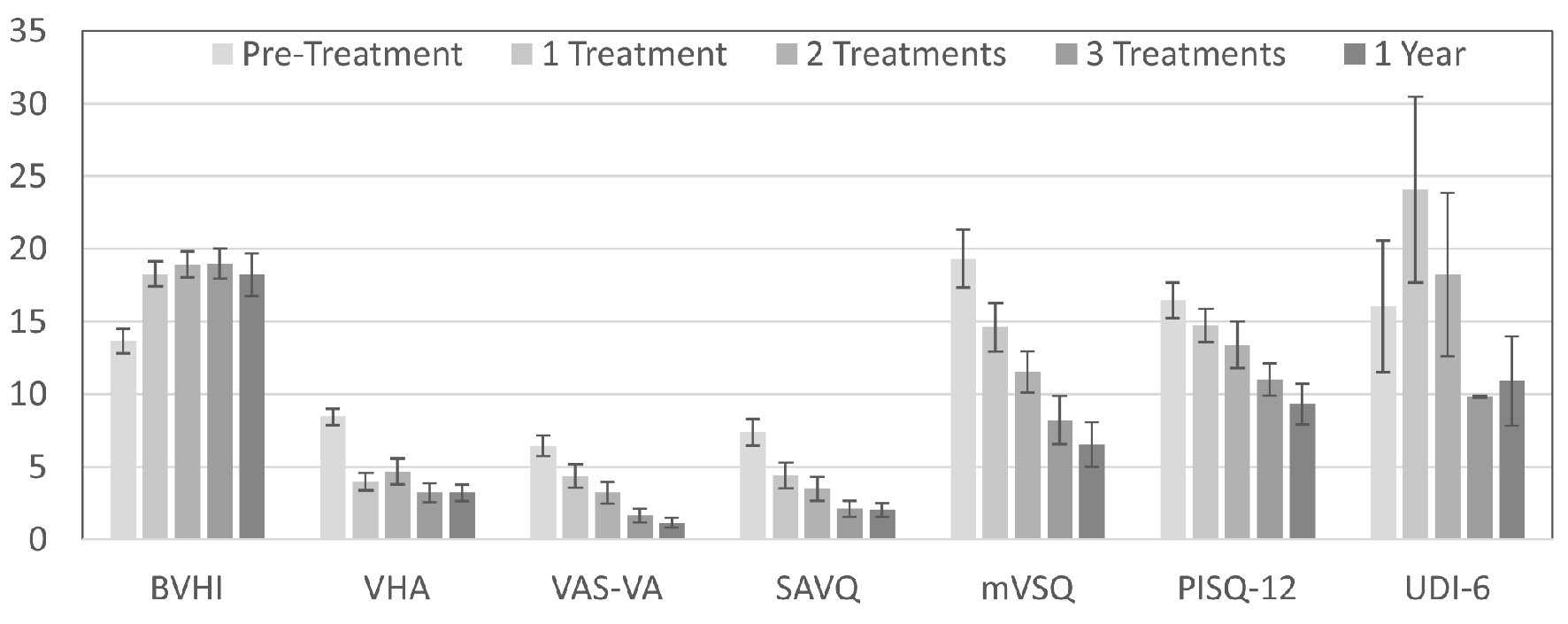 Click for large image | Figure 1. Change in GSM assessment scores over time with pixelated CO2 laser treatment. Lower scores indicate fewer or less severe symptoms for all assessments, except the BVHI. |
Similar to short-term follow-up, 1-year follow-up demonstrated significant improvements over baseline assessments in both of the physician as well as in all of the patient subjective assessments except the UDI-6 (Table 3). The short-term follow-up assessments were compared to the 1-year follow-up assessments. There were no statistical differences in any of the assessments between the short-term and 1-year follow-up periods (Table 4).
 Click to view | Table 3. Comparison of Assessments of GSM From Baseline to 1 Year |
 Click to view | Table 4. Comparison of Assessments of GSM Between Short-Term Follow-Up and 1Year Follow-Up |
Interestingly, there were no significant changes between baseline and 1-year follow-up with regards to the vaginal maturation indices (MD: -0.55 (95% confidence interval (CI): -16.03, 14.94), P = 0.734). Histologically, the surface epithelium on the vaginal biopsies ranged from within normal limits to mild squamous atrophy. There was mild submucosal vascular congestion in all specimens, with evidence of neovascularization (Fig. 2).
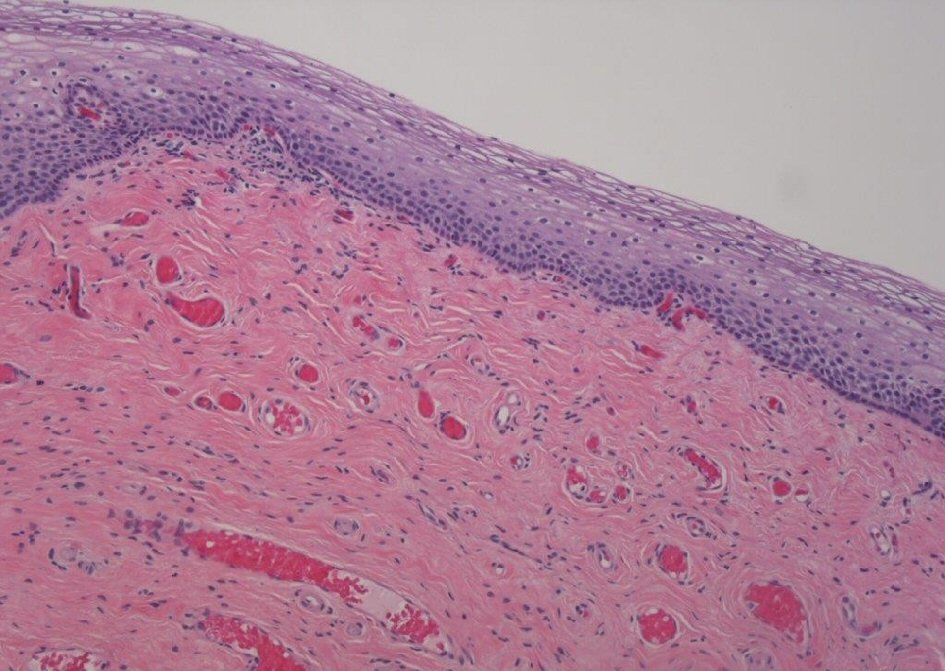 Click for large image | Figure 2. Vaginal epithelial biopsy 1 year after laser therapy. |
| Discussion | ▴Top |
Based upon the seven objective and subjective evaluations, there was significant improvement in signs and symptoms of GSM following pixelated CO2 laser treatments in the short-term, and these improvements were sustained at 1-year follow-up. In particular, this study highlights improvements in vulvovaginal atrophy and sexual function. Similar to other short-term studies, this study shows significant improvement in both subjective and objective findings of vulvovaginal atrophy after just one treatment session. However, improvements were not maximized until after the third treatment, suggesting that less than three treatment sessions may lead to suboptimal outcomes. Our 1-year follow-up also coincides with findings with other long-term studies [1, 16, 17]. However, this study utilized more extensive evaluation methods than previous studies.
Histologically and cytologically, the findings of this study differ significantly from previous studies. On microscopic evaluation, the changes to the vaginal epithelium were mostly limited to neovascularization of the submucosal region, as can be clearly seen on the vaginal wall biopsies. In contrast, Pagano et al demonstrated increased epithelial thickness, as well as restoration of epithelial and sub-epithelial structures after fractionated CO2 laser therapy, which are similar to the effects found after treatment with estrogen [10]. Cruz et al also used the maturation index to evaluate the vaginal epithelial cells and noted a significant increase in the maturation value in patients who underwent fractional laser treatment, again similar to the findings associated with estrogen therapy [3]. Other studies have also reported vaginal cytology improvement with CO2 laser therapy, similar to that seen with local estrogen.
The findings of this study included lack of epithelial maturation after CO2 laser therapy, highlighting that although the pixelated CO2 laser significantly improves symptoms of vulvovaginal atrophy like estrogen therapy; the mechanism of action may be different. Other recent studies have demonstrated similar findings. Takacs et al showed that CO2 laser treatment improved vaginal dryness on a VAS, with no improvement in vaginal cytology (maturation Index) [23]. In a randomized trial comparing estrogen cream to CO2 laser therapy for GSM, Paraiso et al demonstrated similar improvement in symptomatology, but vaginal maturation index scores were higher in the estrogen group [24]. Larger studies will be required to clarify the actual mechanism of action of CO2 laser therapy in improving symptoms of GSM.
Although there has been a recent growth in research on laser therapy for symptoms of GSM, there is a dearth of information on laser use for urinary incontinence. Two prior studies noted improvement in stress urinary incontinence symptoms, and one noted improvement in women with overactive bladder [10, 15, 25]. In our study, there were no improvements in UDI-6 scores in the short-term or after 1 year. However, our study is limited in that only four subjects had urinary incontinence complaints before treatment.
CO2 laser treatments are technically easy to administer in a short outpatient visit. Most patients experience a sensation of heat, but no significant pain. All of the current studies have reinforced the safety of the laser for this indication, as minimal to no significant adverse events have been reported. The subjects in our study did not have any significant adverse events, which is in concordance with the prior studies [3, 12, 15, 17]. Although rare, the most common side effects are usually transient and include mild vaginal discharge, burning, itching, bruising and swelling [4].
The North American Menopause Society (NAMS) has cautioned that currently laser therapy is not intended for use for vaginal rejuvenation or tightening, nor stress urinary incontinence or sexual health concerns that are not associated with vaginal atrophy. In addition, NAMS has warned patients that since this therapy is not covered by insurance, patients may incur substantial out-of-pocket costs [2]. Another potential drawback of laser therapy is the concern of the possible consequences of repeated and long-term use. At this time, most experienced users recommend an annual booster treatment, despite the lack of evidence to justify the need for or the safety of repeat therapy [2].
The strengths of this study include the extensive evaluation of the symptoms of GSM including five subjective and two objective scoring systems. In addition, maturation indices and histological biopsies were used to evaluate the vaginal epithelium. One year outcomes are reported, and are uniformly significant. The weaknesses of this study include the small sample size and a lack of randomization or a control/placebo/sham arm. In addition, our study population consisted of relatively healthy, post-menopausal non-obese women. This narrow population decreases the generalizability of the study.
Conclusions
CO2 fractionated laser therapy appears to be of significant value for GSM in those symptomatic women in whom estrogen is not desired, or recommended, such as women with hormone-dependent breast cancers or those with a history of venous thromboembolic events. This study adds long-term data on the efficacy and safety of the CO2 lasers for use in gynecology. In addition, the lack of histologic epithelial changes highlights the need for more research to better understand the mechanism of action and how this therapeutic modality differs from that of estrogen therapy. In summary, CO2 laser therapy provided significant improvement in symptoms of GSM, and results were maintained for 1 year. Larger randomized studies are needed to confirm the findings of this study and to better stratify this treatment modality amongst the other available options.
| Supplementary Material | ▴Top |
Suppl 1. Modified Vulvovaginal Symptom Questionnaire.
Acknowledgments
None to declare.
Financial Declaration
Equipment and a research grant were provided to Cleveland Clinic Florida for this study by Alma Lasers, who did not have any input on data collection, analysis of statistics, or the presentation or publication of the data.
Conflict of Interest
Dr. Schachar: None. Dr. Devakumar: None. Dr. Martin: None. Dr. Hurtado: Sponsored research: Acell, Alma Laser, Coloplast, Cook Biomedical. Dr. Davila: Research grant: Acell, Coloplast, Cook Biomedical, Pfizer. Speaker: Alma Lasers, Astellas. Data were presented at: International Urogynecological Association 42nd Annual Meeting. Vancouver, Canada, June 20 - 24, 2017; American Urogynecologic Society PFD Week 2017, Providence, Rhode Island, October 3 - 7, 2017; and American Society for Laser Medicine and Surgery 38th Annual Conference, Dallas, Texas, April 11 - 15, 2018.
Informed Consent
Informed consents were obtained from all subjects.
Author Contributions
Dr. Schachar: data collection, data analysis, and manuscript writing. Dr. Devakumar: data collection. Dr. Martin: data collection. Dr. Hurtado: protocol/project development, and manuscript editing. Dr. Davila: protocol/project development, and manuscript editing.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Sokol ER, Karram MM. Use of a novel fractional CO2 laser for the treatment of genitourinary syndrome of menopause: 1-year outcomes. Menopause. 2017;24(7):810-814.
doi pubmed - Streicher LF. Vulvar and vaginal fractional CO2 laser treatments for genitourinary syndrome of menopause. Menopause. 2018;25(5):571-573.
doi pubmed - Cruz VL, Steiner ML, Pompei LM, Strufaldi R, Fonseca FLA, Santiago LHS, Wajsfeld T, et al. Randomized, double-blind, placebo-controlled clinical trial for evaluating the efficacy of fractional CO2 laser compared with topical estriol in the treatment of vaginal atrophy in postmenopausal women. Menopause. 2018;25(1):21-28.
doi pubmed - Arroyo C. Fractional CO2 laser treatment for vulvovaginal atrophy symptoms and vaginal rejuvenation in perimenopausal women. Int J Womens Health. 2017;9:591-595.
doi pubmed - Sokol ER, Karram MM. An assessment of the safety and efficacy of a fractional CO2 laser system for the treatment of vulvovaginal atrophy. Menopause. 2016;23(10):1102-1107.
doi pubmed - Vieira-Baptista P, Marchitelli C, Haefner HK, Donders G, Perez-Lopez F. Deconstructing the genitourinary syndrome of menopause. Int Urogynecol J. 2017;28(5):675-679.
doi pubmed - Labrie J, Berghmans BL, Fischer K, Milani AL, van der Wijk I, Smalbraak DJ, Vollebregt A, et al. Surgery versus physiotherapy for stress urinary incontinence. N Engl J Med. 2013;369(12):1124-1133.
doi pubmed - ACOG Committee Opinion No. 659 Summary: The use of vaginal estrogen in women with a history of estrogen-dependent breast cancer. Obstet Gynecol. 2016;127(3):618-619.
doi pubmed - Fractional Laser Treatment of Vulvovaginal Atrophy and U.S. Food and Drug Administration Clearance - ACOG. https://www.acog.org/Clinical-Guidance-and-Publications/Position-Statements/Fractional-Laser-Treatment-of-Vulvovaginal-Atrophy-and-US-Food-and-Drug-Administration-Clearance. Accessed February 27, 2018.
- Pagano I, Gieri S, Nocera F, et al. Evaluation of the CO2 laser therapy on Vulvo-Vaginal Atrophy (VVA) in oncological patients: preliminary results. J Cancer Ther. 2017;8(5):452-463.
doi - Salvatore S, Leone Roberti Maggiore U, Athanasiou S, Origoni M, Candiani M, Calligaro A, Zerbinati N. Histological study on the effects of microablative fractional CO2 laser on atrophic vaginal tissue: an ex vivo study. Menopause. 2015;22(8):845-849.
doi pubmed - Salvatore S, Nappi RE, Zerbinati N, Calligaro A, Ferrero S, Origoni M, Candiani M, et al. A 12-week treatment with fractional CO2 laser for vulvovaginal atrophy: a pilot study. Climacteric. 2014;17(4):363-369.
doi pubmed - Salvatore S, Nappi RE, Parma M, Chionna R, Lagona F, Zerbinati N, Ferrero S, et al. Sexual function after fractional microablative CO(2) laser in women with vulvovaginal atrophy. Climacteric. 2015;18(2):219-225.
doi pubmed - Siliquini GP, Tuninetti V, Bounous VE, Bert F, Biglia N. Fractional CO2 laser therapy: a new challenge for vulvovaginal atrophy in postmenopausal women. Climacteric. 2017;20(4):379-384.
doi pubmed - Perino A, Calligaro A, Forlani F, Tiberio C, Cucinella G, Svelato A, Saitta S, et al. Vulvo-vaginal atrophy: a new treatment modality using thermo-ablative fractional CO2 laser. Maturitas. 2015;80(3):296-301.
doi pubmed - Behnia-Willison F, Sarraf S, Miller J, Mohamadi B, Care AS, Lam A, Willison N, et al. Safety and long-term efficacy of fractional CO2 laser treatment in women suffering from genitourinary syndrome of menopause. Eur J Obstet Gynecol Reprod Biol. 2017;213:39-44.
doi pubmed - Pieralli A, Fallani MG, Becorpi A, Bianchi C, Corioni S, Longinotti M, Tredici Z, et al. Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Arch Gynecol Obstet. 2016;294(4):841-846.
doi pubmed - Bachmann G, Notelovitz M, Kelly S, Owens A, Thompson C. Long term nonhormonal treatment of vaginal dryness. Clin Pract Sex. 1992;8(8/9):3-8.
- Davila GW, Singh A, Karapanagiotou I, Woodhouse S, Huber K, Zimberg S, Seiler J, et al. Are women with urogenital atrophy symptomatic? Am J Obstet Gynecol. 2003;188(2):382-388.
doi pubmed - Erekson EA, Yip SO, Wedderburn TS, Martin DK, Li FY, Choi JN, Kenton KS, et al. The Vulvovaginal Symptoms Questionnaire: a questionnaire for measuring vulvovaginal symptoms in postmenopausal women. Menopause. 2013;20(9):973-979.
doi pubmed - Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA. Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program for Women Research Group. Neurourol Urodyn. 1995;14(2):131-139.
doi pubmed - Rogers RG, Kammerer-Doak D, Villarreal A, Coates K, Qualls C. A new instrument to measure sexual function in women with urinary incontinence or pelvic organ prolapse. Am J Obstet Gynecol. 2001;184(4):552-558.
doi pubmed - Takacs P, Sipos AG, Kozma B, Cunningham TD, Larson K, Lampe R, Poka R. The Effect of Vaginal Microablative Fractional CO2 Laser Treatment on Vaginal Cytology. Lasers Surg Med. 2020;52(8):708-712.
doi pubmed - Paraiso MFR, Ferrando CA, Sokol ER, Rardin CR, Matthews CA, Karram MM, Iglesia CB. A randomized clinical trial comparing vaginal laser therapy to vaginal estrogen therapy in women with genitourinary syndrome of menopause: The VeLVET Trial. Menopause. 2020;27(1):50-56.
doi pubmed - Tien YW, Hsiao SM, Lee CN, Lin HH. Effects of laser procedure for female urodynamic stress incontinence on pad weight, urodynamics, and sexual function. Int Urogynecol J. 2017;28(3):469-476.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
