| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Original Article
Volume 11, Number 3, September 2022, pages 62-68
Virtual Prenatal Care During a Pandemic: How Satisfying Is It to the Caregivers and the Patients?
Momina Zulfeena, c, Nirmala Chandrasekaranb
aPublic Health, MPH, University of York, UK
bSt Michael’s Hospital, Toronto, ON, Canada
cCorresponding Author: Momina Zulfeen, Public Health, University of York, York, UK
Manuscript submitted July 24, 2022, accepted September 3, 2022, published online September 30, 2022
Short title: Patient Satisfaction With Virtual Prenatal Care
doi: https://doi.org/10.14740/jcgo817
| Abstract | ▴Top |
Background: To inform post-pandemic obstetric care, we sought to explore the perceptions of the new virtual prenatal care model by patients and physicians.
Methods: The study is a cross-sectional survey of the patients attending the prenatal clinic and physicians during the start of the coronavirus disease 2019 (COVID-19) pandemic. Fifty-three patient-satisfaction and 14 physician-satisfaction questionnaires were collected. Scores were compared between the traditional model and the virtual care model.
Results: Mean patient satisfaction scores were significantly higher with regular visits compared to virtual visits (4.56 vs. 4.43, P = 0.023). This difference was more pronounced in women with previous poor obstetric outcomes. While women found their physicians to be friendlier on virtual visits, traditional visits allowed for easier scheduling. Differences in age, ethnicity, distance to travel and working status did not lessen the satisfaction.
Conclusions: Mothers were less satisfied with virtual prenatal care telehealth services, especially vulnerable patient populations. Special considerations may be helpful for women with previous poor obstetric outcomes.
Keywords: Virtual prenatal care; Telehealth; Tele-obstetrics; Patient satisfaction; Pandemic; Post-pandemic; Questionnaire study; Physician-satisfaction
| Introduction | ▴Top |
Restrictions during the coronavirus disease 2019 (COVID-19) pandemic necessitated a rapid adaptation to the situation. The changes that needed to be made during this evolving situation were vital to reduce the exposure to the virus, to preserve personal protective equipment (PPE), and to minimize the impact of the burden on facilities. Since the majority of our clinical workflows and health care delivery systems are designed around an in-person or face-to-face style of care, telemedicine is still new [1]. Furthermore, while the “non-essential” care can be delayed, prenatal care must continue.
Telemedicine has been around for decades [2]. It is traditionally defined as the remote provision of medical care using audio-visual technology. Varieties such as teleradiology and telepathology have been tested and are found to be successful [3]. While telemedicine has also been tried in prenatal care, it had little impact in change of care [4]. Various factors underlay this, including barriers to adapting to digital services among both patients and patient care providers, need for physical assessments, ultrasounds, and laboratory tests [5]. These barriers, to some extent, could be addressed with the spacing of visits, video meetings and at-home use of technologies such as blood pressure measuring device and smartwatches. With the lack of data about the impact of telemedicine practices on both patients and physicians, addressing these issues may be challenging.
Therefore, we aimed to conduct a survey to evaluate both patient and physician satisfaction and evaluate the limitations and barriers in virtual care.
| Materials and Methods | ▴Top |
Study design and setting
To assess the effects of virtual care on patient and physician satisfaction, we conducted a cross-sectional study in the antenatal clinics of St. Michael’s Hospital, Toronto, Canada.
A convenience-based sampling strategy was employed to recruit participants. As the estimated number of patients receiving both virtual and traditional care was around 200, which is a small population, it was agreed that all patients will be approached during the time period. We aimed to survey all patients attending at least one virtual visit during the study period and all obstetricians employed at our hospital.
Telemedicine services used at the setting included phone calls and direct video conferencing. Remote health monitoring, when used, included home or remote clinic-based health care devices where available. Figure 1 depicts our cloud-based telemedicine services. Hospital administrators employed necessary security protocols for safe and confidential teleconsultation services. Although it was actively encouraged, physicians had the autonomy of choosing virtual care.
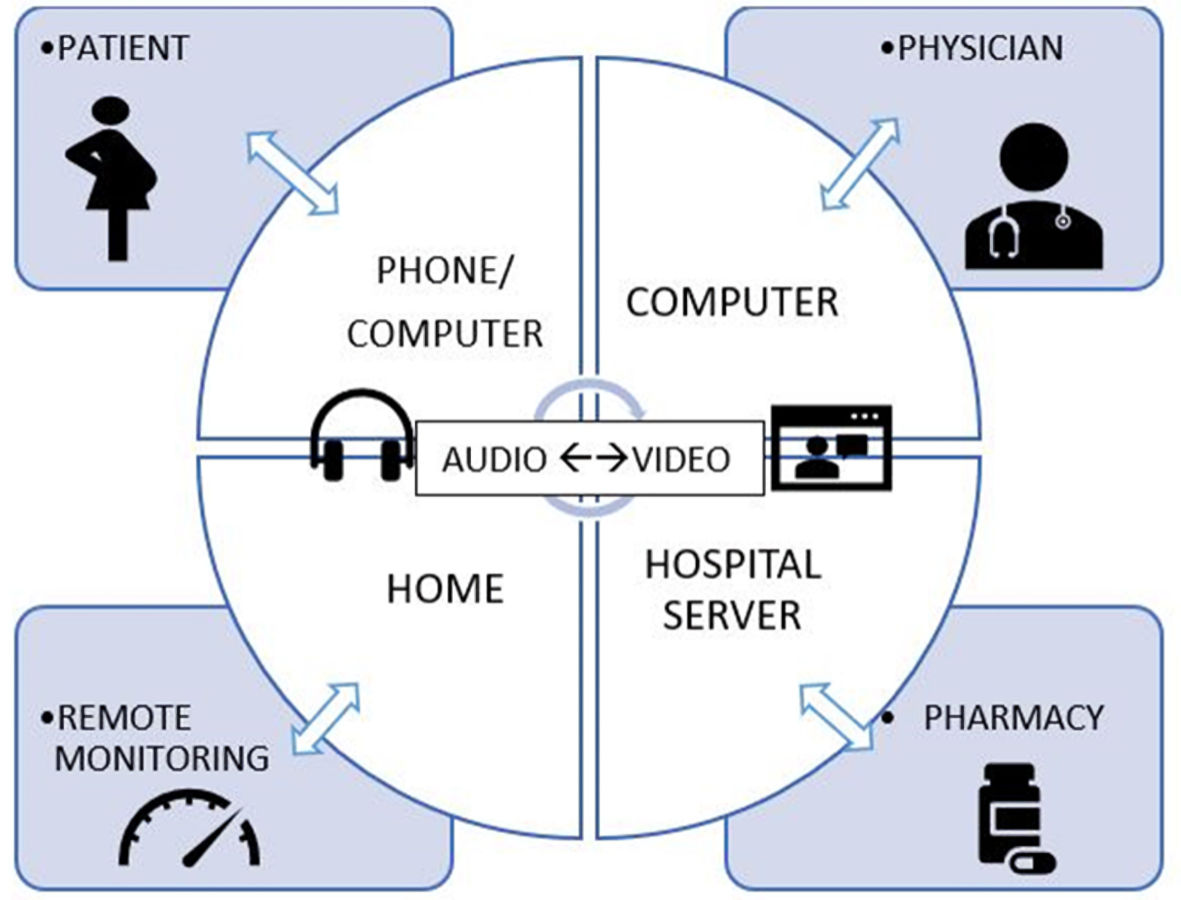 Click for large image | Figure 1. Cloud-based telemedicine services. |
Research model
The researchers recognized the need for using the appropriate survey tools for evaluation of patient and physician satisfaction. We used the previous works by Kissi et al [6] and Pflugeisen et al [7] to generate the survey questionnaires.
To understand the performance of telemedicine services among healthcare professionals, Kissi et al [6] developed a physician satisfaction survey model using the technology acceptance model (TAM) [8] framework. The researchers used the domains: perceived ease of use (PEOU), perceived usefulness (PU), individual behavioural intention (BI), actual telemedicine utilization (ATU) and user satisfaction (SE). The results from 543 participants supported their hypothesis that the PEOU and PU have a positive impact on BI, which in turn influenced ATU positively. The results also supported a positive influence of ATU on physician satisfaction (SE). “Behavioural intention” depicts physicians’ intention to either accept or reject the telemedicine services. The authors reaffirmed the need for improving BI by motivating physicians’ technology acceptance, as the physicians had enough autonomy in accepting or rejecting the telemedicine services.
Patient satisfaction
Participating women registered a significantly higher total/mean satisfaction scores with traditional visits compared to virtual visits. This difference was significant with and without technology domain. Ease of scheduling and overall satisfaction scores were also significantly higher with traditional visits, whereas “friendliness/courtesy of provider” scores were better with virtual visits.
Women with previous poor obstetric outcome reported relatively lower satisfaction scores (4.4 vs. 4.0). Demographics such as age, ethnicity, distance to travel, working status, the previous poor obstetric outcome did not seem to adversely affect the total satisfaction scores.
Physician satisfaction scores
Physicians reported an overall satisfaction score of 65.5 (36 - 89) for a maximum of 100. Demographics such as age, gender did not affect the overall satisfaction scores. However, physicians with prior experience and “frequent” use of telehealth services reported higher satisfaction scores. Due to a very small sample size, the domains did not achieve significant correlations with each other; however, PEOU correlated the most with BI (r = 0.52, P = 0.09) and SE (r = 0.48, P = 0.13).
Physician satisfaction survey
All prenatal care providers were invited to fill out a physician satisfaction survey via institutional emails. Participation was voluntary. The questionnaire was designed using physician satisfaction questionnaire by Kissi et al [6], and items were modified to fit the prenatal care construct. The questionnaire comprised of constructs PU, PEOU, BI, ATU and SE, with Likert scale questions.
Patient satisfaction survey
All patients, both low-risk and high-risk, completing at least one virtual visit and one traditional visit between March 1, 2020, to June 30, 2020, were invited to participate in a patient satisfaction survey. Research personnel identified the virtual care patients through Centricity Perinatal (CPN) database. Health care providers who are part of the patient’s circle of care would introduce the study either by phone or during a face-to-face visit. Consenting patients received the surveys through email with a link to the survey.
Surveys were designed using pre-validated questionnaires for virtual prenatal care and traditional care models by Pflugeisen et al [7]. The questionnaires were self-administrable and could be completed in less than 15 min.
Satisfaction was measured using Likert scale questions, which was divided into the domains; “scheduling”, “technology”, “provider” (or interchangeably), “patient”, “personal” and “general”. The individual domain scores thereby generate the overall satisfaction scores.
Multiple choice demographic questions will include demographics. Surveys were deidentified to preserve anonymity, and no other data were collected from physicians or patients.
Statistics
All survey-related data were entered by co-investigator into Excel sheet. Using SPSS 20 software, the categorical data were descriptively analyzed and expressed in percentages and means. Mean scores for each domain for traditional and virtual visits were compared using the t-paired test. A P value of < 0.05 was considered significant.
Ethical statement
Ethical approval was obtained from the Research and Ethics Board (REB) at St. Michael’s Hospital (REB 20-118), University of Toronto. All participants were contacted by a person from their circle of care. The study was introduced by reading out a script, thoroughly explaining the study. Survey links were provided via email, and the landing page of the survey included a digital consent. As the questionnaires had questions on the previous obstetric outcome, social work support was available. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
| Results | ▴Top |
Patient demographics
A total of 103 women agreed to receive the surveys and 100 women were approached. Three women were not approachable due to incorrect contact information. With a response rate of 53%; 53 women with a mean age of 32.7 years replied to the survey. Majority participants were Caucasian (49.1%), with 67.9% seeing the prenatal care provider for the first time. Around 17 patients had experienced previous poor obstetric outcomes in the form of miscarriages or stillbirths (Table 1).
 Click to view | Table 1. Demographics of the Participants |
The results show that the mean patient satisfaction scores were significantly higher with traditional visits compared to virtual visits (4.56 vs. 4.43, P = 0.023). Demographics such as age, ethnicity, distance to travel, working status did not seem to adversely affect the total satisfaction scores. Its worth noting that women with previous poor obstetric outcome reported relatively lower satisfaction scores (4.4 vs. 4.0) (Tables 2, 3).
 Click to view | Table 2. Mean Likert Scores of Survey Questions and Domains |
 Click to view | Table 3. Overall Domain Scores |
Physicians on the other part, reported an overall satisfaction score of 65.5 (36 - 89) for a maximum of 100. Demographics such as age, gender did not affect the overall satisfaction scores. Physicians with prior experience and “frequent” use of telehealth services reported higher satisfaction scores with telemedicine (Tables 4-6).
 Click to view | Table 4. Individual Domain and Total Scores of Physicians |
 Click to view | Table 5. Mean Difference in Total Scores According to Physician Characteristics |
 Click to view | Table 6. Correlations Among Domains, Correlation Coefficient (r) and P value (P) |
| Discussion | ▴Top |
Telemedicine services in prenatal care
Telemedicine has the potential to reduce health care costs substantially. For physicians, this could mean lesser utilization of the space, supporting personnel and time and lower exposure. For patients, this could mean reduced travel costs, work hours and so forth [3]. The benefits are abstract as the research is limited for patient-centered outcomes. There can be some perceived limitations to telehealth, including the inability to discuss sensitive topics, limited access to resources, cultural acceptance, etc.
The World Health Organization (WHO) [9] recommends at least eight contacts during the prenatal period to improve maternal and perinatal outcomes in low-risk pregnancies. A higher number of visits than this would improve maternal satisfaction. Fewer visits than these would reduce maternal satisfaction and increase perinatal mortality, with no effect on preterm births or small for gestational age (SGA) birth [10].
On March 11, the WHO characterized COVID-19 as a pandemic. Between March 12 and March 22, every Canadian province and territory had declared a state of emergency and tightened the restrictions. In mid-April 2020, public health measures, including staying home, physical distancing, and handwashing, led to a positive change [11]. Non-essential services and workplaces remained closed. In the past 6 months, we have witnessed a change in prenatal care practices, with a shift towards a virtual care model [12]. There have also been changes in prenatal screening [13] and diabetes screening [14] protocols. Although Ontario has gradually started reopening the province, these changes are likely to remain longer, aiming at a sustainable virtual care model [12, 15]. Furthermore, the attitudes of women since the COVID-19 pandemic have changed towards health care [16]. This change warrants exploring patient beliefs through the lens of pandemic and its aftereffects.
American College of Obstetricians and Gynecologists (ACOG) has made recommendations that some of the non-essential prenatal care can be virtual [17]. The ACOG [17] guidance states that “OB/Gynes and other prenatal care practitioners should also consider creating a plan to address the possibility of a decreased health care workforce, potential shortage of personal protective equipment, limited isolation rooms, and should maximize the use of telehealth across as many aspects of prenatal care as possible”. Though not widely used, the feasibility of the use of telemedicine has been established, in the context of counseling for fetal surgeries, ultrasound interpretations, genetic counseling and also the management of gestational diabetes [18, 19].
With quick adoption and acceptance of virtual care models, there is also an advocacy for telehealth post COVID-19 [9]. As the health care providers do not routinely integrate this into prenatal care, the feasibility, dependability, cost-effectiveness, and the impact on patients and healthcare providers are largely unknown [12]. A systematic review [20] looking at telehealth in obstetrics and gynecology also suggested some benefit with telehealth interventions. However, the studies have not looked at provider/physician satisfaction.
In our study, we aimed to examine the impact of virtual prenatal care on patients and physicians. The results show that the mean patient satisfaction scores were significantly higher with traditional visits compared to virtual visits. This is in contrast from earlier studies by Pflugeisen et al [7, 21], where patient satisfaction was higher with virtual prenatal care model. The authors evaluated patient satisfaction with a novel virtual obstetric care model and reported significantly higher mean satisfaction scores with the virtual-care model. There were no differences in perinatal outcomes. The patients, however, were given a choice between virtual care and traditional model. This self-selected approach may have introduced potential bias. Also, the study let the women have an electronic sphygmomanometer and handheld Doppler for self-checking. This may not be feasible on a larger scale, especially amid pandemics. Nevertheless, our results were consistent with studies evaluating patient satisfaction in non-pregnant populations [22, 23].
Our results are rather unexpected as one would expect a generational acceptance of technology given the young prenatal population that is being studied. The low scores for virtual visits despite the ease of no travel, increased access to care, decreases wait times, etc., could be because pregnant women perhaps find traditional visits more reassuring. The face-to-face contact, listening to the fetal heart rate can be emotionally gratifying to the women. This is more so for women who experienced prior adverse outcomes. There is also the additional element of providing non-verbal cues to the physicians in cases of intimate partner violence, which may not be possible with virtual visits. Our findings agree with findings from Liu et al where patients were satisfied with virtual prenatal care, however indicated a preference for in-person care under non-pandemic circumstances [24].
Physicians on the other part, reported an overall satisfaction score, though physicians with prior experience reported higher satisfaction scores. This is consistent with an earlier study [6] where physicians less familiar with telemedicine services were more likely dissatisfied.
Limitations
Although virtual care has not been satisfying to our patients, the current delivery of telemedicine services has not been time-tested. Ongoing studies [12, 25] implementing newer, more structured prenatal framework such as OB Nest [26] will likely provide insight into further planning and implementation of obstetric telehealth. Our response rates were low and may have missed vulnerable populations, especially those with poor internet access.
Conclusions
Mothers were less satisfied with virtual prenatal care compared to traditional visits. Telehealth services, especially in vulnerable patient populations, are likely suboptimal in achieving patient satisfaction. Emphasis should be laid on the ease of scheduling visits, and special considerations may be made for women with previous poor obstetric outcomes.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
Authors declare no conflict of interest.
Informed Consent
Informed consent was obtained.
Author Contributions
MZ contributed to original research, manuscript writing and submission. NC contributed to the supervision of research and manuscript writing.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Keesara S, Jonas A, Schulman K. COVID-19 and health care's digital revolution. N Engl J Med. 2020;382(23):e82.
doi pubmed - Johnson LL, Schwarz E, Rosenberg KD. The evolution of state-based dental sealant programs in oregon within the context of the state health care transformation process. J Public Health Manag Pract. 2020;26(5):461-470.
doi pubmed - Kahn JM. Virtual visits—confronting the challenges of telemedicine. N Engl J Med. 2015;372(18):1684-1685.
doi pubmed - Telemedicine and Pregnancy Care | The Henry J. Kaiser Family Foundation. https://www.kff.org/womens-health-policy/issue-brief/telemedicine-and-pregnancy-care/. Accessed April 27, 2020.
- Health Resources & Services Administration. Telehealth Programs | Official web site of the U.S. Health Resources & Services Administration. U.S. Department of Health and Human Services.
- Kissi J, Dai B, Dogbe CS, Banahene J, Ernest O. Predictive factors of physicians' satisfaction with telemedicine services acceptance. Health Informatics J. 2020;26(3):1866-1880.
doi pubmed - Pflugeisen BM, Mou J. Patient satisfaction with virtual obstetric care. Matern Child Health J. 2017;21(7):1544-1551.
doi pubmed - McCord M. Technology acceptance model. In: Handbook of Research on Electronic Surveys and Measurements. 2006.
doi - World Health Organization. WHO Recommendation on Antenatal care for positive pregnancy experience. WHO Recomm Antenatal care Posit pregnancy Exp. 2016. ISBN: 9789241549912.
- Tuncalp, Pena-Rosas JP, Lawrie T, Bucagu M, Oladapo OT, Portela A, Metin Gulmezoglu A. WHO recommendations on antenatal care for a positive pregnancy experience-going beyond survival. BJOG. 2017;124(6):860-862.
doi pubmed - Ayouni I, Maatoug J, Dhouib W, Zammit N, Fredj SB, Ghammam R, Ghannem H. Effective public health measures to mitigate the spread of COVID-19: a systematic review. BMC Public Health. 2021;21(1):1015.
doi pubmed - Fryer K, Delgado A, Foti T, Reid CN, Marshall J. Implementation of obstetric telehealth during COVID-19 and beyond. Matern Child Health J. 2020;24(9):1104-1110.
doi pubmed - Audibert F, Ouellet A, Okun N, Douglas Wilson R. Prenatal screening update during the COVID-19 pandemic.
- Yamamoto JM, Donovan LE, Feig DS, et al. Urgent update-temporary alternative screening strategy for gestational diabetes screening during the COVID-19 pandemic a joint consensus statement from the Diabetes Canada Clinical Practice Guidelines Steering Committee* and the Society of Obstetricians and Gynecologists of Canada.
- Redesigning prenatal care during the COVID-19 pandemic. https://labblog.uofmhealth.org/rounds/redesigning-prenatal-care-during-covid-19-pandemic. Accessed August 20, 2020.
- Cavaliere AF, Zaami S, Pallottini M, Perelli F, Vidiri A, Marinelli E, Straface G, et al. Flu and tdap maternal immunization hesitancy in times of COVID-19: an Italian survey on multiethnic sample. Vaccines (Basel). 2021;9(10):1107.
doi pubmed - Implementing Telehealth in Practice: ACOG Committee Opinion Summary, Number 798. Obstet Gynecol. 2020;135(2):493-494.
doi pubmed - Odibo IN, Wendel PJ, Magann EF. Telemedicine in obstetrics. Clin Obstet Gynecol. 2013;56(3):422-433.
doi pubmed - Nudell J, Slade A, Jovanovic L, Hod M. Technology and pregnancy. Int J Clin Pract Suppl. 2011;170:55-60.
doi pubmed - DeNicola N, Grossman D, Marko K, Sonalkar S, Butler Tobah YS, Ganju N, Witkop CT, et al. Telehealth interventions to improve obstetric and gynecologic health outcomes: a systematic review. Obstet Gynecol. 2020;135(2):371-382.
doi pubmed - Pflugeisen BM, McCarren C, Poore S, Carlile M, Schroeder R. Virtual Visits: Managing prenatal care with modern technology. MCN Am J Matern Child Nurs. 2016;41(1):24-30.
doi pubmed - Ayas M, Ali Al Amadi AMH, Khaled D, Alwaa AM. Impact of COVID-19 on the access to hearing health care services for children with cochlear implants: a survey of parents. F1000Res. 2020;9:690.
doi pubmed - Wolthers TO, Wolthers OD. Telephone consultation as a substitute for face-to-face consultation during the COVID-19 pandemic. Dan Med J. 2020;67(7):A04200300.
- Liu CH, Goyal D, Mittal L, Erdei C. Patient satisfaction with virtual-based prenatal care: implications after the COVID-19 pandemic. Matern Child Health J. 2021;25(11):1735-1743.
doi pubmed - Peahl AF, Smith RD, Moniz MH. Prenatal care redesign: creating flexible maternity care models through virtual care. Am J Obstet Gynecol. 2020;223(3):389.e1-e10.
doi pubmed - Bright MA, Thompson LA, Roussos-Ross D, Montoya-Williams D, Hardt N. Bridging prenatal and pediatric care: a proposed simple yet novel approach to preventing family violence. J Pediatr. 2020;224:133-136.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
