| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Original Article
Volume 10, Number 3, September 2021, pages 59-66
A Randomized Controlled Trial to Evaluate the Effect of Abdominal Electrical Muscle Stimulation on Abdominal Wall Restoration in Postpartum Women
Ahmed Abdelaziza, d, Henry Ramirezb, Tracy Blusewiczc, Mickey Karrama
aDivision of Urogynecology/OBGYN Department, The Christ Hospital/University of Cincinnati, Cincinnati, OH, USA
bSouthern Oklahoma Women’s Health PC, Ardmore, OK, USA
cAdvanced Women’s Care of the Low Country, Bluffton, SC, USA
dCorresponding Author: Ahmed Abdelaziz, Division of Urogynecology/OBGYN Department, The Christ Hospital/University of Cincinnati, 2123 Auburn Ave Suite 720, Cincinnati, OH 45219, USA
Manuscript submitted June 4, 2021, accepted July 13, 2021, published online September 28, 2021
Short title: The Effect of EMS in Treating DRAM
doi: https://doi.org/10.14740/jcgo755
| Abstract | ▴Top |
Background: Diastasis of recti abdominis muscle (DRAM) is a common condition occurring postpartum and thought to be a cause for back pain and pelvic instability. Electrical muscle stimulation (EMS) had been used in abdominal muscle rehabilitation in combination with exercises in DRAM. This study looks at the effect of EMS in treating DRAM in comparison to a control group receiving no treatment.
Methods: This is a prospective randomized clinical trial. A total of 51 patients were included in the study, including group A (28 patients) that was treated with EMS, and a control group B (23 patients) that did not receive any treatment. Pre-treatment baseline, 1-, 3-, and 6-month follow-up data were collected. Results were evaluated through ultrasound measurements of inter-rectal distance (IRD), investigator assessments, patient subjective improvement and satisfaction and Pelvic Floor Distress Inventory (PFDI) questionnaire.
Results: Ultrasound IRD measurements demonstrated improvement from baseline to the 3-month and 6-month follow-up in the treatment group. Investigator assessment favored the treatment group with significant difference at all study points. Subjective assessments by patients demonstrated a significant difference between the two groups at 1-month while continued to show improvement at 3- and 6-months follow-up. PFDI questionnaire favored the treatment group over the control group in three PFDI subscales at all study points. Progress of the EMS effect over time was shown.
Conclusions: The current study supports potential efficacy of the EMS device as a stand- alone treatment modality for the improvement of DRAM in postpartum women.
Keywords: Abdominal muscles; Back pain; Diastasis recti abdominis; Electrical muscle stimulation; Postpartum
| Introduction | ▴Top |
Diastasis of recti abdominis muscles (DRAM) is defined as a separation of the two muscle bellies of rectus abdominis [1]. DRAM occurs very commonly during pregnancy with a prevalence of 27-33.1% in the second trimester [2, 3], and up to 100% in the third trimester [4]. Postpartum DRAM can persist up to 6 month ranging in 39% to 45% of women [3, 4] even lasting up to 1 year postpartum in 33% of patients [3].
The wide range of prevalence is due to lack of standardization in the definitions used to define DRAM. Some studies have used objective measures like ultrasound criteria for diagnosis (inter-rectus space > 16 mm) [4], while others have used more clinical criteria (separation ≥ 2 finger breadths) [2, 3]. DRAM occurs during pregnancy due to hormonal changes combined with uterine growth that displace the rectus abdominis muscles; the linea alba softens resulting in separation of the muscles occur in between. The inter-recti distance (IRD) varies from 2 to 3 cm wide and 2 to 5 cm long to 20 cm wide affecting the entire length of the muscle [5]. DRAM can also occur in postmenopausal women. A study in a urogynecology population showed that 66% of patient with DRAM had pelvic floor dysfunction [6]. Risk factors for developing DRAM include high age, multiparity, cesarean section, weight gain, high birth weight, multiple pregnancy and ethnicity [7-9]. The clinical implications of DRAM are not fully appreciated, but historically patient complaints of symptoms of ventral hernia such as back pain, pelvic instability and cosmetic disfigurement [10, 11].
There is increasing focus on how women may regain abdominal strength after childbirth, with much focus on exercises and physiotherapy as the most common methods for regaining the strength [12, 13].
A recent meta-analysis on published outcomes of surgical and non-surgical treatments of DRAM noted insufficient data to support physiotherapy as a stand-alone treatment modality [11].
Electrical muscle stimulation (EMS), also known as neuromuscular electrical stimulation (NMES), is the application of an electric current to elicit a muscle contraction [14]. The principle of electrostimulation mimics the process observed during voluntary muscle contraction. The stimulator sends an electrical impulse to the nerve fibers to excite them which results in muscular contraction.
EMS application has grown significantly in recent years and has been widely used in orthopedics and physiotherapy for muscle rehabilitation, training and re-education. EMS was found to be effective for muscle strengthening in orthopedic surgery, mostly being applied to quadriceps muscle [15, 16], and in neurological rehabilitation [17, 18].
Alon et al studied the effect of EMS on abdominal muscles and found it was well tolerated and strengthened the muscles. They noted the combined use of electrical stimulation and exercise to be the most effective mode for isometric strength of the abdominal muscles [19].
Two recently published studies investigated the effect of electrical stimulation in combination with abdominal exercises on the recovery of abdominal muscle strength and reduction of DRAM in postpartum women [20, 21]; both studies noted electrical stimulation in conjugation with exercises produced better outcomes than conventional exercises alone.
These studies, however, did not have a control arm, so they could not differentiate patients who had spontaneous resolution of DRAM from those who truly benefitted from the treatment protocol.
The purpose of this study was to evaluate EMS (Evolve, InMode, Irvine, CA) as a stand-alone treatment approach for recovery of abdominal muscle strength and to compare those outcomes to a control group which was just observed for spontaneous resolution of DRAM.
| Materials and Methods | ▴Top |
Patients and study design
This was an Institutional Review Board (IRB)-approved investigational prospective randomized clinical trial. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration. Postpartum women from two clinical sites were assessed routinely during their first postpartum visit 2 weeks after delivery. Patients who met the diagnostic criteria for DRAM were offered to participate in the study. DRAM was diagnosed using the criteria proposed by Boissonnault et al [2]. All clinical examinations were performed by one physician at each clinical site. IRD was measured by palpation 4.5 cm above, and 4.5 cm below the umbilicus. The women were tested in a standardized supine crock-lying position with arms crossed over the chest. They were instructed to perform an abdominal crunch till the shoulder blades were off the bench.
Recruited subjects were randomized with 1:1 ratio to either a treatment group that was treated with the EVOLVE Tone device (InMode Corporation, Lake Forest, CA) in the abdominal area, or to a control group that did not receive any treatment but were followed in an identical fashion as the treatment group.
Inclusion criteria included postpartum women aged 18 - 45 years with clinical diastasis recti and weakness of the linea alba, body mass index (BMI) of 18.5 - 32 (normal to overweight, but not obese).
Exclusion criteria included history of other energy-based therapy within 1 year, diffuse pain syndrome or chronic pain requiring daily narcotics, active electrical implant/device in any region of the body, including pacemaker or internal defibrillator, permanent implant in the treated area, pregnancy, and breast feeding, current or history of skin cancer, severe concurrent conditions, such as cardiac disorders, sensory disturbances, epilepsy, uncontrolled hypertension, and liver or kidney diseases, history of skin disorders, bleeding coagulopathies, impaired immune system, poorly controlled endocrine disorders, any active condition in the treatment area, any surgical procedure in the treatment area within the last months or before complete healing and any therapies or medications which may interfere with the use of the study device or compromised health as determined by the study doctor.
Study protocol included eight treatment visits once a week, and three follow-up visits at 1, 3 and 6 months post last treatment. Any adverse events were recorded.
Results were evaluated through photographs, ultrasound measurements of IRD, investigator assessments and Pelvic Floor Distress Inventory (PFDI) questionnaire.
PFDI questionnaire was included in our study since pelvic floor muscles and abdominal muscles function synergistically, we want to investigate how the effect of decreased abdominal muscles function through diastasis recti would affect the function of pelvic muscle.
Baseline and follow-up photographs were obtained, using consistent camera and subject placement settings with a digital imaging system.
The subjects underwent ultrasound and/or caliper measurements to evaluate IRD. Subjects assumed a supported and relaxed crook-lying position. Subjects were asked to relax their abdominal muscles and the transducer was placed perpendicular to the linea alba, above the umbilicus (midway between the umbilicus and the xiphoid process). Focus and depth were adjusted to visualize the medial aspects of both recti. The hyperechoic connective tissues with the hypoechoic rectus abdominis muscles were identified to measure the IRD at the end of a normal expiration with the automatic ruler to the nearest 0.1 cm.
Subjects’ diastasis recti condition was classified as mild, moderate or severe based on classification proposed by Ranney [22]. An observed separation of < 3 cm between the rectus muscles was labeled mild diastasis, 3 - 5 cm separation moderate diastasis, and more than 5 cm severe diastasis.
The IRD distance was measured in each visit. In addition to the above measurements, the study investigators rated the improvement levels according to a scale with score 0 for no improvement, 1 mild improvement, 2 moderate improvement, 3 marked improvement, and 4 significantly marked improvement. This was based solely on a subjective assessment by the physician performing the exam.
Subjects also rated the improvement levels according to the same scale used by study investigators. Subjects also rated their satisfaction level according to a scale with very dissatisfied -2, dissatisfied -1, neutral 0, satisfied 1, and very satisfied 2.
The PFDI-20 (short version) was used both as a symptom inventory and a measure of the degree of bother and distress (quality-of-life) caused by pelvic floor symptoms [23, 24]. This is a valid and reliable condition-specific quality-of-life questionnaire for women with disorders of the pelvic floor including urinary incontinence, pelvic organ prolapsed and fecal incontinence.
Safety of the device was evaluated by assessing the incidence, severity and persistence of adverse events, if any, occurring during the study period.
Device and treatment
The EVOLVE system Tone applicator (InMode Corporation, Lake Forest, CA) is an EMS device suitable for the treatment of skeletal muscle. EMS stimulates the muscles and assists in strengthening, training and recovering of muscles such as abdominal muscles for improved strength and endurance.
The Tone hands-free applicator (Fig. 1) is designed to deliver electrical stimulation to skeletal muscles leading to supraphysiologic contraction frequency and strength. The Tone applicators are applied to the skin surface using a belt.
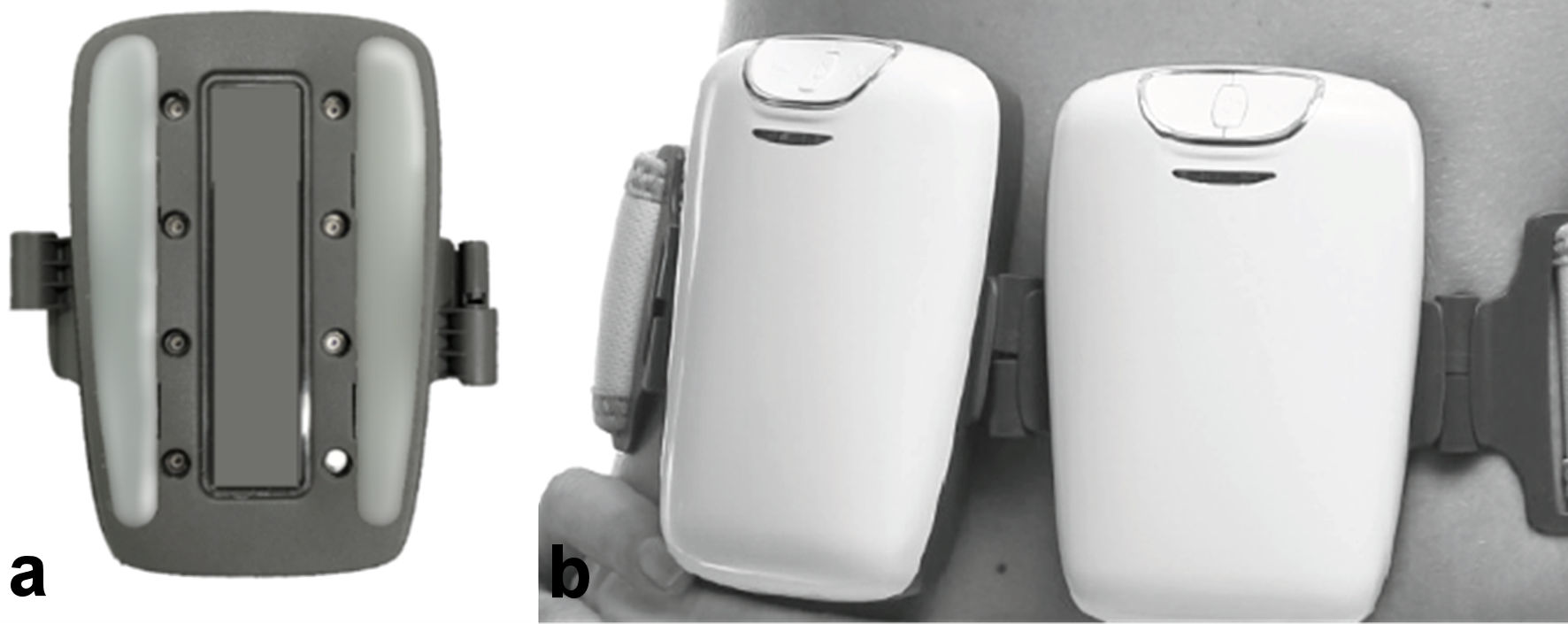 Click for large image | Figure 1. The Tone applicator. (a) Electrodes side of 1 unit. (b) Tone units on a belt attached to the abdomen. |
The EMS system enables individual adjustment of parameters such as intensity level, pulse width and frequency to achieve maximum efficiency, safety and comfort for each patient.
The two large rectangular electrodes used for the electrical stimulation were applied on the treatment area over water-based ultrasonic gel, bilaterally to the rectus abdominis. The electrodes were fixed in their position with belt. Intensity was increased gradually until a visible muscle contraction was observed, without affecting subject’s comfort. The subjects were instructed to relax their abdominal muscles during EMS application. Treatment duration was 15 - 30 min according to subject’s condition, comfort and tolerance.
| Results | ▴Top |
A total of 60 patients met the inclusion criteria and agreed to participate in the study. Thirty patients were enrolled in each arm. Two patients were lost to follow-up in the treatment arm and seven patients were lost to follow-up in the control arm; data were available at 6-months follow-up on 28 patients treated with EMS and 23 patients followed for spontaneous resolution of DRAM. The average age was 29 and BMI was 27 for both groups.
Measurements were captured at every patient visit; analyses were conducted at four time points: 1) baseline; 2) 1-month follow-up; 3) 3-month follow-up; and 4) 6-month follow-up. Measurements included IRD (with head titled ultrasound), investigator assessment of improvement, subject assessment of improvement and the PFDI (split among three subscales).
The ultrasound, investigator assessment and subject improvement scores were utilized for analysis purposes. The 20 PFDI items were collapsed (averaged) into three distinct subscales. The first subscale was comprised of the first six items Pelvic Organ Prolapse Distress Inventory-6 (POPDI-6), the second subscale was comprised of the next eight items Colorectal-Anal Distress Inventory-8 (CRADI-8), and the third subscale was comprised of the last six items Urinary Distress Inventory-6 (UDI-6). While the data do allow themselves to be analyzed as a between- and within-subjects design (i.e., a repeated measures analysis of variance (ANOVA) with treatment group serving as a fixed factor), given the sample size; and for ease of interpretation, univariate, one-way ANOVA tests were conducted comparing the two groups at each time point individually. Therefore, for variables with baseline measures (the ultrasound measurements), the baseline measurements were subtracted from the 1-month, 3-month, and 6-month measurements for each patient, and univariate, one-way ANOVA test were likewise computed on the differenced scores.
There were no significant demographic differences noted between the two groups (Table 1).
 Click to view | Table 1. Demographics of Patients |
Ultrasound measurements of the IRD did not differ from baseline to 1 month; however there was a significant improvement in the treatment arm at 3-month follow-up (P = 0.6), and the baseline to 6-month follow-up scores, while still quite different favoring the treatment group but dropping in statistical significance (P = 0.18; Table 2, Fig. 2).
 Click to view | Table 2. IRD Ultrasound Measurements |
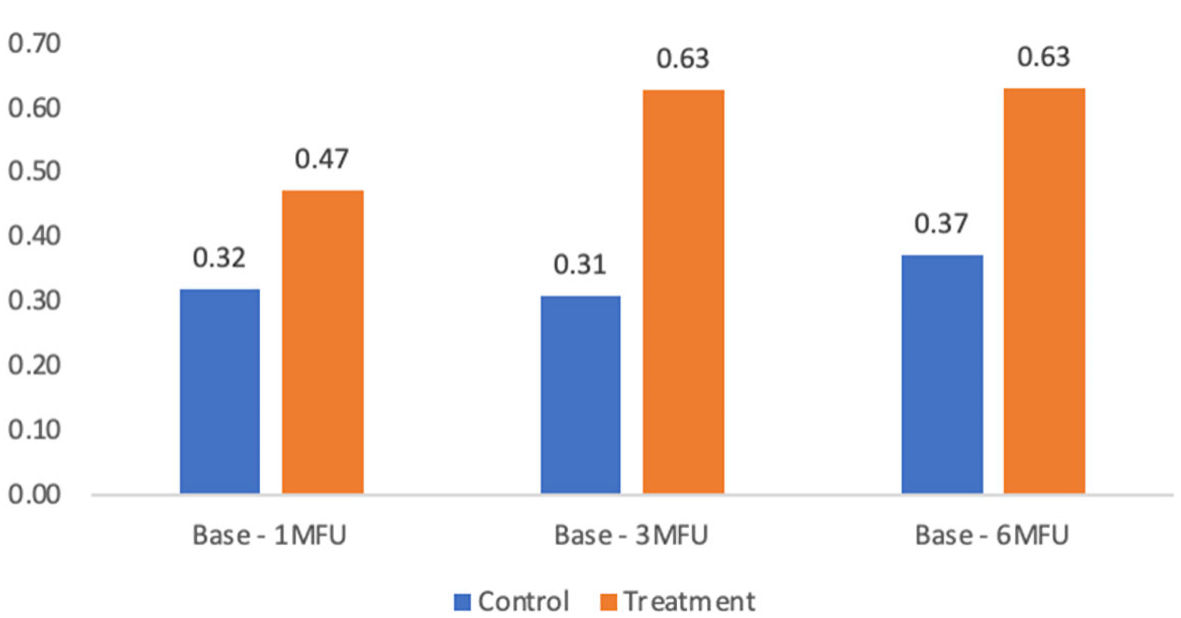 Click for large image | Figure 2. IRD baseline to 1-, 3-, and 6-month follow-ups (MFU). IRD: inter-rectal distance. |
The investigator assessments of improvement scores were compared for the two groups and noted significant improvement in the treatment group at 1-month, 3-month and 6-months (Table 3, Fig. 3).
 Click to view | Table 3. Investigator Improvement Assessment (1-, 3-, and 6-Month Follow-Ups) |
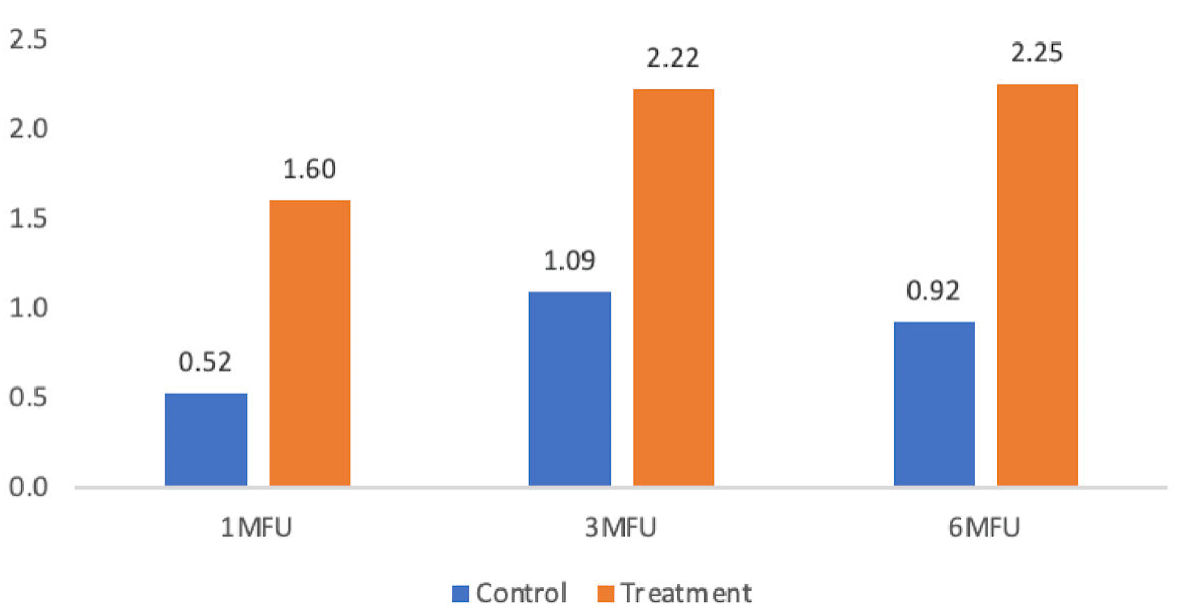 Click for large image | Figure 3. Investigator improvement: 1-, 3-, and 6-month follow-ups (MFU). |
Subject assessments of improvement scores also were different between groups at 1-month follow-up; however, that difference was noted not to be significant at the 3-month follow-up or 6-month follow-up (Table 4, Fig. 4).
 Click to view | Table 4. Subject Improvement Assessment (1-, 3-, and 6-Month Follow-Ups) |
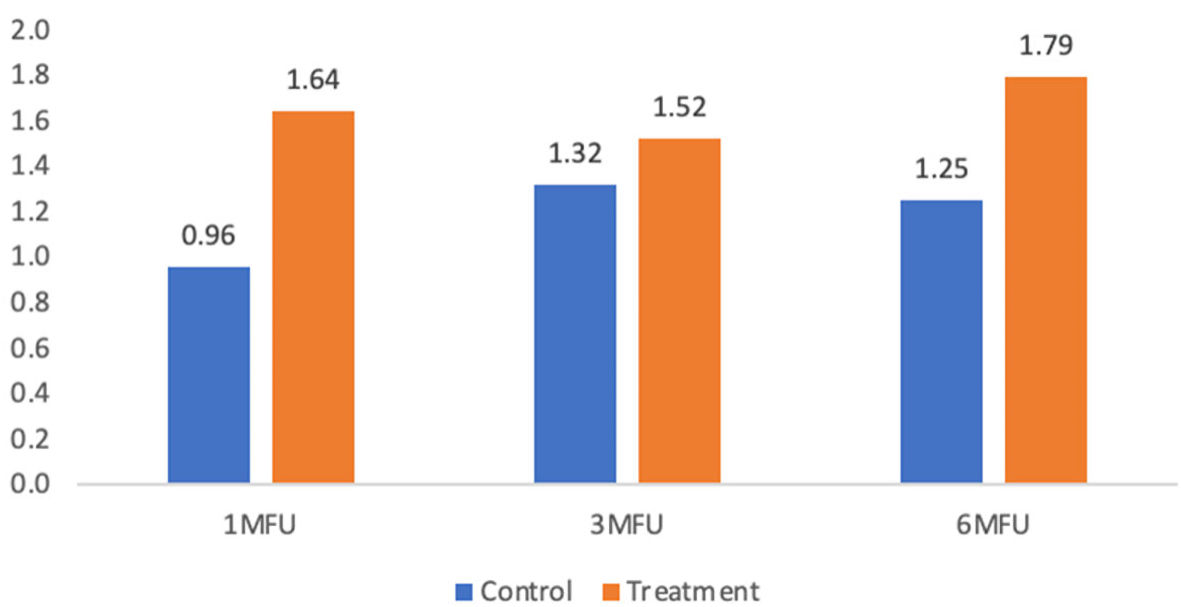 Click for large image | Figure 4. Subject improvement: 1-, 3-, and 6-month follow-ups (MFU). |
For the PFDI subscales, at the 1-month follow-up, the treatment group had significantly lower scores (thus, improved scores) compared to the control group for the first, second, and third PFDI subscales with statistical significance value in the first and second subset. These improvements in the treatment group persisted through the 3- and 6-months follow-up visits (Table 5, Fig. 5).
 Click to view | Table 5. PFDI Subscales 1 - 3 (1-, 3-, and 6-Month Follow-Ups) |
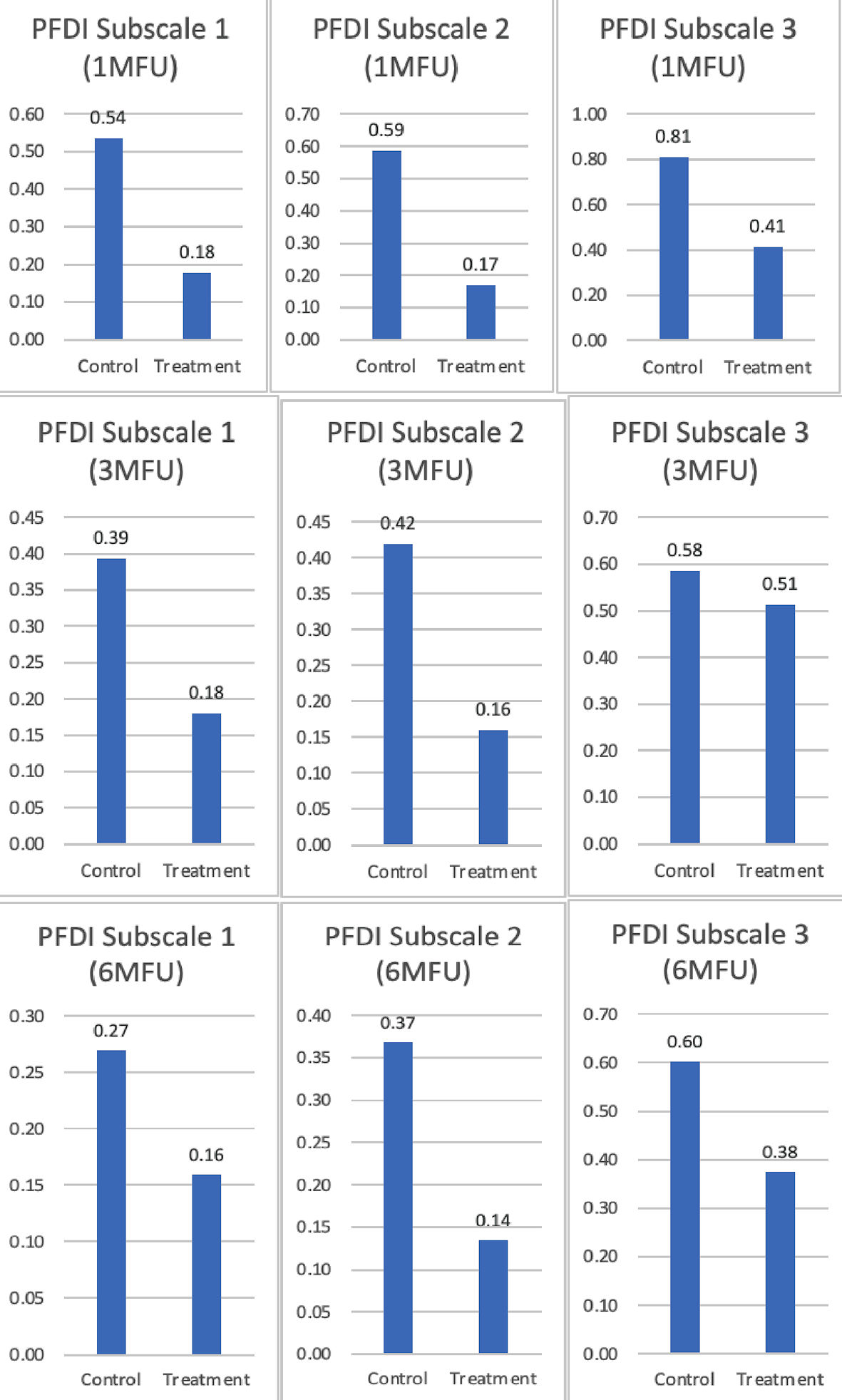 Click for large image | Figure 5. Pelvic Floor Distress Inventory (PFDI) subscales 1 - 3 (1-, 3-, and 6-month follow-ups (MFU)). |
| Discussion | ▴Top |
When contemplating non-surgical treatment for DRAM, it is important to determine if the treatment is truly working or if positive results are simply due to the spontaneous resolution of DRAM, which we knew occur approximately in 70% of women. This is the first study in which a control arm was included to better assess the true impact of the treatment arm.
The data collected during the study demonstrate a potential benefit of the EMS Tone procedure, as detailed by a series of comparisons made between the control group and the treatment group. The IRD ultrasound procedure demonstrated improvement from baseline to the 3- and 6-month follow-up in the treatment group compared to the control group. Moreover, the investigator assessments of improvement scores were better at the 1-, 3-, and 6-month follow-up for the treatment group compared to the control group. Subject improvement assessment scores were higher for the treatment group compared to the control group consistently over the 6-month period though it did not reach statistical significance. Subject improvement needs to be interpreted with care due to inherent bias and thus not very reliable. All three of the PFDI subscale scores were better for the treatment group compared to the control group at 1-, 3- and 6-month follow-up.
The strength of this study is that it is the first study to assess EMS effect on DRAM in comparison to a control group, with relative long-term follow-up of the patients up to 6 months. We used different outcomes for assessment including subjective assessment by the patient and the investigator and objective assessment as the IRD and PFDI questionnaire for more validity of the results. Finally, this is the first prospective study to assess the relationship between DRAM and pelvic floor dysfunction. The limitations of the study are that it was not blinded, so there is always a potential for bias by the patient and the physician; also the study was not powered to statistically show a difference between the two groups, so statistical outcomes need to be evaluated with caution. More studies are needed with more patients recruited to be able to show whether there is real statistical difference that can be detected between both groups.
Conclusions
EMS can potentially be of a benefit in treating DRAM compared to natural healing. The effect is more evident in the first month postpartum, and decreases with time confirming that overtime natural healing will significantly improve this condition. Potential clinical significance is seen with using EMS in pelvic floor dysfunction; however more specific tailored studies are needed to substantiate this finding.
Acknowledgments
None to declare.
Financial Disclosure
The study was funded by InMode.
Conflict of Interest
Ahmed Abdelaziz MD has no competing interest, personal financial interest, no funding from any organization that may gain or lose financially from publication of the article, and is not employed or has not been employed by an organization that may gain or lose financially from publication of the article. Henry Ramirez MD is a consultant and speaker for InMode. Tracy Blusewicz MD is a consultant and speaker for InMode. Mickey Karram MD is a consultant for InMode, Viveve and Cynosure.
Informed Consent
The informed consents were obtained.
Author Contributions
Ahmed Abdelaziz MD contributed to drafting the work, revising it and writing the manuscript. Tracy Blusewicz MD contributed to design of the work, analysis and interpretation of data for the work. Henry Ramirez MD contributed to design of the work, analysis and interpretation of data for the work. Mickey Karram MD contributed to revising it critically for important intellectual content and final approval of the version to be published.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Taber's Cyclopedic Medical Dictionary - Donald Venes - Google Books. https://books.google.com/books?hl=en&lr=&id=OA37DQAAQBAJ&oi=fnd&pg=PR1&ots=R_0u_e3-hD&sig=39_BTayHFizp36px6ByzBGspJtU#v=onepage&q&f=false. Accessed Nov 20, 2020.
- Boissonnault JS, Blaschak MJ. Incidence of diastasis recti abdominis during the childbearing year. Phys Ther. 1988;68(7):1082-1086.
doi pubmed - Sperstad JB, Tennfjord MK, Hilde G, Ellstrom-Engh M, Bo K. Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med. 2016;50(17):1092-1096.
doi pubmed - Fernandes da Mota PG, Pascoal AG, Carita AI, Bo K. Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Man Ther. 2015;20(1):200-205.
doi pubmed - Polden M MJ. Physiotherapy in obstetrics and gynaecology. Oxford: Butterworth Heinemann. 1990.
- Spitznagle TM, Leong FC, Van Dillen LR. Prevalence of diastasis recti abdominis in a urogynecological patient population. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(3):321-328.
doi pubmed - Candido G, Lo T, Janssen PA. Risk factors for diastasis of the recti abdominis. J Assoc Chart Physiother Womens Heal. 2005;97:49-54.
- Turan V, Colluoglu C, Turkyilmaz E, Korucuoglu U. Prevalence of diastasis recti abdominis in the population of young multiparous adults in Turkey. Ginekol Pol. 2011;82(11):817-821.
- Canada TL-P. Undefined diastasis of the recti abdominis in pregnancy: risk factors and treatment. 1999. ci.nii.ac.jp.
- Parker MA, Millar LA, Dugan SA. Diastasis rectus abdominis and lumbo-pelvic pain and dysfunction-are they related? J Womens Health Phys Therap. 2009;33:15-22.
doi - Mommers EHH, Ponten JEH, Al Omar AK, de Vries Reilingh TS, Bouvy ND, Nienhuijs SW. The general surgeon's perspective of rectus diastasis. A systematic review of treatment options. Surg Endosc. 2017;31(12):4934-4949.
doi pubmed - Benjamin DR, van de Water AT, Peiris CL. Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy. 2014;100(1):1-8.
doi pubmed - Michalska A, Rokita W, Wolder D, Pogorzelska J, Kaczmarczyk K. Diastasis recti abdominis - a review of treatment methods. Ginekol Pol. 2018;89(2):97-101.
doi pubmed - Durmus D, Akyol Y, Alayli G, Tander B, Zahiroglu Y, Canturk F. Effects of electrical stimulation program on trunk muscle strength, functional capacity, quality of life, and depression in the patients with low back pain: a randomized controlled trial. Rheumatol Int. 2009;29(8):947-954.
doi pubmed - Stevens-Lapsley JE, Balter JE, Wolfe P, Eckhoff DG, Kohrt WM. Early neuromuscular electrical stimulation to improve quadriceps muscle strength after total knee arthroplasty: a randomized controlled trial. Phys Ther. 2012;92(2):210-226.
doi pubmed - Walls RJ, McHugh G, O'Gorman DJ, Moyna NM, O'Byrne JM. Effects of preoperative neuromuscular electrical stimulation on quadriceps strength and functional recovery in total knee arthroplasty. A pilot study. BMC Musculoskelet Disord. 2010;11:119.
doi pubmed - Yun GJ, Chun MH, Park JY, Kim BR. The synergic effects of mirror therapy and neuromuscular electrical stimulation for hand function in stroke patients. Ann Rehabil Med. 2011;35(3):316-321.
doi pubmed - Guan Y, Wacnik PW, Yang F, Carteret AF, Chung CY, Meyer RA, Raja SN. Spinal cord stimulation-induced analgesia: electrical stimulation of dorsal column and dorsal roots attenuates dorsal horn neuronal excitability in neuropathic rats. Anesthesiology. 2010;113(6):1392-1405.
doi pubmed - Alon G, McCombe SA, Koutsantonis S, Stumphauzer LJ, Burgwin KC, Parent MM, Bosworth RA. Comparison of the effects of electrical stimulation and exercise on abdominal musculature. J Orthop Sports Phys Ther. 1987;8(12):567-573.
doi pubmed - Lalingkar RA, Gosavi PM, Jagtap VK, Yadav TS. Effect of electrical stimulation followed by exercises in postnatal diastasis recti abdominis. Int J Heal Sci Res. 2019;9:88.
- Kamel DM, Yousif AM. Neuromuscular electrical stimulation and strength recovery of postnatal diastasis recti abdominis muscles. Ann Rehabil Med. 2017;41(3):465-474.
doi pubmed - Ranney B. Diastasis recti and umbilical hernia causes, recognition and repair. S D J Med. 1990;43(10):5-8.
- Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193(1):103-113.
doi pubmed - Crosby RD, Kolotkin RL, Williams GR. Defining clinically meaningful change in health-related quality of life. J Clin Epidemiol. 2003;56(5):395-407.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
