| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Original Article
Volume 13, Number 1, March 2024, pages 8-11
Conservative Management Outcome of Cervical Intraepithelial Neoplasia Grade 2: A Three-Year Follow-Up Study
Junaid Rafia, b , Haroona Khalila
aObstetrics and Gynaecology, Ipswich Hospital, Ipswich IP4 5PD, UK
bCorresponding Author: Junaid Rafi, Obstetrics and Gynaecology, Ipswich Hospital, Ipswich IP4 5PD, UK
Manuscript submitted December 12, 2023, accepted March 28, 2024, published online March 31, 2024
Short title: Conservative Management Outcome of CIN2
doi: https://doi.org/10.14740/jcgo936
| Abstract | ▴Top |
Background: This study aimed to evaluate the safety and outcomes associated with the conservative management of cervical intraepithelial neoplasia grade 2 (CIN2) in women by assessing the rates of spontaneous regression of CIN2, persistence of CIN2, or progression to CIN3 and cancer.
Methods: We conducted a retrospective cohort study at DGH Hospital in the UK. We examined the medical records using the “Infoflex” system of 146 women with histologically confirmed CIN2 between April 1, 2019, and April 30, 2022. These patients underwent regular follow-ups every 6 months, including colposcopy, repeated cervical smears/punch biopsy, and human papillomavirus (HPV) testing to monitor the progression or regression of their cervical lesions. The analysis included assessing the rates of spontaneous regression of CIN2, progression to CIN3 and cancer, the duration of conservative management, and the number of patients who defaulted on follow-up.
Results: Among the 146 women with histologically confirmed CIN2, only 67 patients were eligible for conservative management. All cases underwent thorough evaluation by a multidisciplinary team (MDT); and out of these 67 cases, nine cases were upgraded after MDT review: six based on histological findings (punch biopsies) from CIN2 to CIN3, and three based on upgraded cytological assessments resulting in a total of 56 cases suitable for CIN2 management. Out of these 56 women; 39 women were in the age group between 25 and 30 years; 15 women between 30 and 35 age group; one patient was 36 years, and one patient was 40 years old. Regression rate was 71% (n = 40/56) with conservative management; two cases progressed to CIN3 (had large loop excision of the transformation zone (LLETZ) procedure) with no progression to cancer. At 6, 12, 18, and 24 months, the number of negative smears were 27/56 (48%), 5/56 (8.9%), 2/56 (3.5%), and 1/56 (1.7%), respectively.
Conclusions: Contrary to prior studies (upper age limit < 30 years), our findings support successful (71% regression rate) conservative management (CIN2) in women aged 25 - 40 years. Additionally, our observations highlight the quicker resolution of cytological abnormalities compared to histological regression.
Keywords: CIN; HPV; LLETZ
| Introduction | ▴Top |
Historically, high-grade squamous intraepithelial dysplasia, encompassing both cervical intraepithelial neoplasia grade 2 (CIN2) and grade 3 (CIN3), has been collectively managed. Consequently, a significant cohort of patients diagnosed with CIN2 and CIN3 received treatment through large loop excision of the transformation zone (LLETZ). CIN3 is traditionally regarded as a conclusive precancerous condition, carrying an estimated 30% probability of evolving into invasive cervical carcinoma [1]. In contrast, CIN2 has conventionally served as the clinical threshold for intervention. However, recent discourse has brought into question the categorization of CIN2, positing that it may not represent a discrete pathological entity but rather a multifaceted and indeterminate class, encompassing both benign human papillomavirus (HPV) infection and incipient precancerous changes [1, 2].
Prior investigations have endeavored to assess the effects of a conservative management approach, during a follow-up period spanning from 6 to 48 months. Certain studies have reached the conclusion that such a conservative strategy may be deemed justifiable, particularly in the context of younger women who have not yet completed their families. We posit that this approach has the potential to significantly reduce the occurrence of overtreatment in most female patients.
This study aimed to evaluate the safety and outcomes associated with the conservative management of CIN2 in women by assessing the rates of spontaneous regression of CIN2, persistence of CIN2, or progression to CIN3 and cancer.
| Materials and Methods | ▴Top |
We conducted a retrospective cohort study at DGH Hospital in the UK. We examined the medical records using the “Infoflex” system of 146 women with histologically confirmed CIN2 between April 1, 2019, and April 30, 2022. These patients underwent regular follow-ups every 6 months, including colposcopy, repeated cervical smears/punch biopsy, and HPV testing to monitor the progression or regression of their cervical lesions. The analysis included assessing the rates of spontaneous regression of CIN2, progression to CIN3 and cancer, the duration of conservative management, and the number of patients who defaulted on follow-up. The conservative management period was limited to 6 - 24 months since UK guidance recommend treatment if the CIN2 lesion has not resolved within 24 months, and age limit in our study was 25 - 40 years. This study was registered with the Clinical Audit Department (registration number: WC22-1249). Ethical compliance with human/animal study protocols is not applicable as this study does not involve direct participation of humans or animals.
| Results | ▴Top |
Among the 146 women with histologically confirmed CIN2, 67 patients were eligible for conservative management. All cases underwent thorough evaluation by a multidisciplinary team (MDT) to ensure appropriate decisions regarding conservative management and to eliminate instances of under diagnosis or over diagnosis. Out of these 67 cases, nine cases were upgraded after MDT review: six based on histological findings (punch biopsies) from CIN2 to CIN3, and three based on upgraded cytological assessments resulting in a total of 56 cases suitable for CIN2 management. The initial referral for abnormal smears for colposcopy referrals for final cases which underwent conservative management after MDT discussion are shown in Table 1.
 Click to view | Table 1. Initial Referral Smears in Conservative Management Group After MDT Discussion |
Out of these 56 women; 39 women were in the age group between 25 and 30 years; 15 women between 30 and 35 age group; one patient was 36 years, and one patient was 40 years old.
Regression rate was 71% (n = 40/56) with conservative management; and successful outcome was characterized by either a regression of high-grade lesions observed during colposcopy or negative cytology results at 6-month follow-up in colposcopy. At 6, 12, 18, and 24 months, the number of negative smears were 27/56 (48%), 5/56 (8.9%), 2/56 (3.5%), and 1/56 (1.7%), respectively (Fig. 1).
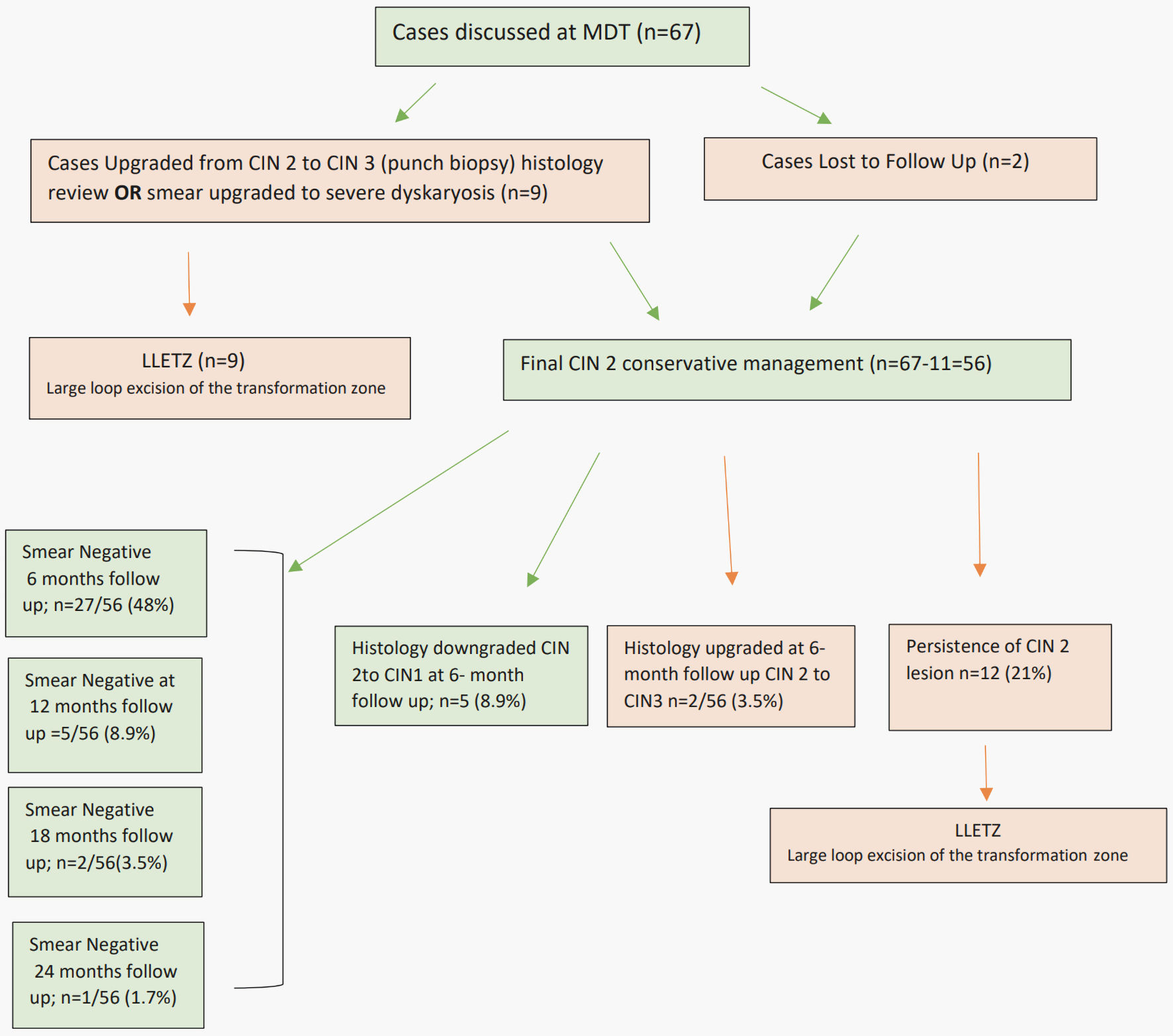 Click for large image | Figure 1. Outcome of CIN2 conservative management. CIN2: cervical intraepithelial neoplasia grade 2; MDT: multidisciplinary team; LLETZ: large loop excision of the transformation zone. |
Whereas histological downgrading from CIN2 to CIN1 or normal occurred in five cases at the 6-month follow-up. In the conservative management subgroup for CIN2, 12 out of 56 patients (21%) showed persistence of lesions and subsequently underwent LLETZ. Notably, only two cases (3.5%) in the conservative management group progressed to histologically confirmed CIN3 at a 6-month follow-up, with no instances of cervical cancer observed during the 24-month median follow-up period.
| Discussion | ▴Top |
CIN2 is a challenging category known for its limited reproducibility and encompassing manifestations of HPV infections and early abnormalities. Notably, it is highly regressive, particularly among young women. The study supports the notion that CIN2 can be effectively monitored, especially in women contemplating future pregnancies. This approach is favored due to the low cancer risk associated with CIN2 and the heightened risk of preterm delivery linked to excisional treatments [3].
A critical review by Ostor in 1993 [4] concluded that the likelihood of regression from CIN2 to CIN1 is 40%, persistence is 20%, progression to CIN3 is 20%, and progression to invasive cancer is 5%. In a study by Tainio et al [5], 3,160 women with CIN2 lesions were investigated for spontaneous regression, persistence, or progression to CIN3 or cancer. At the conclusion of the follow-up period, 18% of CIN2 lesions had progressed, 32% persisted, and 50% had regressed.
The British Society for Colposcopy and Cervical Pathology conducted a survey [6] to assess its members’ attitudes toward conservative management of CIN2. Of over 500 respondents, 68% reported offering this option in the absence of formal specific guidance. The majority considered age over 40 years and the presence of large lesions as contraindications for conservative management.
According to UK guidelines [7], individuals can be considered for conservative management of CIN2 if specific criteria are met. These criteria include ensuring that colposcopy examinations are adequate and have ruled out CIN3 and invasive lesions, that CIN2 has been histologically confirmed and reviewed at MDT meetings to exclude underdiagnosis or overdiagnosis, and that patients agree to regular 6-month follow-up colposcopic examinations, including repeat cervical sampling and biopsy if indicated due to the presence of a more severe lesion (CIN3) on colposcopic examination. Patients must also understand that the resolution of CIN2 can take up to 24 months.
Notably, this guideline [7] does not specify upper or lower age cutoffs for conservative management. While earlier published study included women aged 25 - 30 years, with the highest incidence observed among those aged 25 - 29 years (8.1 per 1,000 women [8]), our study demonstrates the safety and efficacy of CIN2 conservative management in women aged 25 - 40 years, in line with other studies that utilized age cutoffs of 39 - 44 years [9-11]. In the UK, CIN2 follow-up is up to 24 months, whereas in Germany, CIN1 is followed up to 24 months and CIN2 is followed up to 12 months [12].
While Tainio et al [5] reported a regression rate of 52% after 6 months and a regression rate of 50% after 24 months. Recent studies, such as Lee et al in 2018 [13] and Tjandraprawira et al in 2022 [9], have shown higher regression rates of 74% and 77%, respectively. In our study, we observed an overall regression rate of 71% and a regression rate of 57% after 6 months.
Additionally, previous studies, such as that by Godfrey et al [14] from the UK, reported more histological downgrades at 6-month follow-ups, with a lag in cytology becoming negative afterward. In contrast, our study found a higher proportion of cytology turning negative at 6-month follow-ups compared to histological downgrades. In this context, a study by Silver et al [10] reported that only 20% of women met the criteria to exit colposcopic follow-up and return to routine screening, whereas more cases of early regression of smears (48%) in our study allowed discontinuation of colposcopic follow-up at 6 months.
Conclusions
Contrary to prior studies (upper age limit < 30 years), our findings support successful (71% regression rate) conservative management (CIN2) in women aged 25 - 40 years. Additionally, our observations highlight the quicker resolution of cytological abnormalities compared to histological regression.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Patient consent was not required as the retrospective observational study did not involve any patient identifiable data.
Author Contributions
JR conceived the idea, conducted the study, analyzed the data, and wrote the initial manuscript. HK reviewed the manuscript. Both authors approved the final version.
Data Availability
Data are available for the editorial team if required.
| References | ▴Top |
- Gage JC, Schiffman M, Hunt WC, Joste N, Ghosh A, Wentzensen N, Wheeler CM, et al. Cervical histopathology variability among laboratories: a population-based statewide investigation. Am J Clin Pathol. 2013;139(3):330-335.
doi pubmed pmc - Carreon JD, Sherman ME, Guillen D, Solomon D, Herrero R, Jeronimo J, Wacholder S, et al. CIN2 is a much less reproducible and less valid diagnosis than CIN3: results from a histological review of population-based cervical samples. Int J Gynecol Pathol. 2007;26(4):441-446.
doi pubmed - Kyrgiou M, Athanasiou A, Paraskevaidi M, Mitra A, Kalliala I, Martin-Hirsch P, Arbyn M, et al. Adverse obstetric outcomes after local treatment for cervical preinvasive and early invasive disease according to cone depth: systematic review and meta-analysis. BMJ. 2016;354:i3633.
doi pubmed pmc - Ostor AG. Natural history of cervical intraepithelial neoplasia: a critical review. Int J Gynecol Pathol. 1993;12(2):186-192.
pubmed - Tainio K, Athanasiou A, Tikkinen KAO, Aaltonen R, Cardenas J, Hernandes, Glazer-Livson S, et al. Clinical course of untreated cervical intraepithelial neoplasia grade 2 under active surveillance: systematic review and meta-analysis. BMJ. 2018;360:k499.
doi pubmed pmc - Macdonald M, Smith JHF, Tidy JA, Palmer JE. Conservative management of CIN2: National Audit of British Society for Colposcopy and Cervical Pathology members' opinion. J Obstet Gynaecol. 2018;38(3):388-394.
doi pubmed - Guidance; Cervical screening: programme and colposcopy management. Access at: https://www.gov.uk/government/publications/cervical-screening-programme-and-colposcopy-management/3-colposcopic-diagnosis-treatment-and-follow-up.
- Insinga RP, Glass AG, Rush BB. Diagnoses and outcomes in cervical cancer screening: a population-based study. Am J Obstet Gynecol. 2004;191(1):105-113.
doi pubmed - Tjandraprawira KD, Olaitan A, Petrie A, Wilkinson N, Rosenthal AN. Comparison of Expectant and Excisional/Ablative Management of Cervical Intraepithelial Neoplasia Grade 2 (CIN2) in the Era of HPV Testing. Obstet Gynecol Int. 2022;2022:7955290.
doi pubmed pmc - Silver MI, Gage JC, Schiffman M, Fetterman B, Poitras NE, Lorey T, Cheung LC, et al. Clinical outcomes after conservative management of cervical intraepithelial neoplasia grade 2 (CIN2) in women ages 21-39 years. Cancer Prev Res (Phila). 2018;11(3):165-170.
doi pubmed - Skorstengaard M, Lynge E, Suhr J, Napolitano G. Conservative management of women with cervical intraepithelial neoplasia grade 2 in Denmark: a cohort study. BJOG. 2020;127(6):729-736.
doi pubmed pmc - Hillemanns P, Friese K, Dannecker C, Klug S, Seifert U, Iftner T, Hadicke J, et al. Prevention of cervical cancer: Guideline of the DGGG and the DKG (S3 Level, AWMF Register Number 015/027OL, December 2017) - Part 2 on triage, treatment and follow-up. Geburtshilfe Frauenheilkd. 2019;79(2):160-176.
doi pubmed pmc - Lee MH, Finlayson SJ, Gukova K, Hanley G, Miller D, Sadownik LA. Outcomes of conservative management of high grade squamous intraepithelial lesions in young women. J Low Genit Tract Dis. 2018;22(3):212-218.
doi pubmed pmc - Godfrey MAL, Nikolopoulos M, Garner JE, Adib TR, Mukhopadhyay D, Rains JS, Harper CA, et al. Conservative management of cervical intraepithelial neoplasia grade 2 (CIN2) in women under 30 years of age: a cohort study. Eur J Obstet Gynecol Reprod Biol. 2018;228:267-273.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
