| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Original Article
Volume 10, Number 3, September 2021, pages 73-80
The Psychological Effects of the Coronavirus Disease 2019 Pandemic on Pregnant and Postpartum Women
Hana Al Sumria, d, Rahma Al Kindib, Sana Al Sumric
aDepartment of Family Medicine and Public Health, Sultan Qaboos University Hospital, PO Box 693, PC 133, Al Khuwair, Muscat, Sultanate of Oman
bDepartment of Family Medicine and Public Health, Sultan Qaboos University Hospital, PO Box 61, PC 138, Al Mouj, Almawaleh North, Muscat, Sultanate of Oman
cDepartment of Family Medicine and Public Health, Sultan Qaboos University Hospital, PO Box 50, PC 123, Al Khoud, Muscat, Sultanate of Oman
dCorresponding Author: Hana Al Sumri, Department of Family Medicine and Public Health, Sultan Qaboos University Hospital, PO Box 693, PC 133, Al Khuwair, Muscat, Sultanate of Oman
Manuscript submitted May 10, 2021, accepted June 29, 2021, published online September 28, 2021
Short title: Perinatal Mental Health and COVID-19
doi: https://doi.org/10.14740/jcgo752
| Abstract | ▴Top |
Background: There is little research available regarding the psychological effect of the coronavirus disease 2019 (COVID-19) pandemic on antenatal and postnatal women in the Middle East. This study aimed to evaluate the burden of the pandemic on the mental health of pregnant and postpartum women in Oman.
Methods: A cross-sectional study was carried out from July to December 2020 at the Sultan Qaboos University Hospital in Muscat, Oman. A previously validated Arabic version of the Depression, Anxiety, and Stress Scale was distributed to eligible participants via text message.
Results: A total of 148 women completed the questionnaire (response rate: 12.8%). Of these, 35 participants (23.6%) reported symptoms of stress, ranging in severity from mild (n = 13, 8.8%) to extremely severe (n = 4, 2.7%); and 44 women (29.7%) reported some level of anxiety, most usually of moderate severity (n = 15, 10.1%). In addition, 46 women (31.1%) reported symptoms of depression, with 16 women (10.8%) having severe or extremely severe depression. Various factors were significantly associated with anxiety and depression levels, including lack of social support due to quarantine restrictions, the presence of an elderly individual at home, and the effect of the pandemic on monthly income (P < 0.05).
Conclusions: These findings underscore the importance of finances, family, and social support on the psychological wellbeing of pregnant and postpartum Omani women during this pandemic. In future, healthcare providers should implement awareness campaigns and educational programs to provide additional support to this population group during similar health crises.
Keywords: Depression; Anxiety; Psychological stress; COVID-19; Pregnant women; Postpartum period
| Introduction | ▴Top |
Coronavirus disease 2019 (COVID-19) is a public health emergency of international concern in which a new strain of a coronavirus in the severe acute respiratory syndrome (SARS) family, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been identified as the cause of a worldwide outbreak of contagious respiratory illness. The illness was first detected in Wuhan, China, in December 2019, and has since spread rapidly around the globe [1]. While it is well-established that stressful events can have a significant impact on psychological and physical well-being, the effect of acute large-scale events such as outbreaks of infectious disease in the general population is understudied [2, 3]. As such, there is a need to better understand the psychological impact of the COVID-19 pandemic, both in the general population as well as in specific high-risk groups such as pregnant or postpartum women [4, 5].
Immunological and physiological changes during pregnancy can make pregnant women more susceptible to viral respiratory infections. Adverse pregnancy outcomes have been reported during previous outbreaks of other coronavirus infections, including SARS and Middle East respiratory syndrome [6-8]. These include increased rates of hospitalization and mechanical ventilatory support, as well maternal mortality, early miscarriage, and preterm birth [8, 9]. However, there is currently insufficient evidence to determine conclusively whether SARS-CoV-2 infection carries a higher risk of adverse reproductive outcomes, nor whether the infection can be vertically transmitted from infected mothers to their fetuses [10-12].
Even under normal circumstances, women are at greater risk of anxiety and depression during pregnancy than at any other time in their lives [13-15]. Moreover, previous research assessing the psychological effects of the 2003 SARS outbreak on pregnant women indicated that such women experienced high levels of anxiety regarding the possibility of infection [16]. The uncertainty of getting pregnant and delivering a baby during a pandemic, along with constant bombardment by daily news or social media reports with new and often negative information, have likely increased the level of stress already inherent in pregnancy [16, 17]. Apart from fear of infection and related health consequences, restrictions imposed by governments worldwide to contain the spread of disease have also hindered opportunities for regular social contact and support. Such social constraints could make expectant and new mothers more vulnerable to anxiety, stress, and depression.
Several recent reports highlight the impact of the pandemic on pregnant and postpartum women. An online survey in the USA during the pandemic lock-down period reported 11.1% and 9.9% of the sampled women meeting the criteria of both anxiety and depression respectively. The reported reasons were related to the negative economic consequences of the pandemic along with worries about women’s prenatal care, birth experience and postnatal needs [18]. Similarly, another large-scale study has also reported increased levels of anxiety/depression (31%), loneliness (53%) and post traumatic distress (43%) among 6,894 pregnant and postpartum women in 64 countries in relation to COVID-19 pandemic [19]. The reported factors were linked to receiving negative information about the pandemic from different sources many times a day, and other factors related to contracting the infection and receiving the care needed for their pregnancy and newborns in addition to worries about the long-lasting economic consequences [19].
As of the time of writing, there were 198,572 positive cases and 2,071 deaths attributable to COVID-19 in Oman, a country located in the south-eastern Arabian Peninsula [20]. However, there is a lack of COVID-19-related literature from the Middle East focusing on mental well-being during pregnancy and the postpartum period. As such, this study sought to investigate the psychological burden of the ongoing COVID-19 pandemic and its effects on levels of anxiety, stress, and depression among pregnant and postpartum women in Oman.
| Materials and Methods | ▴Top |
Study design
A cross-sectional survey was carried out over a 6-month period from July to December 2020 among Omani pregnant women and those up to 3 months postpartum who were registered at the Sultan Qaboos University Hospital (SQUH) in Muscat, Oman, between the period of March to November 2020, equivalent to the height of the COVID-19 pandemic.
Target population
The target population included all women of Omani nationality who were at any gestational age of pregnancy or up to 3 months postpartum who were registered at the antenatal clinics of SQUH between March and November 2020. The inclusion criteria comprised either primigravida or multigravida women aged 18 years or older with either spontaneous or assisted pregnancies. Among postpartum women, those who had undergone vaginal, assisted, or cesarean section deliveries were included. Women with serious medical conditions requiring frequent hospital visits and admissions and those who were more than 3 months postpartum were excluded from the study.
Sample size calculation
An online sample size calculator was used to estimate the required sample size, taking into account the estimated population of Omani pregnant and postpartum women registered at SQUH during the COVID-19 pandemic. According to unpublished hospital data, approximately 3,561 newborns were delivered at SQUH in 2020. Therefore, considering a 5% error rate and 95% confidence interval, the required sample size was calculated to be 377; however, as the estimated response rate was 30%, a total of 1,157 women were invited to participate. Unfortunately, only 148 completed questionnaires were returned, yielding a response rate of 12.8% and a margin of error of 8%.
Data collection tool
A self-administered questionnaire was used for the purpose of data collection. Information gathered included the participants’ sociodemographic characteristics, such as age, place of residence, education level, employment status, gravidity and parity, and monthly income, in addition to their living circumstances. The questionnaire also included items related to the women’s experience with the hospital’s new COVID-19-related healthcare and social distancing guidelines.
Furthermore, all respondents were asked to complete a previously validated Arabic version of the Depression, Anxiety, and Stress Scale (DASS) questionnaire [21]. The standardized DASS questionnaire includes a total of 42 items, comprising 14 items each in the depression, anxiety, and stress sub-scales. Responses were scored on a 4-point scale from 0 (“does not apply to me”) to 3 (“applies to me most of the time”) in order to determine the frequency with which the respondent had experienced each state over the past week. Scores for each DASS sub-scale were calculated by summing the scores of the items, with participants categorized into groups based on severity. Cut-off values for mild, moderate, and severe depression were 10, 14, and 21, respectively, whereas cut-off values for mild, moderate, and severe anxiety were 8, 10, and 15, respectively. For stress, cut-off values were 15, 19, and 26, respectively.
Recruitment of participants
The final version of the questionnaire was published online using SurveyMonkey® (SVMK Inc., San Mateo, CA). The contact details of eligible candidates were retrieved from the antenatal SQUH registry. An invitation to participate along with an electronic link to the questionnaire was distributed via regular text message. The aims and objectives of the study were stated clearly at the beginning of the online questionnaire and participants were informed that they had the right to withdraw at any time. A statement of confidentiality was included, and participants were clearly informed that completion of the questionnaire constituted agreement and consent to take part in the study. In addition, it was made explicitly clear that the survey would not offer any medical advice. Completed questionnaires were coded and stored in a secured database.
Statistical analysis
The Statistical Package for the Social Sciences (SPSS version 23) software program was used for data analysis (IBM Corp., Armonk, NY). Categorical data were presented as frequencies and percentages. The prevalences of the three main psychological outcomes (depression, anxiety, and stress) were categorized according to severity based on the aforementioned cut-off scores. Associations between various demographic characteristics and the severity of these psychological outcomes were analyzed using a Chi-squared test (χ2) for categorical variables. A nonparametric Fisher’s exact test (two-tailed) was used in cases wherein the expected frequency was < 5 in any of the cells. The level of statistical significance was set at P ≤ 0.05.
Ethical approval
Ethical approval for this study was obtained from the Medical Research and Ethics Committee of the College of Medicine and Health Sciences, Sultan Qaboos University (REF, NO.SQU-EC/185/2020). This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration. The participation in the study was entirely voluntary and anonymous.
| Results | ▴Top |
Demographic characteristics
A total of 148 out of 1,157 pregnant or postpartum women submitted completed questionnaires (response rate: 12.8%). The respondents ranged in age from 21 - 45 years, with a mean age of 32 ± 5 years. Most participants (n = 81, 54.7%) were 30 - 40 years old. All of the participants resided in Muscat Governorate, with the majority (n = 102, 68.9%) being located in A’Seeb Wilayat (county). More than half of the participants had a university degree (n = 94, 63.5%) and were employed (n = 102, 68.9%). Approximately three-quarters (n = 106, 71.6%) were in the initial postpartum period, with the remaining 42 women (28.4%) being in different stages of pregnancy. Of the pregnant women, most (n = 27, 64.3%) were in the third trimester (i.e., at 27 - 40 weeks of gestation, Table 1).
 Click to view | Table 1. Demographic Characteristics of the Participants (N = 148) |
Effects of the COVID-19 pandemic on health visits and social support
A total of 14 women (9.5%) had tested positive for COVID-19, while eight women (5.4%) had symptoms but had not yet been tested. Almost half of the participants (n = 71, 48.0%) reported that the outbreak had affected their decision to reduce their number of healthcare visits. The most frequently reported reason for reducing visits to health facilities was fear of catching the infection (n = 42, 28.4%). In addition, the vast majority (n = 116, 78.4%) reported that the pandemic had negatively affected their pregnancy and birth preparations, and that they missed the presence and support of family members and friends during their pregnancy or after giving birth (Table 2).
 Click to view | Table 2. Effect of the COVID-19 Pandemic on Health Visits and Social Support (N = 148) |
Effects of the COVID-19 pandemic on psychological outcomes
Based on their DASS scores, one-quarter of the participants (n = 35, 23.6%) reported symptoms of stress that ranged in severity from mild (n = 13, 8.8%) to extremely severe (n = 4, 2.7%; Fig. 1). In addition, 44 participants (29.7%) reported having anxiety ranging in severity from mild (n = 12, 8.1%) to extremely severe (n = 10, 6.8%), with the majority demonstrating moderate anxiety (n = 15, 10.1%; Fig. 2). Finally, 46 women (31.1%) reported symptoms of depression, of which eight (5.4%) cases each were severe and extremely severe (Fig 3).
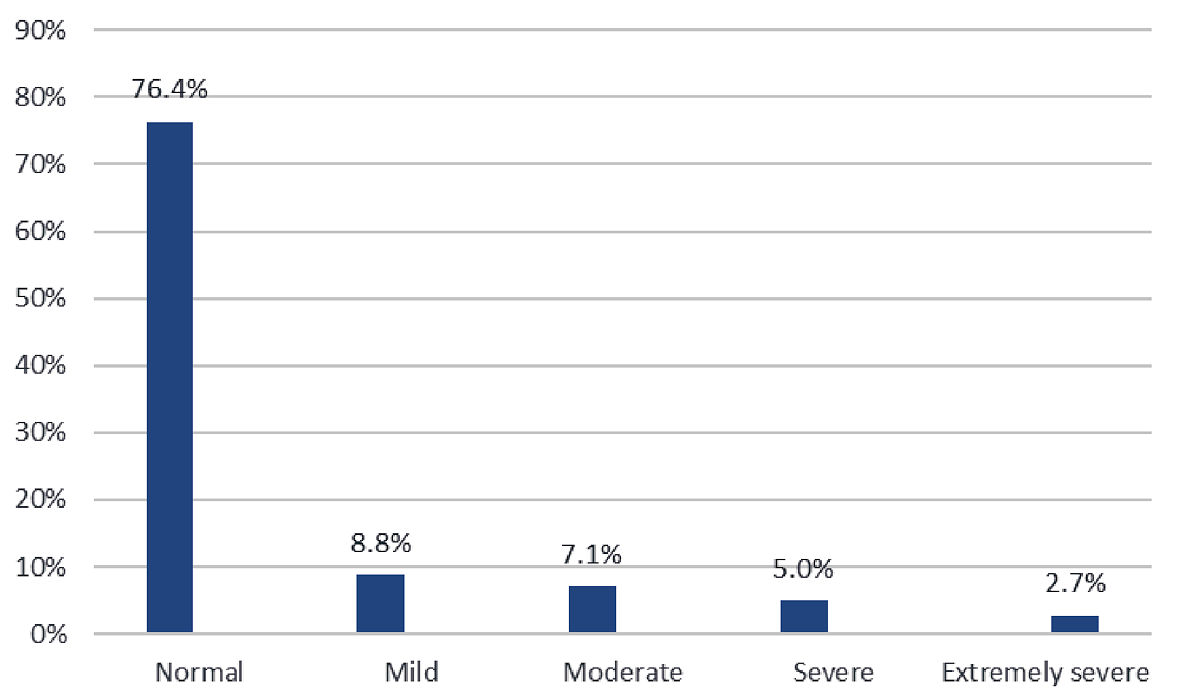 Click for large image | Figure 1. Distribution of stress symptom severity among the participants (n = 148). |
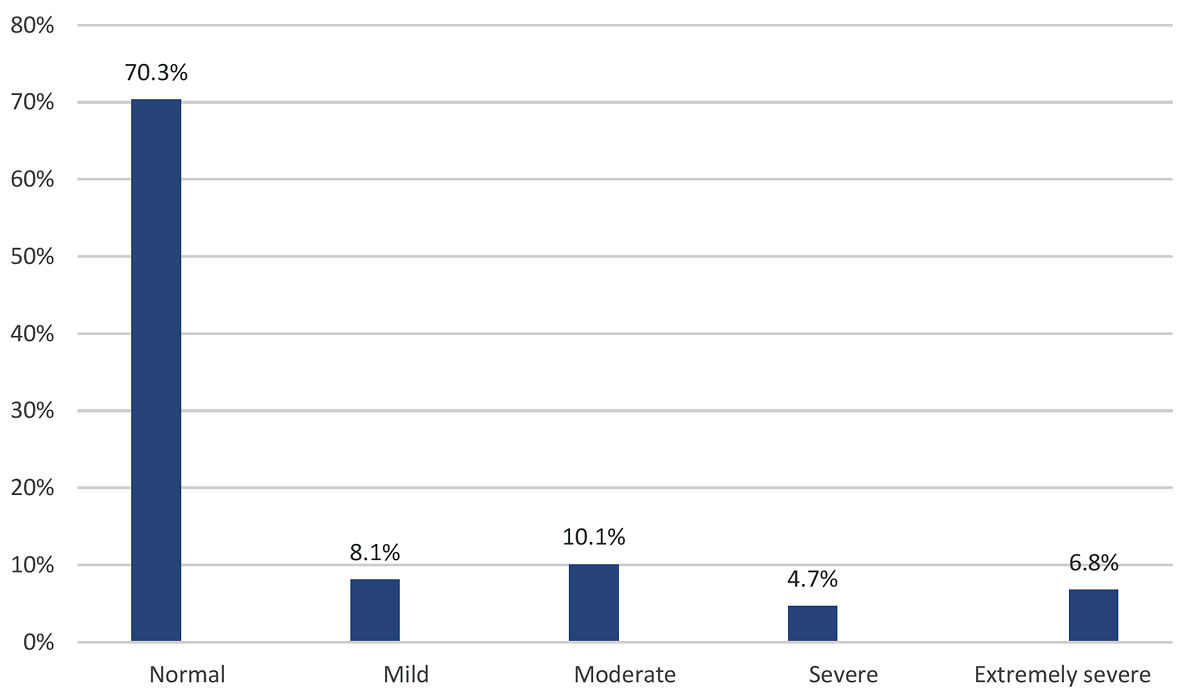 Click for large image | Figure 2. Distribution of anxiety symptom severity among the participants (n = 148). |
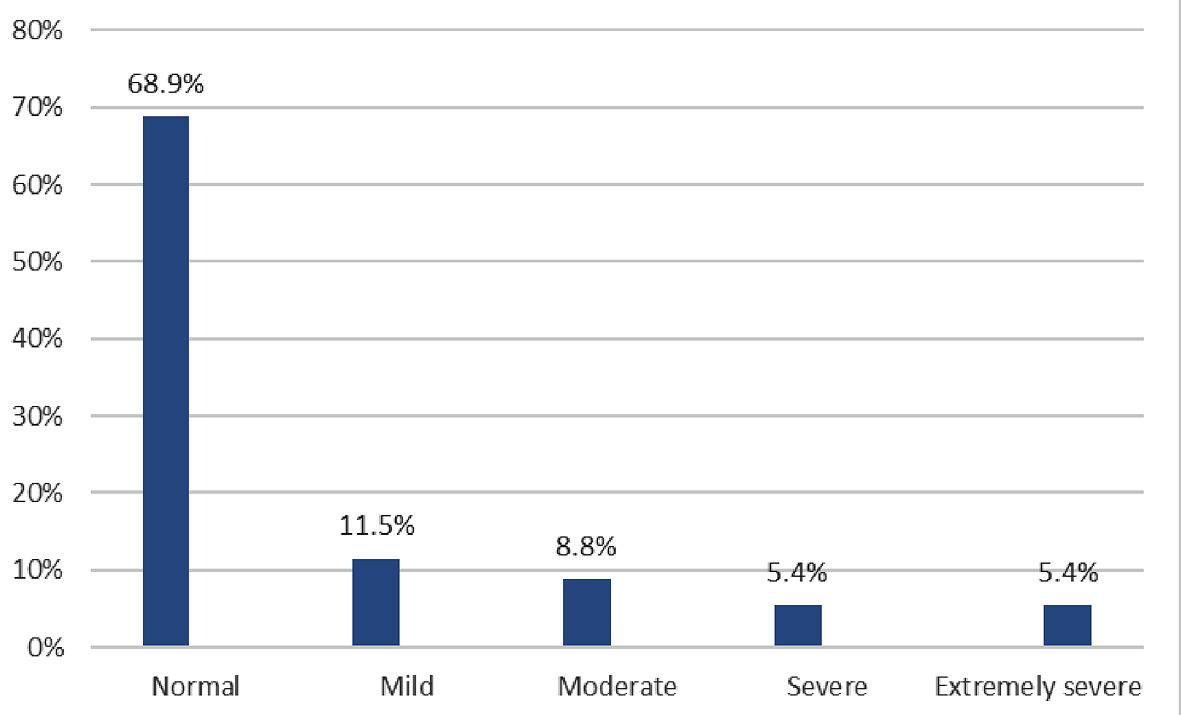 Click for large image | Figure 3. Distribution of depression symptom severity among the participants (n = 148). |
Associations between psychological outcomes and demographic characteristics
There was a statistically significant association between anxiety level and the absence of family and friends during pregnancy and after birth (P = 0.016). Similarly, the absence of social support was significantly associated with depression severity (P = 0.033). The effect of social restrictions on pregnancy and delivery preparations was significantly associated with anxiety status (P = 0.029). In addition, the presence of an elderly person in the household was significantly associated with anxiety level (P = 0.047). Levels of both anxiety (P < 0.001) and depression (P < 0.001) were significantly affected by the impact of the pandemic on monthly income. No significant associations were observed with other demographic characteristics such as age, educational level, employment status, reproductive category, or COVID-19 infection status (P > 0.05; Table 3).
 Click to view | Table 3. Associations Between Psychological Outcomes and Selected Demographic Characteristics and Participant Responses |
| Discussion | ▴Top |
Maternal depression during pregnancy can result in various adverse outcomes for both mother and fetus, including an increased risk of premature delivery and sub-optimal breastfeeding practices [22]. In addition, antenatal anxiety has been associated with various negative consequences, such as preterm birth, low birth weight and small-for-gestational age babies, and smaller head circumference [23]. These psychological conditions can have far-reaching implications for the behavior, cognition, and normal development of the child [24, 25]. In the current study, rates of psychological stress, anxiety, and depression were 23.7%, 29.7%, and 31.1%, respectively, among pregnant and postpartum women in Oman during the height of the COVID-19 pandemic. In particular, a considerable proportion of women (10.8%) demonstrated symptoms of severe or extremely severe depression, thus mandating urgent attention by health workers.
Studies conducted in other countries have reported similar results. Recent research from China and Italy reported an increase in anxiety and depression during COVID-19-related confinement among pregnant women and those in the immediate postpartum period [26, 27]. In one study, 53% of women who were in the first trimester of pregnancy during the outbreak rated the psychological impact of the COVID-19 pandemic as severe [24]. A study from Belgium reported depressive symptoms among 25.3% and 23.6% of pregnant and postpartum women, respectively, using the Edinburgh Depressive Scale and seven-item Generalized Anxiety Disorder scale (GAD-7) [28].
In particular, 14% of women in the Belgian study met the criteria for high anxiety during the COVID-19 lock-down period [26]. These findings were also in line with those reported in a national UK survey wherein the introduction of social distancing measures was found to predict unique variance in the risk of clinically relevant maternal depression (30%) and anxiety (33%) [29]. Similarly, a case-control study of postpartum women in Italy found that women who gave birth during the COVID-19 pandemic had a significantly higher rate of depressive symptoms (P < 0.001) compared to women who had given birth during the same period in 2019 [30].
Exceptional quarantine measures have been found to have negative effects on maternal emotional well-being, exacerbated by strict isolation and the women’s fear of infection due to their increased vulnerability. In Italy, concerns regarding risk of exposure combined with strict quarantine measures during the pandemic were found to adversely affect the emotional well-being of new mothers [30]. Moreover, 36% of pregnant women in a study conducted in Pakistan stated that the pandemic had had a large psychological impact on them due to their risk of exposure, increased vulnerability, and fears regarding the potential for vertical transmission to the fetus [31]. The study also reported associations between older age, low education level, and low income to rates of depression, anxiety, and sleep disturbances. Negative perceptions regarding the pandemic and fear of social stigma and discrimination towards those infected also added to the psychological burden of the women [31].
To the best of the authors’ knowledge, the present study is the first to report the psychological effect of the COVID-19 pandemic among a sample of pregnant and postpartum woman from the Middle East. Interestingly, the negative emotional effects of the pandemic were found to be significantly associated with several factors, including the women’s changed financial circumstances, new social restriction measures, and the presence of an elderly individual at home. No significant associations were found between adverse mental well-being and other demographic characteristics, such as age, education level, employment, or reproductive category. This indicates that the respondents placed a high degree of importance on their financial status and their need for social support during the pregnancy, delivery, and immediate postpartum period.
In particular, the presence of an elderly individual at home was found to be significantly associated with increased levels of anxiety. It can be assumed that these elderly individuals represented the parents or parents-in-law of the women, as such individuals commonly live with their children and spouses as a norm in traditional Omani culture. The presence of older relatives at home may be considered a source of anxiety due to such individuals’ increased risk of morbidity and mortality if they should become infected. This association further supports other findings highlighting the value of family ties and social support in Omani society [32, 33].
One limitation of this study was the low response rate (12.8%), resulting in a small sample size. This might have affected the power of the study to detect outcomes of interest. In addition, the study was conducted in a single institute; however, due to the tertiary nature of the hospital in question, some of the women were originally from different regions in Oman, thus allowing for the sample to be considered representative of the target population. Moreover, the findings of this study provide much-needed insight into the psychological well-being of a particularly vulnerable patient group. Additional awareness campaigns and educational programs are recommended to support the mental health of such individuals during similar public health crises in the future to ensure better health outcomes for mothers and their newborns.
Acknowledgments
The authors would like to thank the respondents for their participation in this study as well as the staff of the different SQUH clinics for their cooperation. Special thanks are also extended to Miss Nawf for her contribution to this work.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained prior to participation in study and approved by the Medical Research and Ethics Committee of the College of Medicine and Health Sciences, Sultan Qaboos University (REF, NO.SQU-EC/185/2020).
Author Contributions
HS conceived the original idea, supervised the project, did the data entry and statistical analysis, and wrote the manuscript; RK contributed to patient recruitment, data collecting and manuscript writing; SS contributed to patient recruitment and manuscript review. All authors discussed the results and contributed to the final manuscript jointly.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
COVID-19: coronavirus disease 2019; DASS: Depressive, Anxiety and Stress Scale; SARS: severe acute respiratory syndrome; SPSS: Statistical Package for the Social Science; SQUH: Sultan Qaboos University Hospital
| References | ▴Top |
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506.
doi - DeLongis A, Folkman S, Lazarus RS. The impact of daily stress on health and mood: psychological and social resources as mediators. J Pers Soc Psychol. 1988;54(3):486-495.
doi pubmed - Dohrenwend BS, Dohrenwend BP, editors. Stressful life events: their nature and effects. Oxford: John Wiley & Sons; 1974. p. 340-xi.
- Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatry. 2012;25(2):141-148.
doi pubmed - Martini J, Petzoldt J, Einsle F, Beesdo-Baum K, Hofler M, Wittchen HU. Risk factors and course patterns of anxiety and depressive disorders during pregnancy and after delivery: a prospective-longitudinal study. J Affect Disord. 2015;175:385-395.
doi pubmed - ANZIC Influenza Investigators and Australasian Maternity Outcomes Surveillance System. Critical illness due to 2009 A/H1N1 influenza in pregnant and postpartum women: population based cohort study. BMJ. 2010;340:c1279.
doi pubmed - Mullins E, Evans D, Viner RM, O'Brien P, Morris E. Coronavirus in pregnancy and delivery: rapid review. Ultrasound Obstet Gynecol. 2020;55(5):586-592.
doi pubmed - Alfaraj SH, Al-Tawfiq JA, Memish ZA. Middle East respiratory syndrome coronavirus (MERS-CoV) infection during pregnancy: report of two cases & review of the literature. J Microbiol Immunol Infect. 2019;52(3):501-503.
doi pubmed - Allen MC, Jones MD, Jr. Medical complications of prematurity. Obstet Gynecol. 1986;67(3):427-437.
- Knight M, Bunch K, Vousden N, Morris E, Simpson N, Gale C, O'Brien P, et al. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study. BMJ. 2020;369:m2107.
doi pubmed - Yu N, Li W, Kang Q, Xiong Z, Wang S, Lin X, Liu Y, et al. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: a retrospective, single-centre, descriptive study. Lancet Infect Dis. 2020;20(5):559-564.
doi - Rasmussen SA, Smulian JC, Lednicky JA, Wen TS, Jamieson DJ. Coronavirus Disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. 2020;222(5):415-426.
doi pubmed - Guardino CM, Schetter CD. Coping during pregnancy: a systematic review and recommendations. Health Psychol Rev. 2014;8(1):70-94.
doi pubmed - Priya A, Chaturvedi S, Bhasin SK, Bhatia MS, Radhakrishnan G. Depression, anxiety and stress among pregnant women: A community-based study. Indian J Psychiatry. 2018;60(1):151-152.
doi pubmed - Mukherjee S, Pierre-Victor D, Bahelah R, Madhivanan P. Mental health issues among pregnant women in correctional facilities: a systematic review. Women Health. 2014;54(8):816-842.
doi pubmed - Lee CH, Huang N, Chang HJ, Hsu YJ, Wang MC, Chou YJ. The immediate effects of the severe acute respiratory syndrome (SARS) epidemic on childbirth in Taiwan. BMC Public Health. 2005;5:30.
doi pubmed - Ng J, Sham A, Tang PL, Fung S. SARS: pregnant women's fears and perceptions. Br J Midwifery. 2004;12(11):698-702.
doi - Raquel E. GLK, Michal A. The disproportionate burden of the COVID-19 pandemic among pregnant black women. Psychiatry Research. 2020;293:1-18.
doi pubmed - Basu A, Kim HH, Basaldua R, Choi KW, Charron L, Kelsall N, Hernandez-Diaz S, et al. A cross-national study of factors associated with women's perinatal mental health and wellbeing during the COVID-19 pandemic. PLoS One. 2021;16(4):e0249780.
doi pubmed - Oman New Agency [Internet]. Muscat: ONA; 2021 Apr 18 [cited 2021 May 5]. 3363 more catch COVID-19 in Oman: health ministry. Available from: https://omannews.gov.om/NewsDescription/ArtMID/392/ArticleID/30900/3363-More-Catch-Covid-19-in-Oman-Health-Ministry.
- Moussa MT, Lovibond P, Laube R, Megahead HA. Psychometric properties of an arabic version of the depression anxiety stress scales (DASS). Res Soc Work Pract. 2017;27(3):375-386.
doi - Grigoriadis S, VonderPorten EH, Mamisashvili L, Tomlinson G, Dennis CL, Koren G, Steiner M, et al. The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta-analysis. J Clin Psychiatry. 2013;74(4):e321-341.
doi pubmed - Grigoriadis S, Graves L, Peer M, Mamisashvili L, Tomlinson G, Vigod SN, Dennis CL, et al. Maternal anxiety during pregnancy and the association with adverse perinatal outcomes: systematic review and meta-analysis. J Clin Psychiatry. 2018;79(5):17r12011.
doi pubmed - Kingston D, Tough S. Prenatal and postnatal maternal mental health and school-age child development: a systematic review. Matern Child Health J. 2014;18(7):1728-1741.
doi pubmed - Buss C, Davis EP, Hobel CJ, Sandman CA. Maternal pregnancy-specific anxiety is associated with child executive function at 6-9 years age. Stress. 2011;14(6):665-676.
doi pubmed - Mappa I, Distefano FA, Rizzo G. Effects of coronavirus 19 pandemic on maternal anxiety during pregnancy: a prospectic observational study. J Perinat Med. 2020;48(6):545-550.
doi pubmed - Dong H, Hu R, Lu C, Huang D, Cui D, Huang G, Zhang M. Investigation on the mental health status of pregnant women in China during the Pandemic of COVID-19. Arch Gynecol Obstet. 2021;303(2):463-469.
doi pubmed - Ceulemans M, Hompes T, Foulon V. Mental health status of pregnant and breastfeeding women during the COVID-19 pandemic: A call for action. Int J Gynaecol Obstet. 2020;151(1):146-147.
doi pubmed - Fallon V, Davies SM, Silverio SA, Jackson L, De Pascalis L, Harrold JA. Psychosocial experiences of postnatal women during the COVID-19 pandemic. A UK-wide study of prevalence rates and risk factors for clinically relevant depression and anxiety. J Psychiatr Res. 2021;136:157-166.
doi pubmed - Zanardo V, Manghina V, Giliberti L, Vettore M, Severino L, Straface G. Psychological impact of COVID-19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. Int J Gynaecol Obstet. 2020;150(2):184-188.
doi pubmed - Shahid A, Javed A, Rehman S, Tariq R, Ikram M, Suhail M. Evaluation of psychological impact, depression, and anxiety among pregnant women during the COVID-19 pandemic in Lahore, Pakistan. Int J Gynaecol Obstet. 2020;151(3):462-465.
doi pubmed - Al-Barwani TA, Albeely TS. The Omani family: strengths and challenges. Marriage Fam Rev. 2007;41(1-2):119-142.
doi - Al-Bahri A, Al-Moundhri M, Al-Mandhari Z, Al-Azri M. The role of patients' families in treatment decision-making among adult cancer patients in the Sultanate of Oman. Eur J Cancer Care (Engl). 2018;27(3):e12845.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
