| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Original Article
Volume 13, Number 1, March 2024, pages 1-7
Stroke Education for Obstetric Providers: A Single-Center Pilot Following a Case of Delayed Recognition of Postpartum Intracerebral Hemorrhage
Kali J. Sullivana, h, Matthew N. Andersonb, Ali Saadc, Desmond Suttond, Bradford B. Thompsone, Linda C. Wendellf, Aleksandra Yakhkindg
aTufts University School of Medicine, Boston, MA, USA
bUniversity of Washington, Department of Neurosurgery, Seattle, WA, USA
cClimate and Health Department, University of Colorado, Aurora, CO, USA
dDepartment of Obstetrics and Gynecology, Maternal-Fetal Medicine, Mount Sinai West Hospital, New York, NY, USA
eDepartment of Neurology, Neurocritical Care, St. Elizabeth’s Medical Center, Brighton, MA, USA
fDivision of Neurology, Department of Medicine, Mount Auburn Hospital, Cambridge, MA, USA
gDepartment of Neurology, Tufts Medical Center, Boston, MA, USA
hCorresponding Author: Kali J. Sullivan, Tufts University School of Medicine, Boston, MA 02111, USA
Manuscript submitted January 11, 2024, accepted March 25, 2024, published online March 31, 2024
Short title: Stroke Education for Obstetric Providers
doi: https://doi.org/10.14740/jcgo943
| Abstract | ▴Top |
Background: Stroke is three times more likely in obstetric patients than in age-adjusted non-pregnant women. No studies have focused on obstetric provider education for stroke management. A case of a postpartum woman with intracerebral hemorrhage at a large obstetrics hospital spurred modification of the code stroke protocol and an educational seminar on neurologic emergencies geared towards obstetric providers. The effectiveness of stroke triage training to improve understanding of management in obstetric patients was assessed.
Methods: Obstetric providers were assessed before and after attending a 1-h educational seminar by stroke experts from the affiliated comprehensive stroke center at an associated large academic institution. The knowledge assessment included seven questions about concerning symptoms and initial steps in management of suspected stroke.
Results: Twenty-eight out of 48 participants completed before and after knowledge assessments. The average increase in point score was 1.25 (21%). The greatest post-education increases occurred regarding blood pressure augmentation during a stroke alert (18% to 82% correct) and initial tests needed for evaluation (36% to 89% correct). Providers learned head imaging must be obtained to differentiate between types of strokes before treating hypertension, and labs, except finger stick glucose, are not needed before administering a thrombolytic.
Conclusions: Obstetric patients are at increased risk of stroke, and targeted clinician education can improve knowledge of initial management steps. Obstetric practices should consider additional education for nurses and providers on managing stroke, as proper stroke management is time sensitive and can reduce maternal mortality.
Keywords: Quality improvement; Stroke; Provider education; Obstetrics; Neurological disorders in pregnancy
| Introduction | ▴Top |
Pregnancy-associated strokes (PAS) occur in 30 per 100,000 pregnancies, which is three times the incidence of age-adjusted non-pregnant women. They are a leading cause of mortality in pregnancy [1, 2]. Approximately 11-32% of all PAS occur during the antepartum period, 34-41% during labor or birth, and 34-48% occur postpartum [3-6]. The pathophysiology of pregnancy increases the risk of stroke due to increased blood volume and cardiovascular and coagulation changes [7]. Mode of delivery further impacts risk of stroke, and patients who have a cesarean birth may be at increased risk for up to 12 months postpartum [8, 9]. Stroke can be separated into two main categories: ischemic (non-hemorrhagic) and hemorrhagic. Ischemic strokes can be further divided into arterial ischemic strokes and cerebral sinus venous thrombosis. The incidence of overall pregnancy-related ischemic stroke and pregnancy-related arterial ischemic stroke is 19.9 and 12.2 per 100,000 pregnancies, respectively [1]. Risk factors include preeclampsia, gestational diabetes, infection, as well as factors outside of pregnancy such as hypertension, hyperlipidemia, coagulopathies, smoking, migraines, and social determinants of health [10, 11]. The incidence of hemorrhagic stroke is 12.2 per 100,000 pregnancies and makes up a higher proportion of hemorrhage stroke in the general population [1]. Risk factors include hypertension, cerebrovascular malformations, preeclampsia-spectrum disorders, and gestational trophoblastic disease [10]. The increasing prevalence of traditional cardiovascular risk factors among younger adults, such as hypertension, diabetes, and obesity, as well as the advancing average maternal age at time of birth, likely have increased the risk of acute stroke during pregnancy in recent time [12]. Cerebral venous sinus thrombosis can cause cerebral ischemia and intracerebral hemorrhage (ICH), and thus should always be on the differential when patients present with acute neurologic changes. Its incidence associated with pregnancy is three times higher than that of the general population. Risk factors include hypertension, infection, hypercoagulability, dehydration, smoking, age, hyperemesis gravidarum, and malignancy [13]. Additionally, black race has been reported to be a risk factor for each type of pregnancy-associated stroke, however these studies do not account for the effects of structural racism on health outcomes [14].
Hypertensive disorders of pregnancy, including preeclampsia, increase the risk of stroke. Preeclampsia is estimated to complicate 3-6% of pregnancies in the United States [11, 15]. Preeclampsia with severe features (PESF) is estimated to complicate 1-2% of pregnancies and is diagnosed by the presence of one or more of the following in a patient with preeclampsia: systolic blood pressure ≥ 160 mm Hg and/or diastolic blood pressure ≥ 110 mm Hg requiring antihypertensive medications or presence of two or more severe range blood pressures 4 h apart, symptoms of central nervous system dysfunction, hepatic abnormality, thrombocytopenia, kidney impairment, or pulmonary edema [16].
ICH should be considered when there is any change in mental status or a new neurological deficit in the antepartum, peripartum, or postpartum period, especially in the setting of a hypertensive disorder of pregnancy. The adjusted relative risk of ICH postpartum has been described as 28.3 [17]; 14-55% of cases of ICH in pregnancy had coexisting severe preeclampsia and/or eclampsia, and the presence of either disease is associated with a four-fold increased risk of stroke [3]. Endothelial dysfunction, impaired cerebral autoregulation, and severe hypertension in the setting of preeclampsia predispose women with this spectrum of disorders to stroke [18]. Additionally, hypertension and thrombocytopenia independently increase the risk of ICH. When they occur simultaneously in preeclampsia, this makes pregnant patients especially vulnerable. Posterior reversible encephalopathy syndrome (PRES) is reported as a rare complication of preeclampsia and can also be an inciting event for ICH [18, 19].
Despite the increased risk of PAS, obstetric providers do not typically receive dedicated stroke education. A patient case of PESF complicated by ICH at a large obstetrics hospital spurred the creation of an educational seminar about stroke triage for obstetrics providers and nurses. As part of this quality improvement project, the research team assessed the effectiveness in stroke triage training to improve understanding of management steps in obstetrics patients with symptoms of stroke. To our knowledge, no studies to date focus on provider education on stroke management in the obstetrics setting.
Patient case
The patient was a 27-year-old right-handed woman, gravida 1, para 1 (G1P1) who was induced to deliver at 36 weeks for gestational thrombocytopenia (platelet count 93,000/µL). Her pregnancy was otherwise uncomplicated. Her delivery was complicated by uterine bleeding that required Bakri balloon tamponade and uterine artery embolization by interventional radiology under conscious sedation with propofol and fentanyl. She was hypertensive during the case and was treated with additional pain medication. The patient was expected to be sedated post-procedure, but 4 h after the procedure, she was unarousable with a dilated and unreactive right pupil and a code stroke was called. Her systolic blood pressure at that time ranged between 150 and 160 mm Hg. Upon evaluation by neurology, her National Institutes of Health Stroke Scale (NIHSS) score was 26 due to her loss of consciousness and weakness. Emergent computed tomography (CT) of her brain showed a 25-mL ICH in the right basal ganglia with intraventricular extension, 6 mm of midline shift and compression of the midbrain (Fig. 1). The patient underwent emergent hyperosmolar therapy, external ventricular drain (EVD) placement. Her exam improved from no movement of her extremities in response to noxious stimuli to being able to follow instructions, resulting in an improved Glasgow Coma Score (GCS) score from 3 to 9. She was treated with verapamil for presumed reversible cerebral vasoconstriction syndrome (RCVS) and levetiracetam for seizures. She underwent a decompressive hemicraniectomy to manage elevations in intracranial pressure due to cerebral edema. After 8 weeks in the intensive care unit (ICU), she was discharged to a rehabilitation center with right sided weakness and aphasia. By her 3-month outpatient follow-up, her NIHSS was 0, and her only persistent symptoms were mild left-handed weakness and occasional headaches. At her 6-month follow-up, she only had mild fine motor difficulties in her left hand.
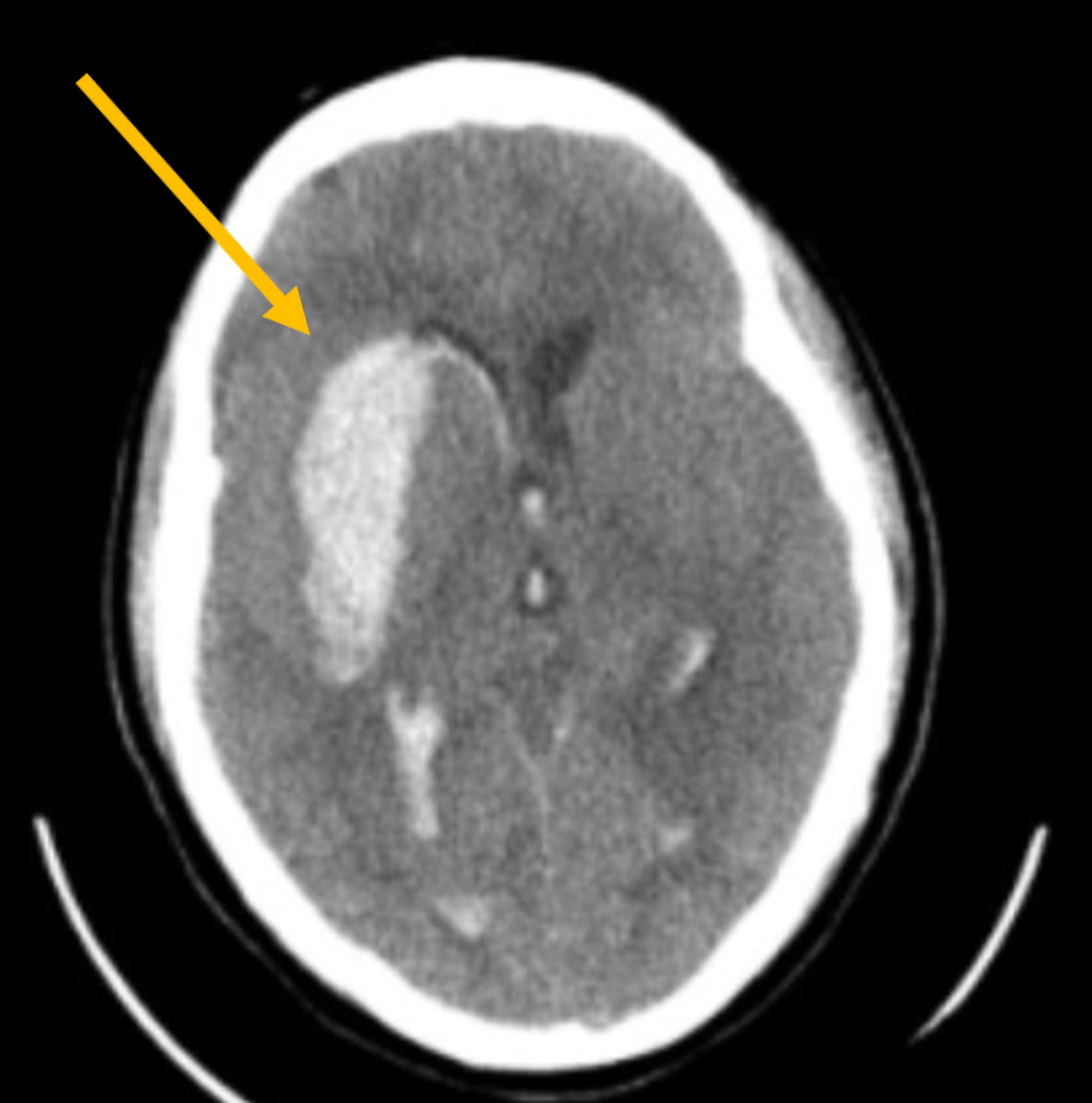 Click for large image | Figure 1. Snapshot of an axial cut of the initial non-contrast head CT showing a 25 mL hemorrhage (arrow) in the right basal ganglia with intraventricular extension causing midline shift and cerebral edema. CT: computed tomography. |
| Materials and Methods | ▴Top |
The patient case described above resulted in extensive discussions between neurology and obstetrics about how to improve stroke recognition in peripartum patients. Root-cause analysis identified symptom recognition and knowledge of initial steps of assessment and management as potential targets for improvement. The decision was made to hold a one-time educational seminar at a monthly hospital safety conference geared towards currently practicing obstetrics physicians, advanced practice providers (APPs) and nurses to assess peri-procedural stroke awareness. This study was exempt from Institutional Review Board review due to low risk to participants. The study was still conducted in compliance with the ethical standards of Women and Infants Hospital on human subjects as well as with the Helsinki Declaration. The speakers were a board-certified vascular neurologist and the stroke coordinator of the affiliated comprehensive stroke center. Participants were assessed before and after the 1-h educational seminar on stroke management in pregnant patients. The knowledge assessment included seven questions about concerning symptoms and initial steps in management of a suspected stroke, which were determined from the root-cause analysis to be the highest yield topics (Fig. 2). The assessment aimed to assess the effectiveness of this seminar and investigators hypothesized an increase in participant scores before and after the intervention. We performed McNemar tests to statistically quantify the difference between before and after scores in Stata [20], as well as a paired t-test to compare final score means before and after intervention (Table 1).
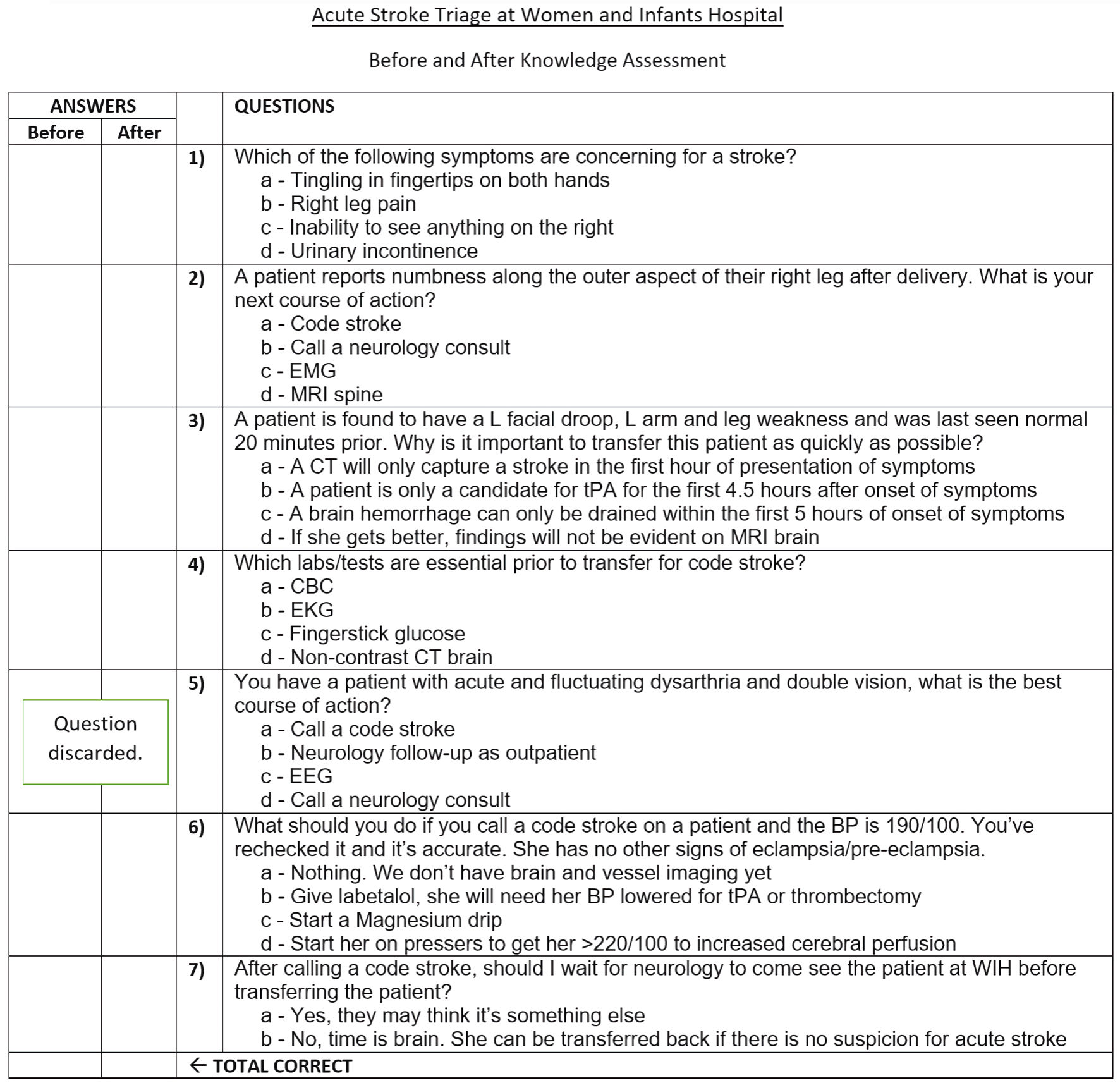 Click for large image | Figure 2. Before and after knowledge assessment after acute stroke triage education as part of quality improvement project at Women and Infants Hospital. |
 Click to view | Table 1. Comparison of Knowledge Assessment Results for Pre- and Post-Education Session |
| Results | ▴Top |
Forty-eight providers attended the seminar. Thirty-two of 48 fully completed pre-intervention knowledge assessments. Twenty-eight out of 32 fully completed post-intervention assessments. Twenty incomplete pre- or post-assessments were excluded. One question was discarded due to ambiguity in answer choices, and thus the maximum score analyzed was out of 6. The average point scores before and after the seminar were 4 (67%) and 5.36 (87.5%), respectively. Thus, the average increase in point score was 1.25 out of 6 (21%). Correct responses from providers regarding blood pressure management during a stroke alert increased from 18% pre-education to 82% post-education. Using the McNemar test, this was determined to be significant change (P = 0.006) in responses from participants after receiving pregnancy-related stroke management education. Prior to the education session, half of the participants would have given labetalol and five would have started magnesium for a blood pressure of 190/85 in the setting of a stroke alert in a pregnant patient. After education, 18 providers with previously incorrect answers significantly improved their scores by altering their response to the correct answer: Do not adjust blood pressure until a head CT has differentiated the type of stroke because permissive hypertension is preferred in the setting of acute ischemic stroke (P ≤ 0.001).
Correct responses from providers regarding initial tests needed for evaluation similarly significantly increased from 36% pre-education to 89% post-education (P ≤ 0.001). Initially, 18 participants stated that labs or diagnostics were needed before calling the neurology team. After education, 15 of those participants corrected their answer to obtaining fingerstick glucose prior to making the call, since hyper or hypoglycemia can mimic stroke symptoms. Five participants learned that homonymous hemianopsia was more indicative of a stroke than tingling in fingertips or pain in one leg. Eighty-six percent of respondents (24 of 28) knew prior to education the importance of quick diagnosis due to the limited time window for thrombolysis in the setting of ischemic stroke. Table 1 shows the summary of results.
| Discussion | ▴Top |
Due to the prevalence of stroke in pregnancy, provider education on recognition and management is essential. In the described case, procedural sedation delayed diagnosis of ICH. While this patient did well, her life-threatening hospital course could have been shortened or avoided with early recognition and treatment.
Treatment of stroke requires prompt identification and appropriate management. When a patient has an abrupt change in mental status or new focal neurologic deficit, a stroke alert should be activated to call neurological experts to the bedside as soon as possible. At the same time, a non-contrast head CT and computed tomography angiography (CTA) head and neck with contrast should be obtained without delay after a fingerstick glucose level is checked. If there is no hemorrhage and an ischemic stroke is suspected, a thrombolytic can be administered if the patient presents within the appropriate time window if benefits outweigh risks. Neither alteplase nor tenecteplase cross the placenta [21]. A patient may also be a candidate for an embolectomy, direct intravascular removal of a blood clot, if a large vessel occlusion is discovered. Obstetric hospitals should have transfer procedures in place with comprehensive stroke centers if neurointerventional radiology is not available on site.
If an ICH is discovered, blood pressure must be controlled immediately, any coagulopathy should be corrected, and emergent surgical intervention for hydrocephalous or clot evacuation should be performed if indicated [22]. Table 2 outlines the ideal time metrics for responding to stroke alerts. Stroke should be on providers’ list of differential diagnoses when there is a change in mental status in the setting of high blood pressure or coagulopathy in pregnancy and the peripartum period. Prompt intervention to prevent hydrocephalous and further brain injury is essential.
 Click to view | Table 2. Proposed Time Metrics for the Acute Management of ICH |
A root-cause analysis in the case of this patient determined symptom recognition and initial management to be the highest yield targets for improvement. On the pre-educational assessment however, most providers knew how to differentiate symptoms of a stroke from other neurologic conditions associated with pregnancy like femoral cutaneous nerve palsy and carpel tunnel syndrome. Loss of consciousness is an uncommon presentation of stroke, but an important one for obstetric providers to recognize quickly especially in high-risk scenarios like preeclampsia and eclampsia.
Respondents to the assessments knew the time sensitive nature of stroke before the educational intervention. The cause of the delay in the care for this patient was not due to a lack of urgency but rather to a lack of recognition. “Time is brain” is an expression frequently used in stroke education to signify the importance of rapid intervention for neurologic emergencies [23]. Every minute that the brain lacks blood supply, it is estimated that 1.9 million neurons die [23]. Any neurologic emergency including hemorrhages, seizures and hydrocephalous puts brain cells at risk, increasing the risk of death and disability, so rapid intervention is key [21, 22].
The key takeaway from the educational intervention was regarding initial assessment and management. In the assessed group, many providers focused on early blood pressure management before obtaining head imaging. This is understandable as hypertensive diseases of pregnancy are incredibly concerning and initial management includes immediate blood pressure control. However, if a cerebrovascular event is suspected in conjunction with the elevated blood pressure, steps must be taken to evaluate for ischemic stroke. Rapid lowering of blood pressure may result in cerebral hypoperfusion and worsen brain ischemia, so blood pressure goals should only be determined after a head CT and in collaboration with neurology and neurosurgery [24].
Although head imaging is integral to diagnosis, providers may be concerned about the risks associated with ionizing radiation in pregnancy. According to the American College of Radiology and the American College of Obstetrics and Gynecology, X-ray-based examinations that do not directly expose the pelvis or gravid uterus to the X-ray beam do not require verification of pregnancy status; thus, head imaging is safe. The amount of radiation a fetus is exposed to in a non-contrast head CT and CT angiogram head and neck is negligible [25, 26].
Another learning point from the seminar is that the only lab or testing necessary before transport to CT during a stroke alert is a fingerstick glucose, since both hyperglycemia and hypoglycemia can mimic stroke. Obtaining complete blood counts, basic metabolic panels, coagulopathy testing, and electrocardiogram (EKG) should not delay obtaining the head CT.
The discarded question was whether to call a stroke alert for “acute and fluctuating dysarthria and double vision”. The answers to this question were controversial. If both occurred abruptly, they could be signs of stuttering perfusion to the posterior circulation. Conversely, these could be nonspecific symptoms and could be a medication effect. Ultimately, the study team recommended not to hesitate to talk to the neurology team on call about such cases to decide whether a stroke alert needs to be activated.
This is the first study of its kind to outline a provider-targeted intervention for stroke management in pregnant patients. It was a single center pilot without a control group and the number of participants was too low to determine statistically significant efficacy of this type of intervention. Low rates of pre- and post-intervention knowledge assessment completion were due to participants leaving the seminar early or choosing not to complete both assessments. This introduces a selection bias and may not accurately represent the entire studied population. Further studies should include demographics data on respondents to differentiate results based on profession (physician, APP, nurse) and years of experience. They should also review responses in partially completed knowledge assessments to look for selection bias. Participants should also be followed up to assess knowledge over time.
Previous studies have suggested simulation is effective at improving knowledge and confidence in various specialties of medicine [27, 28]. An ideal study would also assess the effectiveness of the educational program on provider response times and confidence in real life emergent cases as well as patient outcomes. Fortunately, while stroke is a complex and possibly devastating risk of pregnancy for many reasons including hypercoagulable state, diseases of cerebral autoregulation like preeclampsia, PRES, RCVS and thrombocytopenia, it remains overall rare. It may be difficult to assess real life provider response because of its overall low prevalence among peripartum patients.
Overall, this study revealed that targeted obstetric provider education may be an effective tool to improve knowledge about stroke assessment and management. Many providers have a good appreciation of concerning signs and symptoms in more straightforward cases, but as suggested by our patient case, may struggle with more complicated stroke presentations. Moreover, beyond signs and symptoms, stroke is not encountered everyday by obstetrics providers. It is the responsibility of hospitals to educate obstetrics providers to ensure prompt identification and treatment of stroke in pregnant patients. Further workup and management of PAS should be done together with experts trained in caring for patients with neurologic conditions. Obstetrics providers in low-resource settings without access to specialists should seek out expertise when able, but they may choose to do additional training available from societies such as the Neurocritical Care Society and the American Heart Association/American Stroke Association.
In conclusion, obstetrics patients are at increased risk of stroke. ICH should be considered when there is a change in mental status in the setting of high blood pressure or coagulopathy in pregnancy and the peripartum period. Prompt intervention to prevent clot expansion, hydrocephalous and secondary brain injury is essential, and more training for obstetric providers could provide life-saving skills for the recognition of neurologic emergencies in high-risk obstetrics. Targeted and interactive provider education can improve knowledge of initial management of stroke in obstetric patients and should be studied further. In the meantime, obstetric practices and hospitals should consider targeted education for providers as proper stroke management is time sensitive and can reduce maternal morbidity and mortality.
Acknowledgments
We extend our gratitude to JoAnn Serafin, Stroke Coordinator at Rhode Island Hospital, for her role in teaching during the education session. This quality improvement project was performed at Rhode Island Hospital and Woman and Infant’s Hospital.
Financial Disclosure
None to declare.
Conflict of Interest
Table 2 was originally presented at the NCS Annual Meeting in 2022 by Anne Alexandrov, Stephan Mayer, Joshua Goldstein, Jennifer Frontera, Christopher Kellner, and Aleksandra Yakhkind.
Informed Consent
Not applicable.
Author Contributions
Kali J. Sullivan, as the first author, played a pivotal role in the data analysis phase of this study. She was also instrumental in both the drafting and critical revision of the manuscript, contributing significantly to its intellectual content. Dr. Anderson, Dr. Saad, Dr. Sutton, Dr. Thompson, and Dr. Wendell collectively contributed to the conceptual design and strategic planning of the project. Each of these authors significantly engaged in the writing process and played a crucial role in revising the manuscript critically for important intellectual content. Dr. Yakhkind, serving as the primary investigator, was integral to the conception and design of the project. She contributed extensively to the data analysis and was a key contributor in the writing and critical editing of the manuscript. Her role was central in guiding the project to its completion and ensuring the integrity of its scientific content.
Data Availability
The data supporting the findings of this study are available within the article.
Abbreviations
PAS: pregnancy-associated strokes; PESF: preeclampsia with severe features; ICH: intracerebral hemorrhage; PRES: posterior reversible encephalopathy syndrome; NIHSS: National Institutes of Health Stroke Scale; CT: computed tomography; CTA: computed tomography angiography; EVD: external ventricular drain; GCS: Glasgow Coma Score; RCVS: reversible cerebral vasoconstriction syndrome; ICU: intensive care unit; EKG: electrocardiogram
| References | ▴Top |
- Swartz RH, Cayley ML, Foley N, Ladhani NNN, Leffert L, Bushnell C, McClure JA, et al. The incidence of pregnancy-related stroke: a systematic review and meta-analysis. Int J Stroke. 2017;12(7):687-697.
doi pubmed - Sanders BD, Davis MG, Holley SL, Phillippi JC. Pregnancy-associated stroke. J Midwifery Womens Health. 2018;63(1):23-32.
doi pubmed pmc - James AH, Bushnell CD, Jamison MG, Myers ER. Incidence and risk factors for stroke in pregnancy and the puerperium. Obstet Gynecol. 2005;106(3):509-516.
doi pubmed - Kamel H, Navi BB, Sriram N, Hovsepian DA, Devereux RB, Elkind MS. Risk of a thrombotic event after the 6-week postpartum period. N Engl J Med. 2014;370(14):1307-1315.
doi pubmed pmc - Witlin AG, Mattar F, Sibai BM. Postpartum stroke: a twenty-year experience. Am J Obstet Gynecol. 2000;183(1):83-88.
doi pubmed - Moatti Z, Gupta M, Yadava R, Thamban S. A review of stroke and pregnancy: incidence, management and prevention. Eur J Obstet Gynecol Reprod Biol. 2014;181:20-27.
doi pubmed - Zambrano MD, Miller EC. Maternal stroke: an update. Curr Atheroscler Rep. 2019;21(9):33.
doi pubmed pmc - Lin SY, Hu CJ, Lin HC. Increased risk of stroke in patients who undergo cesarean section delivery: a nationwide population-based study. Am J Obstet Gynecol. 2008;198(4):391.e391-397.
doi pubmed - Lanska DJ, Kryscio RJ. Risk factors for peripartum and postpartum stroke and intracranial venous thrombosis. Stroke. 2000;31(6):1274-1282.
doi pubmed - Uchikova EH, Ledjev II. Changes in haemostasis during normal pregnancy. Eur J Obstet Gynecol Reprod Biol. 2005;119(2):185-188.
doi pubmed - Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US); 2006. Accessed November 3, 2023. http://www.ncbi.nlm.nih.gov/books/NBK52651/.
- Elgendy IY, Gad MM, Mahmoud AN, Keeley EC, Pepine CJ. Acute stroke during pregnancy and puerperium. J Am Coll Cardiol. 2020;75(2):180-190.
doi pubmed - Otite FO, Patel S, Sharma R, Khandwala P, Desai D, Latorre JG, Akano EO, et al. Trends in incidence and epidemiologic characteristics of cerebral venous thrombosis in the United States. Neurology. 2020;95(16):e2200-e2213.
doi pubmed pmc - Mays VM, Cochran SD, Barnes NW. Race, race-based discrimination, and health outcomes among African Americans. Annu Rev Psychol. 2007;58:201-225.
doi pubmed pmc - Ananth CV, Keyes KM, Wapner RJ. Pre-eclampsia rates in the United States, 1980-2010: age-period-cohort analysis. BMJ. 2013;347:f6564.
doi pubmed pmc - Gestational hypertension and preeclampsia: ACOG Practice Bulletin, Number 222. Obstet Gynecol. 2020;135(6):e237-e260.
doi pubmed - Kittner SJ, Stern BJ, Feeser BR, Hebel R, Nagey DA, Buchholz DW, Earley CJ, et al. Pregnancy and the risk of stroke. N Engl J Med. 1996;335(11):768-774.
doi pubmed pmc - Bushnell C, Chireau M. Preeclampsia and stroke: risks during and after pregnancy. Stroke Res Treat. 2011;2011:858134.
doi pubmed pmc - Mrozek S, Lonjaret L, Jaffre A, Januel AC, Raposo N, Boetto S, Albucher JF, et al. Reversible cerebral vasoconstriction syndrome with intracranial hypertension: should decompressive craniectomy be considered? Case Rep Neurol. 2017;9(1):6-11.
doi pubmed pmc - StataCorp. Stata statistical software: release 18. College Station, TX: StataCorp LLC. 2023.
- Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-e110.
doi pubmed - Greenberg SM, Ziai WC, Cordonnier C, Dowlatshahi D, Francis B, Goldstein JN, Hemphill JC, 3rd, et al. 2022 guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022;53(7):e282-e361.
doi pubmed - Saver JL. Time is brain—quantified. Stroke. 2006;37(1):263-266.
doi pubmed - Guo QH, Liu CH, Wang JG. Blood pressure goals in acute stroke. Am J Hypertens. 2022;35(6):483-499.
doi pubmed pmc - ACR-SPR practice parameter for imaging pregnant or potentially pregnant patients with ionizing radiation. https://www.acr.org/-/media/ACR/Files/Practice-Parameters/Pregnant-Pts.pdf.
- Jain C. ACOG Committee Opinion No. 723: guidelines for diagnostic imaging during pregnancy and lactation. Obstet Gynecol. 2019;133(1):186.
doi pubmed - Younes N, Delaunay AL, Roger M, Serra P, Hirot F, Urbain F, Godart N, et al. Evaluating the effectiveness of a single-day simulation-based program in psychiatry for medical students: a controlled study. BMC Med Educ. 2021;21(1):348.
doi pubmed pmc - Sandeva MG, Tufkova S, Ketev K, Paskaleva D. Evaluating the effectiveness of simulation training in obstetrics and gynecology, pediatrics and emergency medicine. Folia Med (Plovdiv). 2019;61(4):605-611.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
