| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Review
Volume 10, Number 2, June 2021, pages 40-45
The Gynecologic Surgeon’s Approach to Evaluating a Patient With Suspected Endometriosis: A Systematic Review
Tracey Jurona, b, George Seamana
aQueens Hospital Center, Jamaica, NY, USA
bCorresponding Author: Tracey Juron, Queens Hospital Center, 82-68 164th Street, Jamaica, NY, USA
Manuscript submitted April 7, 2021, accepted June 8, 2021, published online June 24, 2021
Short title: Evaluating Suspected Endometriosis
doi: https://doi.org/10.14740/jcgo742
| Abstract | ▴Top |
Background: The objective of this review is to assess the most recent literature recommendations for how to approach a patient presenting with chronic pelvic pain (CPP), when a high clinical suspicion of endometriosis exists, to prevent the clinical and economic burden associated with delayed diagnosis.
Methods: An online review of PubMed and Europe PubMed Central was conducted with a final total of 11 articles being reviewed. The search was limited to the preoperative management of these patients, excluding literature focused on the effectiveness of medical vs. surgical management of the disease. There is no main outcome measure.
Results: A thorough history of patient symptomatology and physical exam are paramount to a timely diagnosis of endometriosis. Additionally, the literature supports the use of sonogram as the first-line imaging modality for diagnosis; however, its utility is limited to detection of the two less common forms of the disease, endometrioma and deep peritoneal lesions, with less reliable prediction of superficial implants. If a high clinical suspicion exists for either endometrioma or deep infiltrating disease, magnetic resonance imaging can reliably demonstrate these findings. The gold standard method of laparoscopy for definitive diagnosis is not controversial; however, the literature suggests that proper, sequential evaluation by history, physical and imaging may aid in accurate and timely diagnosis. Delay in the diagnosis of endometriosis creates a significant burden on patient well-being as well as an economic burden on the healthcare system.
Conclusion: Further studies assessing biomarkers of endometriosis and specific features of the disease in time are needed to better understand the etiology and pathogenesis and to subsequently decrease disease burden.
Keywords: Chronic pelvic pain; Endometriosis; Endometriosis diagnosis; Epidemiology; Pathogenesis
| Introduction | ▴Top |
Endometriosis is a benign gynecologic disease defined as extra-uterine implantation of endometrial glands and stroma. As many as 10% of reproductive aged women are affected, though the reported prevalence is influenced by the patients’ presenting complaints and the method of diagnosis [1]. For example, endometriosis is present in 21-47% of women presenting with subfertility and 71-87% of those suffering with chronic pelvic pain (CPP) [2-4].
There are several working theories to explain the pathogenesis of this disease; historically, the most accepted is the theory of retrograde menstruation. Studies have shown that occlusion of the outflow tract increases retrograde flow of endometrial cells and results in an increased incidence of endometriosis. This theory was supported to a large extent by a study of baboons at the Institute of Primate Research in Nairobi, Kenya from 1990 to 1994, demonstrating that occlusion of the cervix or intrapelvic injection of menstrual endometrium caused moderate to severe disease similar to that seen in spontaneous disease [5]. More recent theories include the ectopic differentiation of stem cells, lymphatic or vascular spread of endometrial tissue or metaplastic transformation of the peritoneum into tissue histologically identical to the endometrium [3]. The most recent, more advanced understanding of the complexity of the disease has come from observation of symptomatic patients after surgery and from research on patient-reported symptoms and burden of disease.
Part of the difficulty in diagnosing endometriosis is the enigma it often presents as, appearing quite similar to a variety of differential diagnoses. Patients present with symptoms of dysmenorrhea, dyspareunia, dyschezia, infertility or subfertility and abdominal/pelvic pain. Symptoms often impact both mental and physical health but a timely clinical assessment may be hindered by this symptomatic overlap with other diseases, including inflammatory bowel disease, pelvic inflammatory disease, interstitial cystitis, pelvic floor disorders, anxiety or depression [2].
A detailed history and physical exam are paramount to accurately diagnosing these patients. One of the earliest components of the evaluation must include a self-rated pain score, typically on a 1-10 scale. According to a systematic literature review assessing endometriosis-related pain from a total of 258 studies, the Visual Analog Scale (VAS) is the most frequently used pain scale and, together with the Numerical Rating Scale (NRS), seems the best adapted for endometriosis pain measurement [6]. Patients should also be encouraged to complete the Endometriosis Health Profile (EHP-30) questionnaire indicating the extent of self-reported ill health on each domain measured, including work-life balance, relationship with family and sexual relationships, to name a few [7]. Of note, it is well documented in the literature that superficial peritoneal implants do not correlate well with measures of perceived pain.
There are conflicting opinions in the literature regarding the utility of imaging in evaluating endometriosis. Following a comprehensive physical exam, the surgeon may choose to perform imaging studies such as pelvic ultrasound or magnetic resonance imaging (MRI) to confirm physical exam findings and to facilitate potential pre-operative planning.
Historically, literature on this topic has focused on perception of pain and its strength in predicting the quality and quantity of endometriotic lesions at laparoscopy. The goal of this literature review is to summarize the most recent recommendations for evaluating patients with suspected endometriosis, preoperatively. What criteria are used to determine who is ultimately a candidate for laparoscopy, either for diagnostic purposes or for surgical management? This review does not fill in gaps in existing literature but rather serves as a reiteration of existing data which is paramount to adequately caring for these patients.
The gold standard method for diagnosing endometriosis is not controversial. The approach to a patient suffering from CPP with suspected endometriosis, however, is not black and white. The purpose of this literature review is to discuss the nuances associated with evaluating a patient with CPP. What clinical presentation is most likely to trigger a suspicion of endometriosis and how do we often reach this conclusion? The rationale for performing this review lies in the long-standing complexity of endometriosis and the difficulty in accurately identifying these patients when they present. The objective is to demonstrate the consensus in the literature on the initial approach to a patient with CPP with high suspicion of endometriosis as the underlying cause.
| Methods | ▴Top |
Search strategy
Comprehensive search of PubMed and Europe PubMed Central electronic search engines was performed using the cross references NEJM, Cochrane, NIHR, and AJOG.
Data extraction
Articles were screened and selected by this author as an independent researcher. An initial total of 190 articles were reviewed using the keywords chronic pelvic pain, endometriosis, epidemiology, pathogenesis within the above search engines. Articles were then screened for relevance and must be dated between the years 2015 and 2021 for inclusion. Articles excluded were those limited by a specific patient population, i.e., adolescence and systematic literature reviews. The remaining articles were assessed for eligibility, with further exclusion of any duplicates, articles focused on the medical management of the disease or the effectiveness of laparoscopic excision specifically for the management of endometriosis and articles in non-English languages. A total of 11 articles remained for inclusion in this qualitative analysis.
| Results | ▴Top |
Figure 1 depicts the article search from the years 2015 to 2020. A total of 190 articles were obtained and screened. Based on titles and abstract, 162 articles were omitted if dated prior to the year 2015, limited by a specific patient population or if designed as a systematic literature review. Articles limited to a specific patient population, i.e., adolescence, were excluded in order to evaluate a more widespread patient demographic. From the 28 articles remaining, 17 full text articles were rejected with the majority of these rejected due to a focus on the medical management of the disease or the effectiveness of laparoscopic excision of endometriosis. Furthermore, studies of women with CPP attributable to other known causes and women undergoing laparoscopy for other gynecologic indications, such as known ovarian cyst, sterilization or malignancy, were excluded. Ultimately, 11 articles were found to be eligible for this literature review.
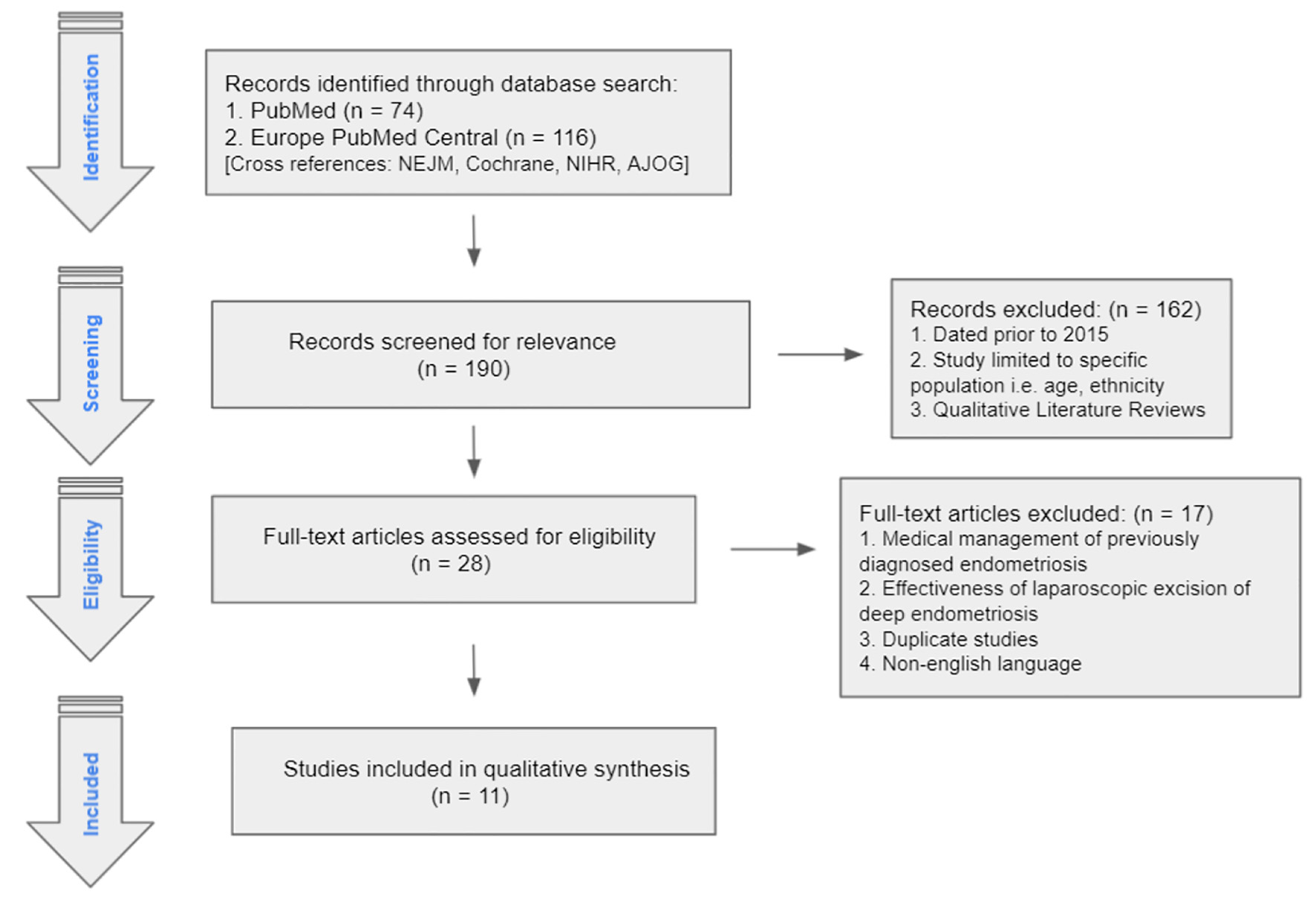 Click for large image | Figure 1. PRISMA diagram. |
The breakdown of eligible articles includes overview articles [8-10], prospective cohort studies [11, 12], systematic literature review with meta-analysis [13], cross-sectional studies [9, 14], retrospective database study [15], quality assessment [16] and case-control [17].
Evaluation of the patient (objective 1)
History and physical
The primary purpose of a detailed history is to obtain a patient’s symptoms and to evaluate her journey to the present date to better assess the symptom duration and subsequent impact on her quality of life. The physician should obtain a comprehensive review of past medical history, past surgical history and an understanding of endometriosis-associated pain (EAP) symptoms, including cyclic pelvic pain, dysmenorrhea, deep dyspareunia, dysuria and dyschezia [8]. Following the history, a meticulous physical exam should include an abdominal, monodigital transvaginal exam and bimanual exam with active involvement of the patient. This “pain-mapping” approach will help guide accurate diagnosis and management [8].
A cross-sectional survey was conducted among women aged 18 - 49 years in the United States in the year 2012. The purpose of the study was to ascertain the prevalence of symptoms associated with diagnosed endometriosis (DE) and to evaluate patient-reported severity of symptoms. An understanding of symptomatology in diagnosed cases of endometriosis is crucial to better evaluate a patient who presents initially with CPP, with suspected endometriosis. Endometriosis-specific symptoms included menstrual vs. non-menstrual pelvic cramping, dyspareunia, menorrhagia, abnormal uterine bleeding, constipation, bloating, fatigue and infertility. Weighted logistic regression was used to assess the difference in symptom burden between those with endometriosis and those without. Among women with typical endometriosis symptoms, the percentage who experienced only one symptom was greater among women without DE than those with DE (35.1% vs. 30.1%, P < 0.001). In contrast, those who reported two or three of the symptoms were two times and four times more likely, respectively, to have DE (two symptoms: 23.6% vs. 13.4%; three symptoms: 13.9% vs. 3.7%, P < 0.001 for both) [9]. One-third of the women with DE reported being “extremely bothered” by their symptoms.
While a thorough history and physical exam is essential in evaluation of patients with CPP, there is robust literature supporting the added utility of imaging studies prior to considering surgery.
Imaging
Ultrasound is often used as the first-line imaging modality in patients with CPP. The same holds true when endometriosis is suspected. The utility of sonogram and MRI largely depends on the type of endometriotic lesion. Lesions associated with endometriosis can be classified into three categories: superficial peritoneal implants, endometriomas and deep infiltrating disease (nodules penetrating > 5 mm through peritoneum). Superficial lesions are the most prevalent and the least likely to be detected on imaging. By contrast, endometriomas are readily identified on pelvic sonograms or MRI with more than 90% sensitivity and specificity [18]. Deep infiltrating endometriosis (DIE) can be found on ultrasound performed by a skilled sonographer while MRI has a 94% sensitivity and 79% specificity for DIE.
Similarly, Okaro et al demonstrated that certain ultrasound-based “soft” and “hard” markers may be strong predictors of pelvic pathology. Soft markers were considered reduced ovarian mobility and site-specific pelvic tenderness while hard markers were endometrioma or hydrosalpinx [11]. The authors concluded this diagnostic approach improves the detection and the exclusion of significant pelvic pathology, lessening the necessity of laparoscopy.
As an adjunct to a consensus opinion by the International Deep Endometriosis Analysis (IDEA) group, Leonardi and Condous (2018) developed a more practical and comprehensive method to perform an ultrasound in an effort to understand the full extent of disease prior to performing any surgical intervention. Their evaluation described a stepwise approach of examining the bowel, uterus, adnexa, anterior compartment, posterior compartment and lastly, an evaluation of site-specific tenderness elicited by the abdominal or transvaginal probe [10]. Those with clinical and/or sonographic evidence of DIE should be referred to a specialist for a comprehensive discussion of medical or surgical management.
A large prospective cohort study was performed to evaluate the added value of MRI after dynamic transvaginal ultrasound (TVUS) for preoperative staging of endometriosis. A total of 363 patients included in the study underwent a history, clinical exam and transvaginal sonogram. Of these, 72 underwent the complete diagnostic pathway (the above plus MRI and surgery). Results showed that adding MRI routinely to the diagnostic procedure of endometriosis did not significantly improve the sensitivity or specificity [12]. When considering which imaging modality to incorporate pre-operatively, it is important to understand if there is any added diagnostic benefit to additional testing.
A systematic review of 30 studies with 4,565 participants analyzed the sensitivity and specificity of transrectal ultrasound (TRUS), TVUS and MRI for diagnosing DIE. Results suggest that while physical examination has intermediate diagnostic accuracy, TRUS, TVUS and MRI have high diagnostic accuracy for DIE [13].
We can conclude from the above sources that ultrasound should continue to be utilized as a first-line imaging modality. The decision to add MRI should be at the discretion of the treating physician. Gynecologic surgeons should manage these patients judiciously, with care not to delay surgical intervention for aid in diagnosis.
Diagnostic delay and its implications (objective 2)
On average, the delay between initial symptom onset and diagnosis is 7 - 9 years. This delay is multifaceted and has both clinical and economic effects. A retrospective database study of more than 11,000 patients demonstrated that those with a “long delay” between symptom onset and diagnosis, defined as 3 - 5 years, had a significantly higher clinical burden with more endometriosis-related symptoms compared to patients with shorter delays [9]. Contributing to this delay is the ambiguity of presenting symptoms, the lack of clear understanding of the pathogenesis of disease and the absence of a valid, less invasive diagnostic test [15]. A quality assessment of data pooled from cross-sectional and randomized control trials of reproductive aged women with characteristic features of endometriosis concluded that no single imaging modality has enough accuracy to replace surgical diagnosis [16]. The limitation of ultrasound as a diagnostic tool is that its utility is largely dependent on the level of expertise of the sonographer. Additionally, ultrasound is not reliable for detection of the most common subgroup of the disease, the superficial subtype.
In a study looking at healthcare costs and resource utilization, pre-diagnosis endometriosis-related healthcare costs accounted for 12.5% of all-cause costs. “This proportion was highest among patients with longer diagnostic delays with values of 9.7%, 13.3% and 13.9% in patients with short (< 1 year), intermediate (1 - 3 years) and long delays (3 - 5 years), respectively” [15]. This article affirms the established knowledge that longer diagnostic delays lead to significantly higher clinical and economic burden.
A similar cross-sectional study, conducted in the USA, gathered patients’ responses to a series of questions pertaining to the timing of their symptoms and timing of their diagnosis, or initial suspicion. “From a total of 638 respondents, the percentage of women with mild, moderate and severe symptoms was 8.3%, 37.2% and 54.5%, respectively. Time from symptom onset to first physician visit was 1.7, 2.6 and 2.3 years, respectively; time from first physician visit to diagnosis was 1.2, 2.0 and 2.2 years, respectively” [14]. These findings underscore what is likely an improvement in physician education and understanding of the complexity of the disease process.
A nested case-control study was executed in Scotland using the electronic medical record system. The purpose was to determine whether a certain combination of symptoms over a specified amount of time can be used to more accurately predict a diagnosis of endometriosis. Using odds ratios to assess occurrence of composite features, the researchers concluded that the combination of pelvic pain and menstrual symptoms within the same year and lower gastrointestinal (GI) symptoms within 90 days of pelvic pain had higher odds ratios compared to controls [17]. This study added new information to existing literature, suggesting that there may be certain trends in patient presentation that can facilitate a shortened time to diagnosis.
| Discussion | ▴Top |
The purpose of this literature review is to assess the most recent recommendations for evaluating a patient with suspected endometriosis. The clinical manifestations of this disease are variable, often leading the physician down a pathway to several other differential diagnoses. Delayed diagnosis has been shown to cause a significant burden on patient well-being as well as economic burden on the healthcare system. The focus of this paper is the importance of accurate and timely diagnosis of this disease and the utility of preoperative imaging to determine disease severity, prior to considering surgical intervention.
The burden of disease is both clinical and economical, with significant effects on patients’ mental and physical health and healthcare costs. Furthermore, patients suffer from long-term sequelae when their disease goes unrecognized. It is the multifactorial nature of the disease presentation, often overlapping with several other differential diagnoses including irritable bowel, interstitial cystitis, pelvic floor disorders, pelvic adhesive disease, anxiety and depression that play a major role in delayed diagnosis.
The literature supports the use of pelvic and transvaginal ultrasound as the first-line imaging modality in patients with suspected endometriosis; however, the most significant barrier to its utility in practice is the difficulty in detecting the most common form of the disease, superficial peritoneal endometriosis. As for the two remaining subtypes of endometriosis, ultrasound and MRI have both reasonably proven to depict disease. Despite the high sensitivity and specificity of imaging, laparoscopy remains the gold standard for confirming the diagnosis, either by visual inspection or by histology. Studies have shown, however, that patients who undergo diagnostic or therapeutic laparoscopy often require subsequent laparoscopy for persistent pain, suggesting poor therapeutic benefit of surgical intervention.
It is justifiable to label a patient with endometriosis as early as their initial evaluation when the symptoms described above are reported and appear to have a significant impact on the patient’s quality of life. Ultrasound is a non-invasive study that can be utilized to evaluate other pathologies but should not delay treatment of endometriosis. Physicians who opt for medical management should proceed with treatment promptly once other diagnoses have been reasonably ruled out. If a patient is inadequately responding to medical management, a trained physician in minimally invasive gynecology should consider laparoscopy for diagnostic and potentially therapeutic purposes.
Conclusion
This review summarizes the most recent literature recommendations for managing a patient with suspected endometriosis and the value of early diagnosis. The focus of this paper is on early recognition of disease to decrease the clinical and economic burden of delayed diagnosis and to better individualize treatment plans. Studies looking at specific combinations of symptoms in time in comparison to controls will contribute meaningfully to earlier diagnosis and management of disease.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
Dr. Tracey Juron was an independent researcher for this article. Database search and review of articles was performed by Dr. Juron. Paper was written by Dr. Juron. Dr. Seaman was a supervisor and editor of this paper with rights to authorship.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
CPP: chronic pelvic pain; SPE: superficial peritoneal endometriosis; GI: gastrointestinal; DIE: deep infiltrating endometriosis; EAP: endometriosis-associated pain; TRUS: transrectal ultrasound; TVUS: transvaginal ultrasound
| References | ▴Top |
- Hoffman BL, Schorge JO, Bradshaw KD, Halvorson LM, Schaffer JI, Corton MM. Williams gynecology (3rd ed.). McGraw Hill Professional. 2016.
- Clinical management of endometriosis: Obstetrics & gynecology. n.d.). Retrieved from: https://journals.lww.com/greenjournal/Fulltext/2018/03000/Clinical_Management_of_Endometriosis.23.aspx.
- Ghai V, Jan H, Shakir F, Haines P, Kent A. Diagnostic delay for superficial and deep endometriosis in the United Kingdom. J Obstet Gynaecol. 2020;40(1):83-89.
doi pubmed - Management of endometriosis. n.d.). Retrieved from https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2010/07/ management-of-endometriosis.
- D'Hooghe TM. Clinical relevance of the baboon as a model for the study of endometriosis. Fertil Steril. 1997;68(4):613-625.
doi - Bourdel N, Alves J, Pickering G, Ramilo I, Roman H, Canis M. Systematic review of endometriosis pain assessment: how to choose a scale? Hum Reprod Update. 2015;21(1):136-152.
doi pubmed - The endometriosis health profile. n.d.). Retrieved from https://innovation.ox.ac.uk/outcome-measures/endometriosis-health-profile-ehp/.
- Vilasagar S, Bougie O, Singh SS. A practical guide to the clinical evaluation of endometriosis-associated pelvic pain. J Minim Invasive Gynecol. 2020;27(2):270-279.
doi pubmed - Fuldeore MJ, Soliman AM. Prevalence and symptomatic burden of diagnosed endometriosis in the United States: national estimates from a cross-sectional survey of 59,411 Women. Gynecol Obstet Invest. 2017;82(5):453-461.
doi pubmed - Leonardi M, Condous G. How to perform an ultrasound to diagnose endometriosis. Australasian Journal of Ultrasound in Medicine. 2018;21(2):61-69.
doi
doi - The use of ultrasound-based 'soft markers' for the prediction of pelvic pathology in women with chronic pelvic pain—can we reduce the need for laparoscopy? (n.d.).
- Berger JP, Rhemrev J, Smeets M, Henneman O, English J, Jansen FW. Limited added value of magnetic resonance imaging after dynamic transvaginal ultrasound for preoperative staging of endometriosis in daily practice: a prospective cohort study. J Ultrasound Med. 2019;38(4):989-996.
doi pubmed - Zhang X, He T, Shen W. Comparison of physical examination, ultrasound techniques and magnetic resonance imaging for the diagnosis of deep infiltrating endometriosis: A systematic review and meta-analysis of diagnostic accuracy studies. Exp Ther Med. 2020;20(4):3208-3220.
doi pubmed - Soliman AM, Fuldeore M, Snabes MC. Factors Associated with Time to Endometriosis Diagnosis in the United States. J Womens Health (Larchmt). 2017;26(7):788-797.
doi pubmed - Surrey E, Soliman AM, Trenz H, Blauer-Peterson C, Sluis A. Impact of endometriosis diagnostic delays on healthcare resource utilization and costs. Adv Ther. 2020;37(3):1087-1099.
doi pubmed - Imaging modalities for the non-invasive diagnosis of endometriosis. n.d.). Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7100540/.
- Burton C, Iversen L, Bhattacharya S, Ayansina D, Saraswat L, Sleeman D. Pointers to earlier diagnosis of endometriosis: a nested case-control study using primary care electronic health records. Br J Gen Pract. 2017;67(665):e816-e823.
doi pubmed - Zondervan KT, Becker CM, Missmer SA. Endometriosis. N Engl J Med. 2020;382(13):1244-1256.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
