| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Original Article
Volume 12, Number 2, August 2023, pages 33-38
Bulbocavernosus Reflex as an Objective Measure of Improvement Following Directed Pelvic Floor Rehabilitation for Treatment of Urinary Incontinence
Ashley E. Hiltona, f, b, Zachary Selzlera, Prachi Kasara, Heather Barbiera, c, Chad L. Crossd, Michael Bradleye, Adam V. Levya
aDepartment of Obstetrics and Gynecology, University of Nevada Las Vegas, School of Medicine, Las Vegas, NV 89102, USA
bDepartment of Obstetrics and Gynecology, University of Colorado School of Medicine, Aurora, CO 80045, USA
cDepartment of Gynecology Surgery & Obstetrics, Uniformed Services University of the Health Sciences, Bethesda, MD 20814, USA
dDepartment of Epidemiology & Biostatistics, University of Nevada Las Vegas School of Public Health, Las Vegas, NV 89119-3063, USA
eNew Image Medical, Inc., Las Vegas, NV 89121, USA
fCorresponding Author: Ashley Hilton, Department of Obstetrics and Gynecology, University of Colorado School of Medicine, Aurora, CO 80045, USA
Manuscript submitted March 22, 2023, accepted April 29, 2023, published online June 21, 2023
Short title: Bulbocavernosus Reflex for Treatment of UI
doi: https://doi.org/10.14740/jcgo871
| Abstract | ▴Top |
Background: Abnormal bulbocavernosus reflex latency and subsequent improvement is an objective measure of improvement after directed pelvic floor physical therapy. The aim of the study was to utilize bulbocavernosus reflex testing as an objective measure of pelvic floor rehabilitation success in the treatment of urinary incontinence (UI) in a large screened population.
Methods: This was a retrospective case series of 95 women with UI who were found to have abnormal bulbocavernosus reflex tests (UroVal System), then treated with guided pelvic floor exercise program for 6 - 12 weeks that included electrical stimulation. Charts were reviewed for demographics, prior treatment, baseline and post-treatment bulbocavernosus reflex latencies, pre- and post-treatment anal manometry, number of daily incontinence episodes, pad counts, patient perception of improvement using satisfaction at the conclusion and at 6 - 24 months post-treatment. Pre-to-post mean differences were calculated using paired t-tests with 95% bootstrap confidence based on 10,000 permutations.
Results: Significant differences were found in pre- and post-treatment bulbocavernosus reflex latency (85.0 vs. 35.4 ms, P < 0.001), anal manometry (40.2 vs. 56.4 ms, P < 0.001), pad counts (1.0 vs. 0.1 per day, P < 0.001), and incontinence episodes (1.8 vs. < 1.0 per day, P < 0.001). Perceived improvement was 80% (standard deviation (SD) 17.8%) at the conclusion of treatment. At 6 to 24 months post-treatment, satisfaction persisted at 93% (SD 12.5%).
Conclusions: The bulbocavernosus reflex is an effective objective screening tool to establish pelvic neuromuscular dysfunction. Abnormal bulbocavernosus reflex latency and subsequent improvement after guided pelvic floor rehabilitation is an objective measure that can be used in conjunction with the patient’s subjective improvement.
Keywords: Bulbocavernosus; Pelvic floor physical therapy; Urinary incontinence; Bulbocavernosus reflex
| Introduction | ▴Top |
Urinary incontinence (UI) is a common and frequently under-reported problem leading to significant impacts on quality-of-life measures [1, 2]. It affects up to 52% of women in the United States alone [3] and both the International Continence Society (ICS) and the International Urogynecological Association (IUGA) recommend pelvic floor muscle (PFM) therapy as a first-line treatment [1-6]. However, both the optimal methods for quantification of PFM strength and the modalities in pelvic floor rehabilitation (PFR) remain unclear [3, 4]. Interpretation of many studies is limited by poor design, insufficient sample size, and lack of data in female subjects leading to the inability to make definitive, objective conclusions regarding particular treatment benefits. Supervised treatment appears to be superior to individual non-supervised therapy [4]. However, randomized controlled trials also show conflicting results when comparing adjunct outpatient treatment such as biofeedback in addition to guided PFM training [5-7]. In our institution, we performed baseline and post-treatment bulbocavernosus reflex testing using a device (UroVal, BRS: Bulbocavernosus Reflex System) followed by electrical stimulation and supervised guided pelvic floor exercise by technicians trained specifically for this instruction. A smaller study published in 2018 demonstrated a high degree of effectiveness using similar techniques including electrical stimulation but was under-powered [8]. Our study expands on this earlier study and incorporates the BRS latency as an objective method to measure of pelvic neuromuscular function and improvement in a larger population of patients with UI [9, 10].
| Materials and Methods | ▴Top |
We conducted a retrospective case series of women diagnosed with UI at the Pelvic Floor Rehabilitation Center at Women’s Health Center, Department of OB/GYN, UNLV School of Medicine, Las Vegas Nevada between June 2015 and September 2019. Patients were screened for pelvic floor dysfunction via a non-validated screening questionnaire. Women with UI based on the questionnaire were then evaluated with the bulbocavernosus reflex using electromyography (BRS). This provides an objective measure, in milliseconds of latency, of the sacral nerve/anal sphincter complex to respond to clitoral and/or vulvar stimulation. We used the UroVal Bulbocavernosus Reflex System (UroVal BRS, Uroval Inc., Manhattan, KS) to obtain these measurements. Figure 1 shows normal and abnormal BRS latency examples. Clinically, this reflex is painlessly elicited by mechanical stimulation of the clitoris and/or vulva, in response to which there is anal sphincteric contaction [11]. In our study, BRS was considered abnormal with a latency of more than 45 ms. This cutoff was chosen based on well-established data in women where the upper limits of latency ranged from 40 to 46.8 ms [12-14]. Weekly treatments of guided pelvic floor training in conjunction with 200 Hz electrical stimulation and peak anal manometry were completed for a planned 8-week treatment course. Charts were reviewed for age, parity, mode of delivery, comorbidities, body mass index, smoking status, pelvic organ prolapse (POP), medical therapy, and prior treatment (Table 1). Baseline and post-treatment measures of BRS latency, peak anal manometry (mm Hg), number of UI episodes, and number of pads used were recorded. The primary outcome was BRS latency. Secondary outcomes were the changes in UI episodes per day, pads used, peak anal manometry measurements in mm Hg, and overall satisfaction. This study was approved by the UNLV Institutional Review Board. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
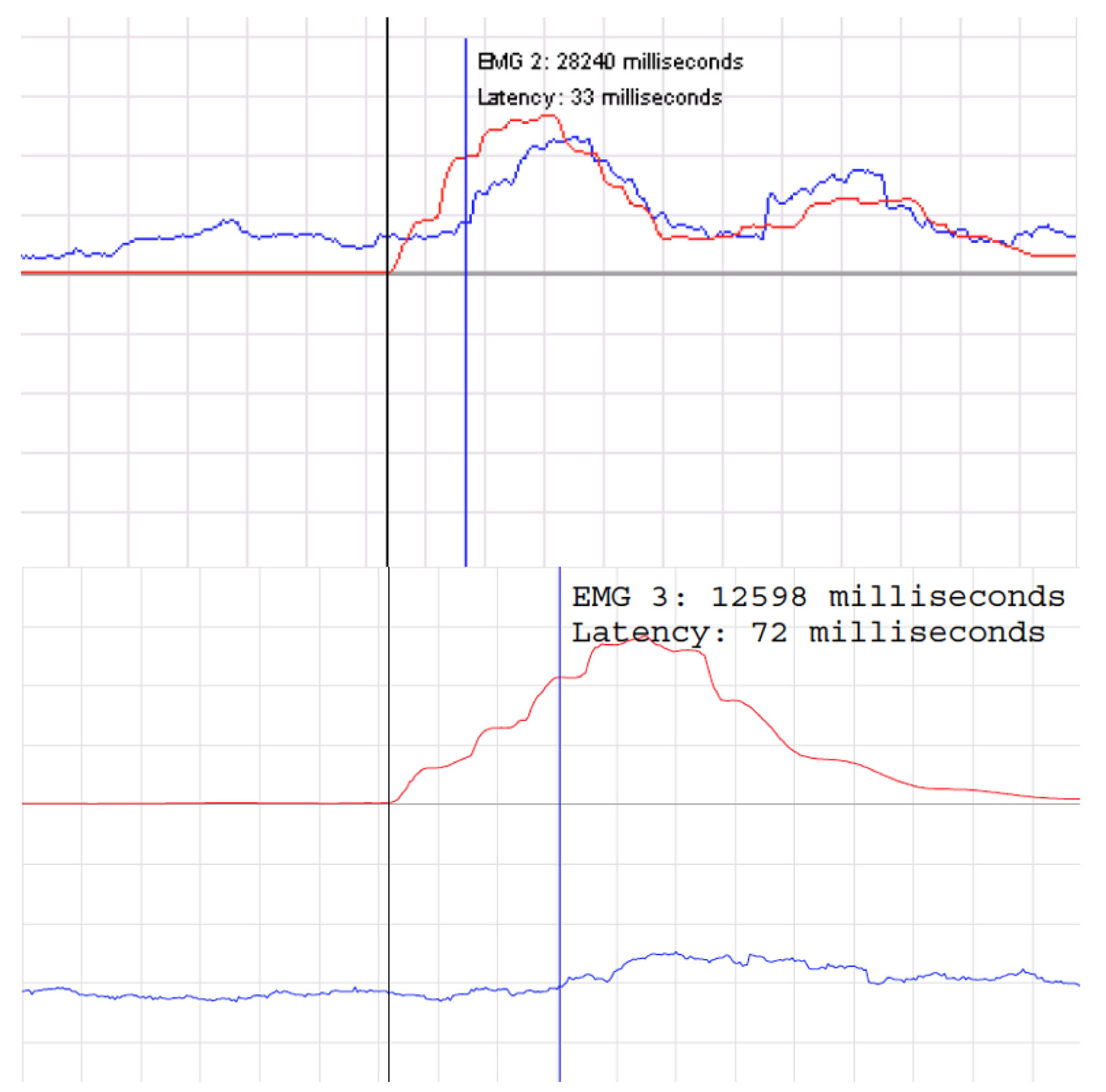 Click for large image | Figure 1. Normal bulbocavernosus reflex latency test above with latency 33 ms. Abnormal bulbocavernosus reflex latency test below with latency 72 ms. |
 Click to view | Table 1. Participant Baseline Characteristics |
Summary descriptive statistics were calculated for all variables, both continuous and categorical. Data that were bounded (e.g., “1 - 2 pads”) were converted to the mean of the range for analysis. Caffeine intake was converted to milliliters under the assumption that approximately 240 mL represented the reported “1 cup” of coffee and that approximately 355 mL represented “1 can” of caffeinated beverage. Similarly, bottles of water were converted to milliliters under the assumption that “1 bottle” represented approximately 470 mL, unless otherwise indicated. Differences between time one measurements and time two measurements (pre-to-post differences) were tested for significant change using a paired-samples t-test. Normality of the data was investigated using the Shapiro-Wilk test along with investigation of measures of skewness and kurtosis. Owing to somewhat skewed distributions, nonparametric analyses with exact P-values were calculated; however, the statistical results were identical to the parametric equivalents and hence the results of the parametric alternative are provided. Additionally, we reported 95% bootstrap confidence intervals based on 10,000 permutations for each statistical test.
| Results | ▴Top |
A total of 95 patients with UI were included in the analysis. The median age was 53 with an average duration of symptoms of 3.6 years. The number of treatments ranged from 4 to 16 (mean = 9). Pre- and post-treatment significant differences were found in several areas. The bulbocavernosus reflex latency was reduced with the mean reflex improved from 85.0 to 35.4 ms (P < 0.001). Maximum BRS at baseline was 273 ms and maximum at completion of treatment was 77 ms. Anal manometry was improved from 40.2 to 56.4 mm Hg (P < 0.001). Minimum anal manometry at baseline was 0.8 mm Hg and minimum at completion was 1.8 mm Hg. Pad count also decreased with treatment from 1.0 to 0.1 mean/median pads per day (P < 0.001). Maximum numbers of pads improved from 8 to 2. Incontinence episodes decreased from 1.8 to < 1.0 per day (P < 0.001). Maximum incontinence episodes improved from 9 to 1 per day. Perceived improvement was noted in 80% of patients (standard deviation (SD) 17.8%). At 6 to 24 months post-treatment, satisfaction was 93% (SD 12) (Table 2).
 Click to view | Table 2. Participant Outcome Statistics |
Voiding frequency ranged from an average nighttime frequency of 2 to a mean daytime frequency of 7; daily UI episodes were common, with a minimum of 0 leaks per day and a maximum of 9 (mean of 1.5). Fifty-four percent of patients reported no alcohol consumption. Patients reported an average intake of 355 mL of caffeinated products daily, and an average of 1,301 mL of total fluids daily. The most common presenting diagnoses included stress UI (64%), frequent urination (39%), urgency UI (30%), and pelvic pain (11%) (Table 1).
| Discussion | ▴Top |
The bulbocavernosus reflex is important for the neuromuscular assessment of patients with lower urinary tract dysfunction [11]. In our population of patients with UI, neuromuscular pelvic floor dysfunction was objectively established with screening BRS. Finding a consistent and standardized screening and treatment methodology for an effective PFR treatment regimen that is both objective and provides subjective effectiveness has been limited in the past due to small study sample sizes, poor methodology, or conflicting results. While this study is a retrospective analysis with the inherent limitations that are associated with this type of approach, the results in this large sample suggest that screening for baseline neuromuscular dysfunction with the BRS, followed by pelvic floor training and electrical stimulation in patients with abnormal BRS results may serve as a model for a standardized treatment. Although this is a case series without a comparison group, given the symptomatic and objective improvement shown in this study, we believe this to be a promising treatment model. However, we acknowledge that prospective comparison studies will be required to validate our approach to treating this disorder. Long-term follow-up of these patients and retreatment with these techniques is needed to evaluate for continued patient satisfaction and reduction or moderation of symptoms. We believe the strengths of this study include the objective measures of success and large sample size. We also acknowledge the weaknesses that include the retrospective design, lack of a comparison group, lack of long-term follow-up, and the lack of validated questionnaires. Future research should include a randomized controlled trial to assess utility of the BRS in a large population-based prospective trial.
Acknowledgments
We would like to thank the UNLV SOM for their IRB approval and support of this project and appreciate every author’s contribution to the project.
Disclaimer
The opinions or assertions contained herein are the private views of the authors and do not reflect the official policy or position of the Uniformed Services University of the Health Sciences, of the Department of the Air Force, nor the Department of Defense. This work was prepared by a military or civilian employee of the US Government as part of the individual’s official duties and therefore is in the public domain and does not possess copyright protection.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
AVL: protocol development, data collection, and manuscript writing; AEH, ZS and HB: manuscript writing; PK and MB: protocol development and data collection; CC: data analysis and manuscript writing.
Data Availability
Data regarding our patients and results can be procured through IRB approval at the UNLV SOM.
Abbreviations
BRS: Bulbocavernosus Reflex System; ICS: International Continence Society; IUGA: International Urogynecological Association; PFM: pelvic floor muscle; POP: pelvic organ prolapse; UI: urinary incontinence
| References | ▴Top |
- Lawrence JM, Lukacz ES, Nager CW, Hsu JW, Luber KM. Prevalence and co-occurrence of pelvic floor disorders in community-dwelling women. Obstet Gynecol. 2008;111(3):678-685.
doi pubmed - Buckley BS, Lapitan MC, Epidemiology Committee of the Fourth International Consultation on Incontinence P. Prevalence of urinary incontinence in men, women, and children—current evidence: findings of the Fourth International Consultation on Incontinence. Urology. 2010;76(2):265-270.
doi pubmed - Markland AD, Richter HE, Fwu CW, Eggers P, Kusek JW. Prevalence and trends of urinary incontinence in adults in the United States, 2001 to 2008. J Urol. 2011;186(2):589-593.
doi pubmed pmc - Ayeleke RO, Hay-Smith EJ, Omar MI. Pelvic floor muscle training added to another active treatment versus the same active treatment alone for urinary incontinence in women. Cochrane Database Syst Rev. 2015;2015(11):CD010551.
doi pubmed pmc - Bertotto A, Schvartzman R, Uchoa S, Wender MCO. Effect of electromyographic biofeedback as an add-on to pelvic floor muscle exercises on neuromuscular outcomes and quality of life in postmenopausal women with stress urinary incontinence: A randomized controlled trial. Neurourol Urodyn. 2017;36(8):2142-2147.
doi pubmed - Fitz FF, Stupp L, da Costa TF, Bortolini MAT, Girao M, Castro RA. Outpatient biofeedback in addition to home pelvic floor muscle training for stress urinary incontinence: a randomized controlled trial. Neurourol Urodyn. 2017;36(8):2034-2043.
doi pubmed - Mendes A, Rodolpho JR, Hoga LA. Non-pharmacological and non-surgical treatments for female urinary incontinence: an integrative review. Appl Nurs Res. 2016;31:146-153.
doi pubmed - Chiu M, Hagglund K, Faisal Aslam M. Pelvic floor rehabilitation with biofeedback and electrical stimulation with urostym® for treatment of urinary incontinence. Frontiers in Women’s Health. 2018;3(4):1-4.
doi - Vodusek DB. The role of electrophysiology in the evaluation of incontinence and prolapse. Curr Opin Obstet Gynecol. 2002;14(5):509-514.
doi pubmed - Vodusek DB. The role of clinical neurophysiology in urogynecology. Int Urogynecol J. 2011;22(12):1473-1477.
doi pubmed - Contreras Ortiz O, Bertotti AC, de Nunez JDR. Female pelvic floor reflex responses. Int Urogynecol J. 1994;5:278-282.
doi - Bilkey WJ, Awad EA, Smith AD. Clinical application of sacral reflex latency. J Urol. 1983;129(6):1187-1189.
doi pubmed - Varma JS, Smith AN, McInnes A. Electrophysiological observations on the human pudendo-anal reflex. J Neurol Neurosurg Psychiatry. 1986;49(12):1411-1416.
doi pubmed pmc - Contreras Ortiz O, Bertotti AC, Rodriguez JD, Lombardo RJ. Bulbocavernosus reflex in normal women. Obstet Ginecol Latin America. 1992;50:191-196.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
