| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Original Article
Volume 11, Number 3, September 2022, pages 75-85
A Novel Approach in Management of Placenta Accreta Spectrum Disorders: A Single-Center Surgical Experience From Vietnam
Xuan Trang Thi Phama, Anh Dinh Bao Vuonga, Lan Ngoc Vuongb, Phuc Nhon Nguyena, c
aDepartment of High-Risk Pregnancy, Tu Du Hospital, Ho Chi Minh City, Vietnam
bDepartment of Obstetrics and Gynecology, Ho Chi Minh University of Medicine and Pharmacy, Ho Chi Minh City, Vietnam
cCorresponding Author: Phuc Nhon Nguyen, Department of High-Risk Pregnancy, Tu Du Hospital, Pham Ngu Lao Ward, District 1, Ho Chi Minh City 730000, Vietnam
Manuscript submitted June 8, 2022, accepted August 11, 2022, published online September 30, 2022
Short title: Novel Approach in Management of PASD
doi: https://doi.org/10.14740/jcgo812
This article has been retracted due to conflict of authors.
| Abstract | ▴Top |
Background: Placenta accreta spectrum disorder (PASD) is the leading cause which results in highly maternal mortality during pregnancy. Although hysterectomy has been the gold standard for PASD, recent data, together with our experience, suggest that conservative management might be better; and thus, we here attempted to determine this.
Methods: A retrospective observational study enrolled 65 patients at the Tu Du Hospital in Vietnam between January 2017 and December 2018. This study included all pregnant women above 28 weeks of gestational age, who had undergone cesarean delivery due to PASD diagnosed preoperatively by ultrasound or upon laparotomy. Additionally, all patients who desired uterine preservation underwent uterine conservative surgery, avoiding hysterectomy.
Results: Overall, the rate of successful preservation was 93.8%. Other main parameters evaluated included average operative blood loss of 987 mL, mean blood transfusion of 831 ± 672 mL; mean operative time of 135 ± 31 min, and average postoperative time of 5.79 days. Postoperative complications happened in six out of 65 cases due to intraoperative bleeding and postoperative infection, requiring peripartum hysterectomy in four patients.
Conclusions: Uterine conservative surgery was associated with less operative blood loss and blood transfusion amount. Its success rate of preservative method was approximately 94% in our study. Thus, this method can be acceptable in PASD management. Further studies might be necessary to evaluate the long-term effects of this method in PASD management.
Keywords: Blood transfusion; Cesarean delivery; Conservative surgery; Obstetric hemorrhage; Placenta accreta spectrum; Maternal-fetal medicine
| Introduction | ▴Top |
Placenta accreta spectrum disorder (PASD) refers to an obstetrical challenge in pregnant women’ health care worldwide. According to the histopathological aspect, based on chorionic villus infiltration into the myometrial uterine wall, PASD includes placenta accreta, placenta increta and placenta percreta [1]. Globally, the incidence of PASD occurs rarely after 1:1,000 deliveries and was reported based on case reports or by case series. The number of placenta accreta spectrum cases increased by 2.1% every quarter year from 0.27% to 0.32% [2, 3]. However, this substantial morbidity has been increased robustly with the high rates of cesarean delivery worldwide [4].
Especially, this obstetric complication often causes a higher rate of adverse outcomes for the mother and the baby in low/middle-income countries (LMICs) such as Vietnam. Generally, antenatal diagnosis may be missed because the limitation of imaging modalities in some countries with low-resource settings and in the group of patients without risk factors. Hence, the diagnostic inspection upon laparotomy leads to the difficulty for the obstetrician without previous multidisciplinary preparation. In result, the mandatory choice is hysterectomy due to uncontrolled blood loss, particularly regardless of the morbidly adherent placenta. However, this inappropriate management causes many controversial consequences for the young female such as psychological issues, life’s quality, and loss of fertility [5]. Furthermore, hysterectomy may damage the pelvic floor function and cause a profound impact on sexual dysfunction in future [6].
Therefore, parallel with the development of imaging technology that helps to diagnose early PASD, the fundamental role of surgery is also essential. The advanced trend in PASD management is conservative surgery and preventing catastrophic blood loss [7]. In fact, we have many reliable methods to prevent massive postpartum hemorrhage (PPH) and approach to conservative treatment such as internal iliac artery ligation, leaving the placenta completely or partially in situ with or without selective arterial embolization, the stepwise cesarean delivery technique or modified Triple P procedure (perioperative ultrasound, pelvic vascularization using internal iliac artery balloon catheter, placental non-separation with myometrial excision) [5]. In 2020, Elkhouly et al mentioned a new technique by clamping bilateral uterine arteries below the placental bed after broad ligament opening by round ligament division and gentle downward dissection of vesical from myometrial tissues from the lateral aspect toward the trigone of bladder in management of PASD [8].
Nevertheless, some complications have been reported regarding of above-mentioned methods if leaving the placenta in situ. Moreover, this management needs long-term follow-up, and the success rate remains still low and cesarean hysterectomy is often required as the last option for life-saving surgery. Similarly, internal iliac artery ligation or Triple P procedure is often associated with complications including adjacent organ damage, impacts on ovarian reserve, and requires complicated technique [9]. In 2015, El Gelany et al described a therapeutic method of cervical inversion as a natural tamponade, which was potentially effective in preventing exceeding blood loss up to 95% of cases (38 out of 40 cases). Whereas, this study included only placenta previa and accreta, without description of cases of placenta percreta [10]. In 2017, Polat et al [1] reported on double uterine incision technique in 12 pregnant women compared to a single uterine incision in 10 women with placenta percreta. In the double uterine incision group, hysterectomy was avoided in 11/12 cases; however, this study with a small sample size did not describe the exact blood loss amount. Until now, some reports also mentioned this effective technique in preserving the uterus compared to single uterine incision, but uterine myometrial quality in the next pregnancy due to double uterine scar is still not studied currently [11]. Recently, Paily et al reported a new operative technique using a novel dissection-free aorta clamp in managing PASD in low-resource settings; however, the sample size is small, and this method is needed to be performed by experienced obstetrician-gynecologists [12].
At our tertiary hospital, we manage about 250 cases in relation to PASD each year. Before 2015, we performed cesarean hysterectomy without placental remove due to exceeding postpartum hemorrhage in almost all cases with new-formerly angiogenesis. From 2015, with the development of a multidisciplinary team including prenatal imaging diagnosis and anesthesia equipment, we did attempt to perform vascular-controlled ligation, invaded bladder dissection, and myometrial resection with placental adherent tissue [13]. In this stage, we also performed empirically hemostatic procedures including placental bed suture, uterine artery ligation, and Cho suture. Nevertheless, these procedures were not effective in almost severe PASD, thus the rate of hysterectomy and blood transfusion was still high. Beginning of 2016, we added a transverse B-Lynch suture to the myometrial resection technique in the decision of conservative management if the residual myometrium of the lower part of the uterus was more than 2 cm following the suggestion of Dr. Vuong ADB (Table 1, Figs. 1, 2a, b) [14]. On the clinical aspect, we have recognized that this option is a good choice for a patient who desires to save their uterus. Through this study, we aimed to describe several primary outcomes, to report our interesting results and shared our clinical experiences about this serious entity in PASD management.
 Click to view | Table 1. Protocol of Uterine Conservative Surgery at Tu Du Hospital |
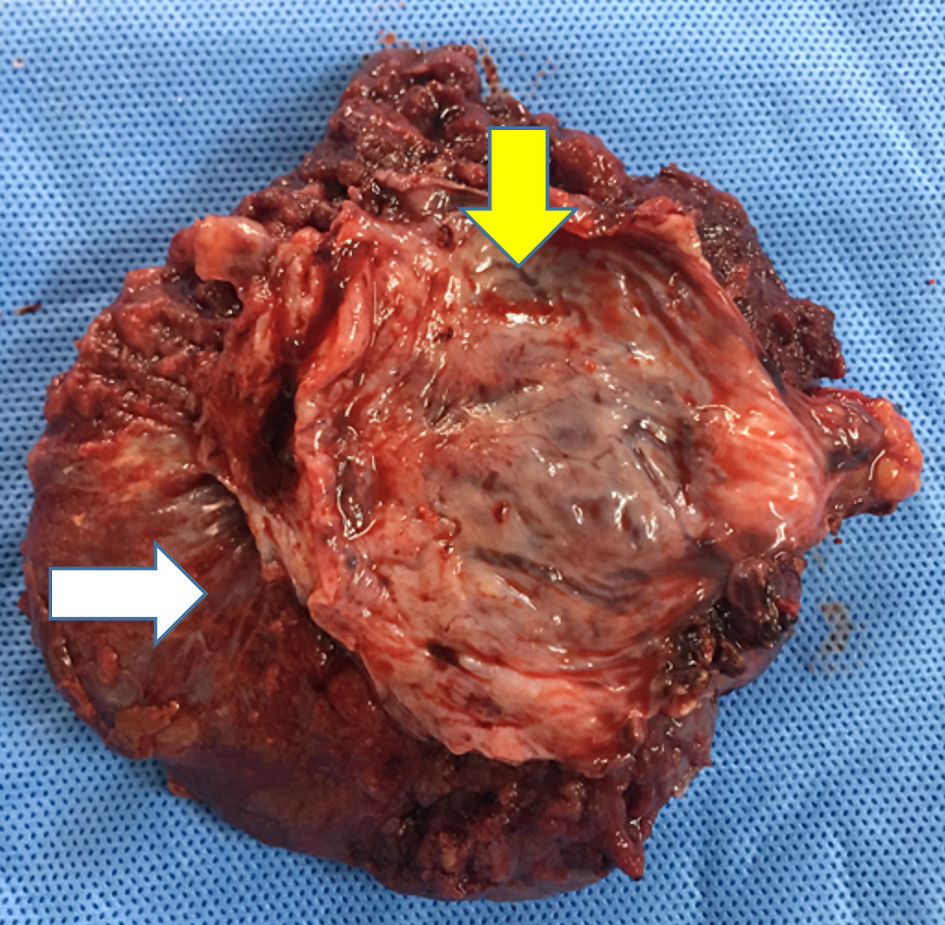 Click for large image | Figure 1. Myometrial part of uterus (yellow arrow) was removed accompanied with specimen of unseparated placenta (white arrow). |
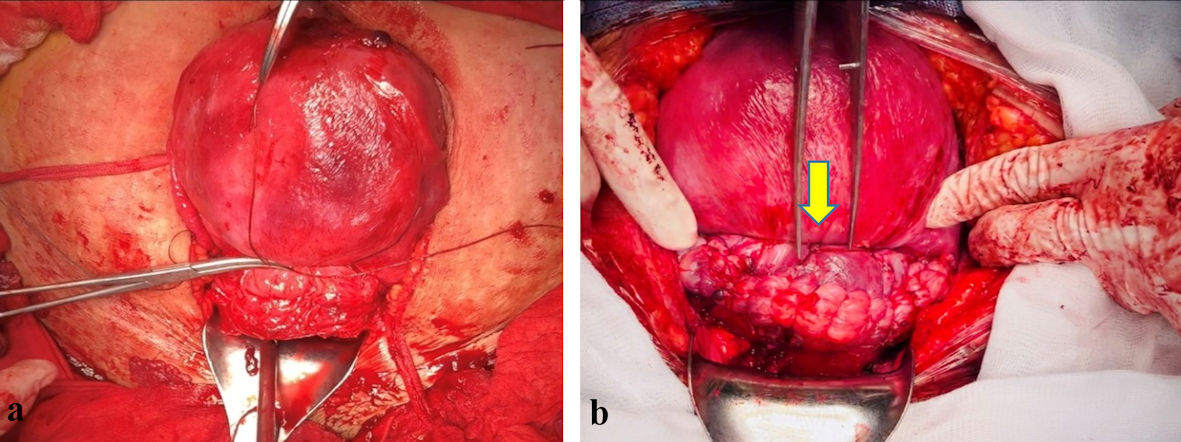 Click for large image | Figure 2. (a) Transverse B-Lynch compressive suture after uterine resection. (b) Transverse B-Lynch procedure followed by uterine closure. Conservative surgery was evaluated successfully by uterine contraction and by reducing active bleeding. |
| Materials and Methods | ▴Top |
Study design
A retrospective descriptive study was conducted at the Tu Du Hospital, Ho Chi Minh City, Vietnam, between January 2017 and December 2018. This study was accepted by Ethical Committee of Tu Du Hospital and Ho Chi Minh University of Medicine and Pharmacy, with Institutional Review Board approval number of CS/TD/18/11 and 18306-DHYD. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
The study included all pregnancies above 28 weeks of gestational age which was diagnosed with PASD. In addition, the patient desired to save their uterus and underwent uterine conservative surgery (Fig. 3).
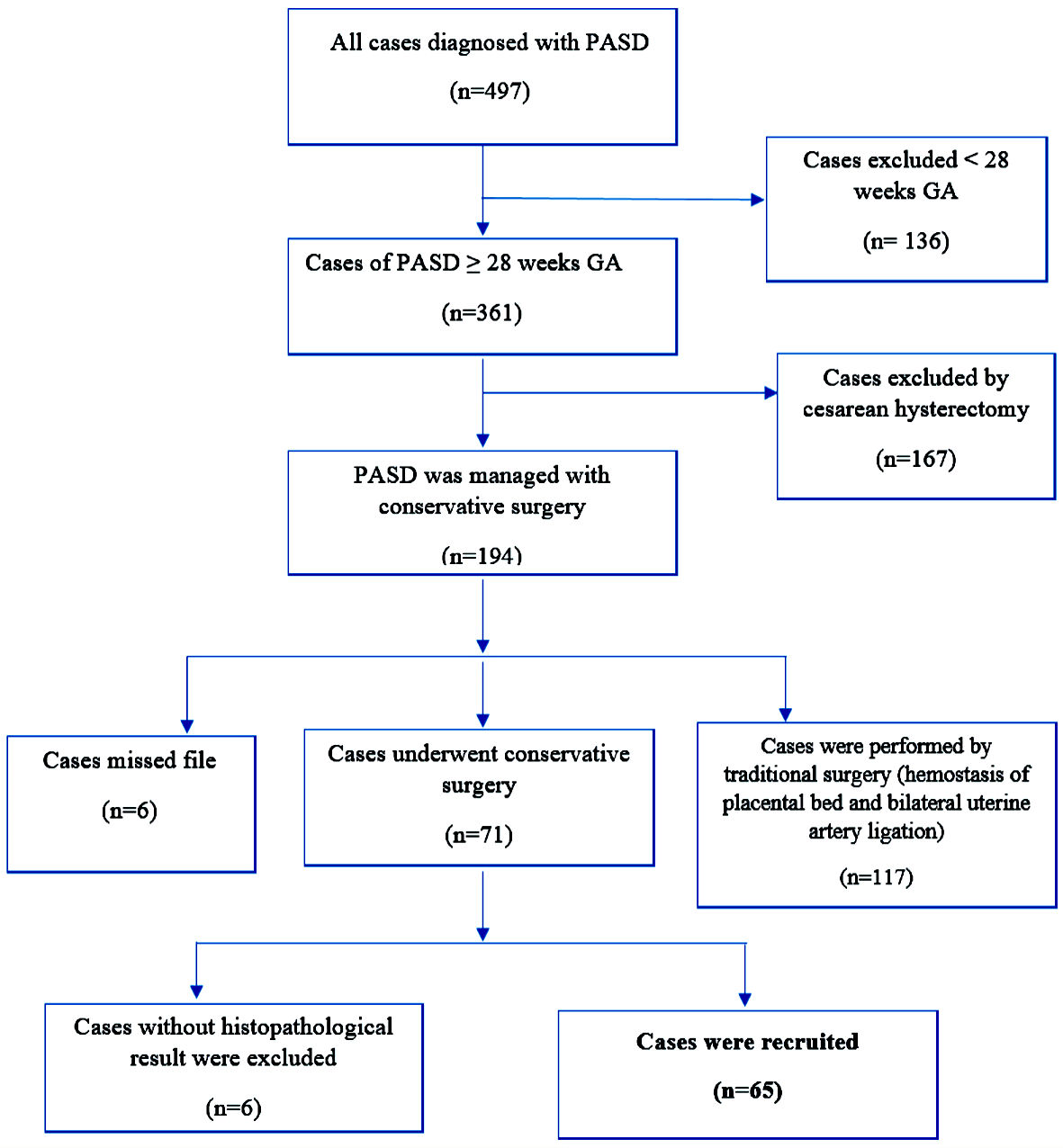 Click for large image | Figure 3. Study flow chart. PASD: placenta accreta spectrum disorder; GA: gestational age. |
Inclusion criteria
PASD was diagnosed at preoperation by ultrasound or at intraoperation by surgeon’s macroscopic observation (Fig. 4a, b). The patient underwent elective surgery or emergency surgery for cesarean delivery, underwent uterine conservative surgery following the protocol of the hospital (Table 1, Figs. 1, 2a, b) [14]. Gestational age was 28 weeks, the newborn infant could be alive.
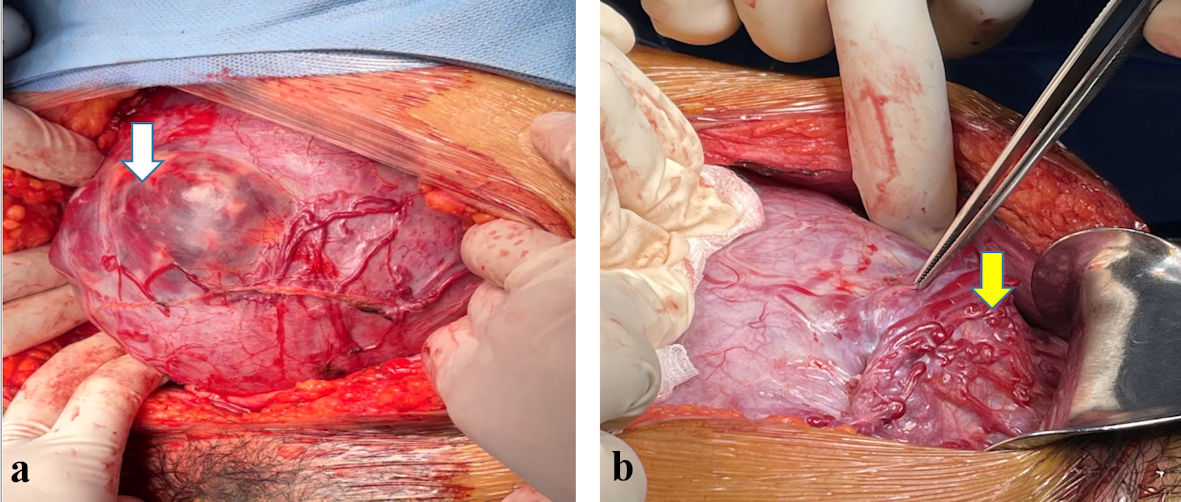 Click for large image | Figure 4. (a) Laparotomy by midline incision. Placenta was invasive deeply through myometrial layer to serosa. Placenta was visible via thin layer of uterus (white arrow). Placenta percreta was located at uterine body, closed to fundus. Newly formed blood vessels were clearly present at uterine serosa’s superficial surface. (b) Laparotomy by midline incision. Placenta was infiltrated robustly through uterine myometrium to serous membrane. Placenta percreta was located at lower segment of uterus, directed to bladder. Vascular angiogenesis developed strongly at anterior position of invasive placenta (yellow arrow). |
Exclusion criteria
Exclusion criteria are patients with missing data, cases without histopathological endpoint, and the patient who refused to participate.
Study process
Stage 1
The work of stage 1 was to filter database on computer at the Operative Department with International Classification of Diseases 10th Revision (ICD-10) code “O43.2”, and gestational age above 28 weeks.
Stage 2
We collected all patient’s files which had a diagnosis compatible with the standards of ultrasound, or whose clinical diagnosis was confirmed upon cesarean delivery by a surgeon who was trained and experienced more than 5 years in surgery for PASDs.
Standards on ultrasound by two-dimensional (2D) gray-scale/color Doppler transabdominal and transvaginal ultrasonography include: 1) loss/irregularity of the echogenic area between the uterus and placenta; 2) thinning or interruption of the hyperechogenic interface between the uterine serosa and bladder wall, uterine myometrial thickness measured below 1 cm; 3) presence of turbulent placental lacunae with high-velocity flow (> 15 cm/s); 4) hypervascularity of the uterine serosa-bladder wall interface; and 5) irregular intraplacental vascularization characterized by tortuous confluent vessels across the placental width. Diagnostic evaluation was confirmed by the presence of at least two criteria [15].
Stage 3
Stage 3 work included collecting data that meet the inclusion criteria from the patient’s file and encoding for categorical variables and continuous variables.
Continuous variables included maternal age, weight of newborn baby, blood loss amount, operation time, postpartum course (days), blood transfusion volume (mL). Blood loss amount was recorded during surgery on the operative file.
Categorical variables included type of PASD, type of surgery, maternal age group, previous cesarean scars group, gestational age group, type of placenta previa on ultrasound, insertion of JJ catheter during surgery, uterine muscular incision, bilateral uterine arteries ligation, selective ligation of vescical-uterine vessels, others hemostatic procedures, intervention of bladder repair, left partial placenta in situ, group weight of newborn infant, group Apgar score at 1 min, group Apgar score at 5 min, admission at neonatal intensive care unit (NICU), postnatal intervention, infant status during postnatal course. Measured main outcome parameters included: grade of blood loss amount, ureteric injury, tubal sterilization, operative time interval, postoperative hemorrhage, and postoperative infection.
Grade of blood loss amount was classified by American College of Obstetrician and Gynecologists (ACOG 2010): grade 0: < 500 mL, grade I: 500 - 1,000 mL, grade II: > 1,000 - 1,500 mL, grade III: > 1,500 - 2,000, and grade IV: > 2,000 - 3,000 mL. Severe blood loss following Bonnar (2000) is more than 1,500 mL which causes hypovolemic and disseminated intravascular coagulopathy [16].
Stage 4
Data were statistically analyzed by Statistical Package for the Social Sciences (SPSS) version 22.0 (SPSS Inc, Chicago, IL, USA). Value was presented with frequency (n), percentage (%), mean ± standard deviation (SD), median and interquartile range according to the distribution of data.
| Results | ▴Top |
A total of 65 placenta accreta spectrum (PAS) cases with uterine conservative surgery were encountered meeting the inclusion criteria. Among 65 patients, we performed mainly planned surgery in 59 patients with PAS in whom uterine conservative surgery was initially intended and emergency surgery in six patients. Mean age of the mother was 32.78 ± 5.19 years, and more than half of the pregnant women in our study was under 35 years old. Approximately, up to 96% of cases underwent at least one previous cesarean scar. Mean gestational age of the fetus was 35.4 ± 2.1, approximate to 85% of cesarean delivery was selective at more than 34 weeks of gestational age which depended on the type of PASD (Table 2).
 Click to view | Table 2. Characteristic of Demographic Study |
Generally, although cesarean delivery was carried out at gestational age below 37 weeks, neonatal outcomes of preterm birth were good. Overall, the average time from systemic anesthesia to fetal extraction was approximately 30 min, almost all preterm newborn babies were prevented with corticosteroids for fetal lung mature prior to cesarean delivery at least 48 h. Only six babies were transferred to a tertiary neonatal hospital due to adjusted anomalies including one case of congenital defect, one case of intestinal occlusion, three cases of gastrointestinal perforation, and one case of severe respiratory distress (Table 3).
 Click to view | Table 3. Characteristics of Neonatal Outcomes in the Study |
In fact, the total operation time was ranging from 2 to 3 h. In this study, the blood loss amount in almost all cases was reduced to less than 1,500 mL; the level of 1,500 mL can be considered as a “cut-off point” in conservative-resective surgery [9]. In this study, intraoperative blood loss was less than 1,500 mL in 51 of 65 women; however, the patients needed blood transfusion in 57 cases due to pre-and postoperative anemia. The most common complications were postoperative infection and postpartum hemorrhage. Three cases were indicated to relaparotomy and performed hysterectomy since severe infectious condition and internal bleeding due to coagulopathy. In our study, almost all patients were discharged to home after 7 days from admission (Table 4).
 Click to view | Table 4. Intraoperative and Postoperative Complications |
Even though placenta percreta occupied 28 cases and placenta increta was present in 22 cases, we attempted to preserve the uterus in nearly 94% of women (Fig. 5). Actually, the accurate prenatal diagnosis of PASD contributed to preparing a multidisciplinary team for patient care, from prenatal management to postoperative course, so the planned surgery was up to 59 out of 65 cases. Almost all the cases of emergency surgery were due to vaginal bleeding or transferred from other hospitals. Uterine conservative surgery avoided peripartum hysterectomy in 61 cases (Table 5).
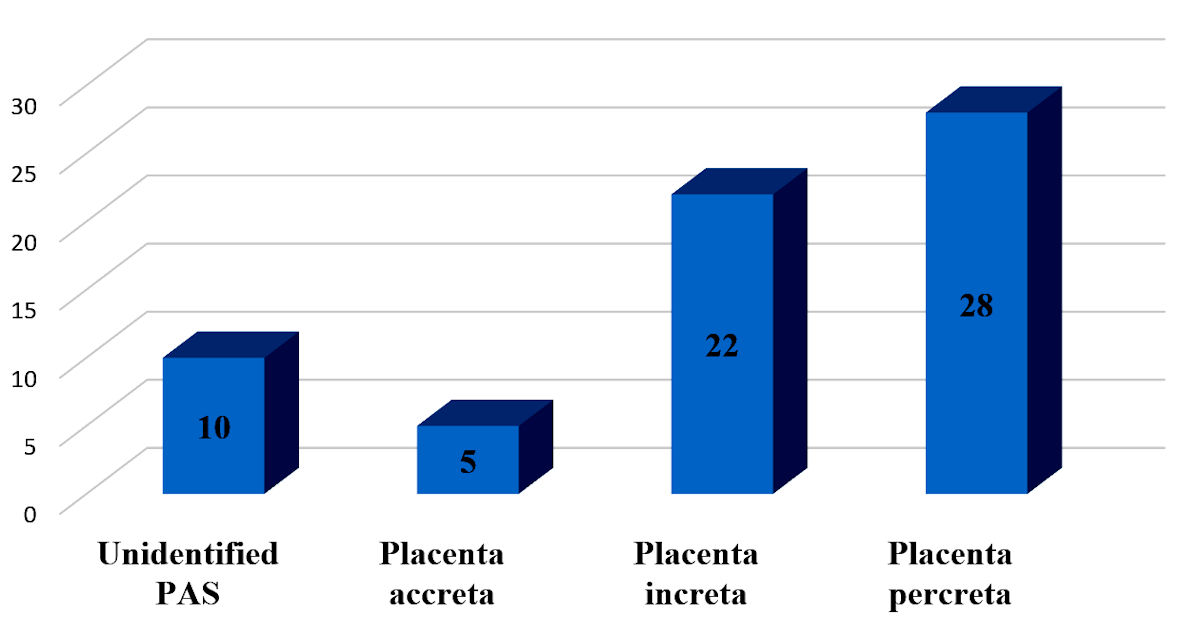 Click for large image | Figure 5. Frequency of placenta accreta spectrum disorders (PASD) in the present study. Unidentified PAS mentioned on severe invasive placenta confirmed accurately by experienced surgeon, leading to totally disappear of the myometrial layer at invasive placental location. Thus, pathologists could not conclude type of PASD in these cases. PAS: placenta accreta spectrum. |
 Click to view | Table 5. Type of PASD Related to Features of Surgery, Blood Loss Amount |
| Discussion | ▴Top |
In LMICs such as Vietnam, since interventional radiology in obstetrics has not been widely applied, thus, we mainly performed local hemostatic procedures. Worldwide, the report mentioned the preservation rate of uterine artery embolization in 76.5% of PASD cases [17]. However, its effectiveness remains controversial due to late complications [18]. Many years ago, for most of the cases of PASD, especially morbidly adherent placenta, the treatment was clearly indicated to hysterectomy without attempts to remove the placenta forcibly as the gold standard [19]. Recently, uterine conservative surgery was an alternative management, avoiding unnecessary cesarean hysterectomy in nearly 94% of cases at our tertiary hospital. However, due to the limited sample size as well as retrospective study, so further prospective cohort studies with larger samples are needed to provide robust evidence. In 2021, Ghaleb et al reported the success rate of the conservative stepwise surgical approach for the management of PASD was 80.64% (50/62 cases); and all surgical steps were similar to Palacios-Jaraquemada, except cervico-isthmic suture [20]. More recently, a multicenter study involving 587 women with PASD by Shazly et al, preserving uterus was reported in 469/587 patients (79.9%), avoiding cesarean hysterectomy for more than 100 female patients [21].
Our purpose as performing B-Lynch transverse suture was to arrest bleeding and to attach the upper and lower edges of the myometrial portion together, to avoid tension and separation during surgery. Uterine compression suture was firstly reported by B-Lynch et al in 1997. Until now, this safe procedure was demonstrated effectively in treating and in preventing uterine atony by many studies in the literature, its success rate was up to 97%, varying from 76% to 100% [14].
Generally, after fetal extraction, we administered immediately the drug to support uterine contraction such as intramuscular oxytocin 10 UI, intravenous oxytocin 40 UI, intramuscular methyl-ergometrine 0.2 mg/mL and carbetocin 100 µg/mL (Duratocin®). Additionally, we performed an exteriorization of the uterus from the abdominal cavity, bundling rapidly the para-cervical area by a 12 Fr Foley catheter to obstruct blood supply, thus leading to minimize active bleeding. After removing the placenta, the unseparated placenta was left in situ, following resection of the anterior uterine wall. We clamped the uterine wall along with the upper-lower margin, sutured two uterine angles, ligated the bilateral uterine arteries, carried out hemostasis at the placental bed site in the uterine cavity, and transverse B-Lynch compression suture. Subsequently, after all procedures including uterine reconstruction, uterine tourniquet was released, the surgeon could evaluate hemostasis, uterine contraction, and successfully confirm the preserving method.
In this study, the failure rate was 6.2% (4/65) due to intra-abdominal bleeding and postoperative infection. The method of leaving the placenta according to Teixidor et al had a failure rate of 27.2% and 40.0%, respectively [22]. Intraoperative blood loss in our study was 987 mL, less than that in the study of Wei et al (987 mL vs. 1,078 mL) with a modified 3-P cesarean section method [23]. Similarly, in the study of Zhao et al, the estimated blood loss of uterine preservation was 1,377.3 ± 605.2 mL, greater than that in our study [24]. Contributing to controlling excessive bleeding, we carefully performed bladder dissection and hemostasis of proliferative vessels prior to myometrial incision.
The number of previous cesarean scars was inversely associated with the conservative rate, adjusted odds ratio (aOR): 0.10; 95% confidence interval (CI): 0.05 - 0.2 with one previous cesarean scar; aOR: 0.02; 95% CI: 0.001 - 3.63 with five previous cesarean scars due to relating to grade of placental invasion [21]. In our study, almost all cases underwent one to two times of cesarean section (93.9%), only one case was with three times of cesarean section. This was explained that pregnant women above 35 years old with more than two times of cesarean section were recommended to undergo tubal sterilization in Vietnam.
In fact, the mean surgical time in the present study was 135 ± 31.8 min, longer than that in the study of Karaman et al (135 min vs. 120 min) and that of Zhao et al (2018) (72.3 ± 24.5 min) [24, 25]. The length of postoperative days was 5.79 days (ranged from 4.66 to 7.11 days), longer than other reports due to the difference in the condition of local health care in LMICs [21].
Preoperatively, to assure the safe surgery as part of the conservative approach, we inserted JJ catheterization in all cases with suspected severe invasion on ultrasound. This is a routine procedure at our hospital with purposes to avoid ureteric injury. According to Erfani et al, greater depth of invasion in PASD was associated with more frequent and severe adverse urologic events [26]. In our study, there was one case of unexpected injury, accounting only for 1.5%. However, this event was encountered during the preoperative JJ catheterization. In the literature, ureteral injury may happen without insertion of a ureteral catheter prior to surgery. Palacios-Jaraquemada et al reported two cases of ureteric ligation due to prompt dissection and attempt of bleeding arrest in a narrow area [13].
In all cases, we had two cases of intra-abdominal bleeding requiring relaparotomy, accounting for 3.0%, of which one case was managed with conservative treatment (by using of acid tranexamic and plasma transfusion), and another case had to remove the uterus. Despite of antibiotic broad-spectrum treatment of (cefotaxim (Cefovidi 1 g®), metronidazole 500 mg/100 mL and gentamicin 80 mg or piperacillin sodium-tazobactam sodium (Tazopelin 4.5 g®) and amikacin (Vinphacine 500 mg®), there were 6.2% (4/65 cases) of postoperative infections, all four cases were positive with Staphylococcus epidermidis, of which two cases had successful medical treatment, and two cases were indicated to hysterectomy since the infection was not response to antibiotic therapy. Whereas, compared with Palacios-Jaraquemada, our study showed lower postoperative bleeding complications and higher postoperative infections. Probably, there was a difference in the hospital’s environmental condition.
Other complications such as thrombosis was not observed in our study. In fact, we prevented this event by postoperative administration of low-molecular-weight heparin drug (enoxaparin sodium (Gemapaxane®) 4,000 UI/0.4 mL within 7 - 14 days), early movement and effort to reduce operative time. Some authors have reported arterial thrombosis during postoperative course [27].
Strengths and limitations
Tu Du Hospital is a tertiary establishment in the south of Vietnam, the number of PASD cases is enormous; therefore, surgeons are continuing to be trained and have more experience in the management of PASD. Along with the obstetrician, neonatal and anesthetic equipment have been already advanced, therefore, we could perform well cesarean delivery with placenta percreta earlier, at 32 - 34 gestational weeks, prevent progressive PASD to invade deeply into the adjacent organs, and care for preterm birth effectively. This results in preserving the uterus as the success rate of 93.8% in our study. Moreover, we identified PASD by histopathological results in almost all cases.
Nevertheless, the retrospective study did not allow all necessary data to be recorded; furthermore, there was no control group to compare the effectiveness of this method, and it had not been evaluated the fertile function of the uterus for the next pregnancy.
Conclusions
Novel approach in uterine conservative management at Tu Du Hospital required less blood loss amount and intraoperative transfusion of packed red cells. High uterine preservation surgery plays a pivotal role in saving the reproductive organ of pregnant women with PASD. Thereby, further studies are needed to accurately evaluate the success rate of uterine conservative management as well as the uterine dehiscence, fertile function, and complications in later pregnancy.
Acknowledgments
We thank the patients, who agreed to participate in our research and allowed us to publish the clinical data. The authors would like to thank Prof. Palacios Jaraquemanda who described “one-step conservative surgery”, Prof. B-Lynch who described “transverse B-Lynch technique” in the management of massive postpartum hemorrhage. The authors thank Dr. Vuong ADB who suggested to combine one-step conservative surgery and transverse B-Lynch technique in the management of PASD. The authors are also grateful to all colleagues working at the Department of High-Risk Pregnancy, Department of Imaging Diagnosis, Department of Surgery and Department of Histopathology at Tu Du Hospital. All of them contributed to providing us the pictures, participating with the operation, taking care of patients and sharing their precious experiences related to manage this clinical course with us.
Financial Disclosure
No funding was provided for the study.
Conflict of Interest
The authors declared that they have no conflict of interest.
Informed Consent
Written informed consent was obtained from the patients for publishing intraoperative pictures in the study.
Author Contributions
XTTP was responsible for conceptualization, methodology, investigation, software, data curation, and writing-original draft preparation. ADBV participated in the project administration, was also an author of the modified methods. LNV was a supervisor, revised the manuscript. Phuc Nhon Nguyen contributed to writing and editing the manuscript. All authors read and approved the final manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
LMICs: low/middle-income countries; PASD: placenta accreta spectrum disorder
| References | ▴Top |
- American College of Obstetricians Gynecologists, Society for Maternal-Fetal Medicine. Obstetric Care Consensus No. 7: Placenta Accreta Spectrum. Obstet Gynecol. 2018;132(6):e259-e275.
doi - Garmi G, Salim R. Epidemiology, etiology, diagnosis, and management of placenta accreta. Obstet Gynecol Int. 2012;2012:873929.
doi pubmed - Matsuzaki S, Mandelbaum RS, Sangara RN, McCarthy LE, Vestal NL, Klar M, Matsushima K, et al. Trends, characteristics, and outcomes of placenta accreta spectrum: a national study in the United States. Am J Obstet Gynecol. 2021;225(5):534.e1-e8.
doi pubmed - Committee on Obstetric Practice. Committee opinion no. 529: placenta accreta. Obstet Gynecol. 2012;120(1):207-211.
doi pubmed - Sentilhes L, Kayem G, Silver RM. Conservative management of placenta accreta spectrum. Clin Obstet Gynecol. 2018;61(4):783-794.
doi pubmed - Goktas SB, Gun I, Yildiz T, Sakar MN, Caglayan S. The effect of total hysterectomy on sexual function and depression. Pak J Med Sci. 2015;31(3):700-705.
- Sentilhes L, Seco A, Azria E, Beucher G, Bonnet MP, Branger B, Carbillon L, et al. Conservative management or cesarean hysterectomy for placenta accreta spectrum: the PACCRETA prospective study. Am J Obstet Gynecol. 2022;226(6):839.e1-e24.
doi pubmed - Elkhouly NI, Solyman AE, Anter ME, Sanad ZF, El Ghazaly AN, Ellakwa HE. A new conservative surgical approach for placenta accreta spectrum in a low-resource setting. J Matern Fetal Neonatal Med. 2022;35(16):3076-3082.
doi pubmed - Aryananda RA, Aditiawarman A, Gumilar KE, Wardhana MP, Akbar MIA, Cininta N, Ernawati E, et al. Uterine conservative-resective surgery for selected placenta accreta spectrum cases: Surgical-vascular control methods. Acta Obstet Gynecol Scand. 2022;101(6):639-648.
doi pubmed - El Gelany SA, Abdelraheim AR, Mohammed MM, Gad El-Rab MT, Yousef AM, Ibrahim EM, Khalifa EM. The cervix as a natural tamponade in postpartum hemorrhage caused by placenta previa and placenta previa accreta: a prospective study. BMC Pregnancy Childbirth. 2015;15:295.
doi pubmed - Polat I, Yucel B, Gedikbasi A, Aslan H, Fendal A. The effectiveness of double incision technique in uterus preserving surgery for placenta percreta. BMC Pregnancy Childbirth. 2017;17(1):129.
doi pubmed - Paily VP, Sidhik A, Girijadevi RR, Sudhamma A, Neelankavil JJ, Menon UG, George R, et al. Managing placenta accreta spectrum in low-resource settings using a novel dissection-free aorta clamp: Operative technique. Int J Gynaecol Obstet. 2022;158(2):469-475.
doi pubmed - Palacios Jaraquemada JM, Pesaresi M, Nassif JC, Hermosid S. Anterior placenta percreta: surgical approach, hemostasis and uterine repair. Acta Obstet Gynecol Scand. 2004;83(8):738-744.
doi pubmed - Balogun-Lynch C, Javaid TA. B-lynch compression suture as an alternative to paripartum hysterectomy. In: Amarin ZO, editor. Approaches to hysterectomy [Internet]. London: IntechOpen; 2015 [cited Aug 07, 2022]. Available from: https://www.intechopen.com/chapters/49153.
doi - Cali G, Giambanco L, Puccio G, Forlani F. Morbidly adherent placenta: evaluation of ultrasound diagnostic criteria and differentiation of placenta accreta from percreta. Ultrasound Obstet Gynecol. 2013;41(4):406-412.
doi pubmed - Bonnar J. Massive obstetric haemorrhage. Baillieres Best Pract Res Clin Obstet Gynaecol. 2000;14(1):1-18.
doi pubmed - Soyer P, Barat M, Loffroy R, Barral M, Dautry R, Vidal V, Pellerin O, et al. The role of interventional radiology in the management of abnormally invasive placenta: a systematic review of current evidences. Quant Imaging Med Surg. 2020;10(6):1370-1391.
doi pubmed - Matsuzaki S, Yoshino K, Endo M, Kakigano A, Takiuchi T, Kimura T. Conservative management of placenta percreta. Int J Gynaecol Obstet. 2018;140(3):299-306.
doi pubmed - Cali G. Re: Prevention of postpartum hemorrhage and hysterectomy in patients with morbidly adherent placenta: a cohort study comparing outcomes before and after introduction of the Triple-P procedure. V.Teixidor Vinas, A. M.Belli, S.Arulkumaran and E.Chandraharan. Ultrasound Obstet Gynecol. 2015;46(3):265.
doi pubmed - Ghaleb MM, Safwat S, Purohit R, Samy M. Conservative stepwise surgical approach for management of placenta previa accreta: A prospective case series study. Int J Gynaecol Obstet. 2022;157(2):383-390.
doi pubmed - Shazly SA, Hortu I, Shih JC, Melekoglu R, Fan S, Ahmed FUA, Karaman E, et al. Prediction of success of uterus-preserving management in women with placenta accreta spectrum (CON-PAS score): A multicenter international study. Int J Gynaecol Obstet. 2021;154(2):304-311.
doi pubmed - Teixidor Vinas M, Belli AM, Arulkumaran S, Chandraharan E. Prevention of postpartum hemorrhage and hysterectomy in patients with morbidly adherent placenta: a cohort study comparing outcomes before and after introduction of the Triple-P procedure. Ultrasound Obstet Gynecol. 2015;46(3):350-355.
doi pubmed - Wei Y, Cao Y, Yu Y, Wang Z. Evaluation of a modified "Triple-P" procedure in women with morbidly adherent placenta after previous caesarean section. Arch Gynecol Obstet. 2017;296(4):737-743.
doi pubmed - Zhao X, Tao Y, Du Y, Zhao L, Liu C, Zhou Y, Wei P. The application of uterine wall local resection and reconstruction to preserve the uterus for the management of morbidly adherent placenta: Case series. Taiwan J Obstet Gynecol. 2018;57(2):276-282.
doi pubmed - Karaman E, Kolusari A, Cetin O, Cim N, Alkis I, Yildizhan R, Sahin HG, et al. Local resection may be a strong alternative to cesarean hysterectomy in conservative surgical management of placenta percreta: experiences from a tertiary hospital. J Matern Fetal Neonatal Med. 2017;30(8):947-952.
doi pubmed - Erfani H, Salmanian B, Fox KA, Coburn M, Meshinchiasl N, Shamshirsaz AA, Kopkin R, et al. Urologic morbidity associated with placenta accreta spectrum surgeries: single-center experience with a multidisciplinary team. Am J Obstet Gynecol. 2022;226(2):245.e1-e5.
doi pubmed - Palacios-Jaraquemada JM, Fiorillo A, Hamer J, Martinez M, Bruno C. Placenta accreta spectrum: a hysterectomy can be prevented in almost 80% of cases using a resective-reconstructive technique. J Matern Fetal Neonatal Med. 2022;35(2):275-282.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
