| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Original Article
Volume 13, Number 3, December 2024, pages 75-82
Racial and Gender Disparities in Obstetrics and Gynecology Applicants and Professionals
Rosa M. Polana, Dovid Y. Rosenb, c, Logan S. Coreya, Radhika P. Gogoia
aKarmanos Cancer Institute, Wayne State University, Detroit, MI, USA
bWayne State University School of Medicine, Detroit, MI, USA
cCorresponding Author: Dovid Y. Rosen, Wayne State University School of Medicine, Detroit, MI, USA
Manuscript submitted September 4, 2024, accepted November 2, 2024, published online December 2, 2024
Short title: Ob/Gyn by Race and Gender
doi: https://doi.org/10.14740/jcgo997
| Abstract | ▴Top |
Background: Equity is a driving force in healthcare, with the goal of creating a diversified workforce, particularly for medically underserved populations. The aim of this study was to measure demographic shifts in the Obstetrics and Gynecology (Ob/Gyn) trainee and physician workforce, including attrition and promotion rates.
Methods: This study included Ob/Gyn residency applicants, matriculants, and early-career faculty recorded by the Association of American Colleges (AAMC) from 2005 to 2020. Gender, race, publications, faculty promotion/attrition rates were analyzed. The χ2 test and two-sample t-test were used as appropriate. A P value < 0.05 was considered statistically significant, and Prism 9.0 (GraphPad Software Inc., CA, US) was used for analyses.
Results: By 2020, Ob/Gyn residency applicants were 20% male and 80% female, compared to 35% and 65% in 2005 (P < 0.001). By 2021, 66% of attendings, and 85% of residents were female, with an increase in White females of 8%, Black females 3%, and no increase in Hispanic and Asian females. Males declined across all races. White female faculty increased by 8%, while minority female faculty rose by 1-2%. Male faculty representation fell by 15%. Promotion rates were higher for White females (44%) than Black females (28%), with Black and Asian females leaving academia early than White and Hispanic females (44% vs. 38%). Male applicants published more than females (3.41 vs. 2.75, P < 0.001) but comprised only 20% of 2020 applicants. Asian males had the highest average publications (P = 0.001).
Conclusions: Over the last 20 years, Ob/Gyn applicants and faculty have seen large increases in White female faculty with minimal to no increase in minority and male representation. Understanding the reasons for this disparity will help promote more diverse representation in the field of Ob/Gyn.
Keywords: Ob/Gyn providers; Gender; Disparity
| Introduction | ▴Top |
Racial and gender equity is an important priority in medicine and healthcare. A diverse workforce is thought to deliver healthcare more effectively, particularly for medically underserved populations [1, 2]. Obstetrics and Gynecology (Ob/Gyn) is relatively more racially diverse than other medical specialties, with 11% of practicing physicians self-identifying as Black and 7% as Hispanic [3, 4]. However, when we consider gender, we find that in 1975, only 16% of Ob/Gyn residents were women, and by 1986, 51% of residents were women. By 2021, these proportions became more unbalanced, with women making up nearly two-thirds of practicing Ob/Gyns and 85% of Ob/Gyn trainees [5].
While the large number of female applicants ensures more same-sex providers for patients, which is an important factor for some patients when choosing a physician, the racial diversity of the workforce remains poorly stratified. Additionally, women and racial minorities are underrepresented in Chairperson and department leadership positions in Ob/Gyn [6]. This remains the case despite a contemporary focus on persistent inequality in academic medicine [7].
Though gender and racial disparities at the top of the academic hierarchy have been well described, there is a knowledge gap regarding disparities that affect the bulk of the workforce. We aim to characterize the racial and gender balance of contemporary Ob/Gyn residency program applicants and early-career faculty. We further aim to describe promotion rates for early-career academic faculty, stratified by race and gender.
| Materials and Methods | ▴Top |
This cross-sectional study included all Ob/Gyn residency program applicants, matriculated residents, and early-career faculty recorded by the American Association of Medical Colleges (AAMC) between 2001 and 2020. Data about faculty came from the AAMC’s Annual Faculty Roster. This national database contains demographic and employment records for more than 95% of full-time faculty at accredited US medical schools.
Full-time faculty members whose first assistant or associate professor appointment began between January 1, 2000, and December 31, 2010, were tracked for 10 years to determine promotion outcomes. Promotion rates of Doctor of Medicine (MD), Doctor of Medicine and Doctor of Philosophy (MD-PhD), and Doctor of Osteopathic Medicine (DO) faculty at the ranks of Instructor, Assistant Professor, Associate Professor and Full Professor only were recorded. Information about voluntary and part-time faculty, as well as faculty with a PhD alone, was excluded.
Data about gender and race were pulled from three national sources: the AAMC Student Records System [8], the AAMC Minority Physicians Database [9], and the American Medical Association Physician Masterfile [10]. Data from these sources were merged to form a cohesive analytic data set. A medical student’s self-reported primary racial background was classified as White, Black, Hispanic or Asian (inclusive of persons who identify as Native American, Alaska Native or Pacific Islander). These categories were treated as mutually exclusive for the purposes of this analysis. Those who did not report their racial background in any category, marked multiple racial categories or marked “other” were excluded. The self-reported primary racial background of Ob/Gyn residents and academic faculty were categorized according to the same classifications.
Average number of abstracts, presentations, and publications per Electronic Residency Application Service (ERAS) applicant to Ob/Gyn residency programs were calculated and stratified by gender and race. The Institutional Review Board considered this project to be exempt, because of the deidentified nature of this national dataset. The ethical compliance requirements related to human subjects are not applicable to this particular study. Descriptive statistics and bivariable tests were used to examine associations; χ2 test and two-sample t-test were used as appropriate. A P value < 0.05 was considered statistically significant, and Prism 9.0 (GraphPad Software Inc., CA, US) was used for all analyses.
| Results | ▴Top |
In 2005, 35% of Ob/Gyn residency applicants were male, and 65% were female. By 2020, the gender balance of applicants had become significantly more polarized, with 20% male and 80% female applicants (P < 0.001) (Fig. 1). Attrition rates for male and female residents during this time period were 1.1% and 0.5%, respectively.
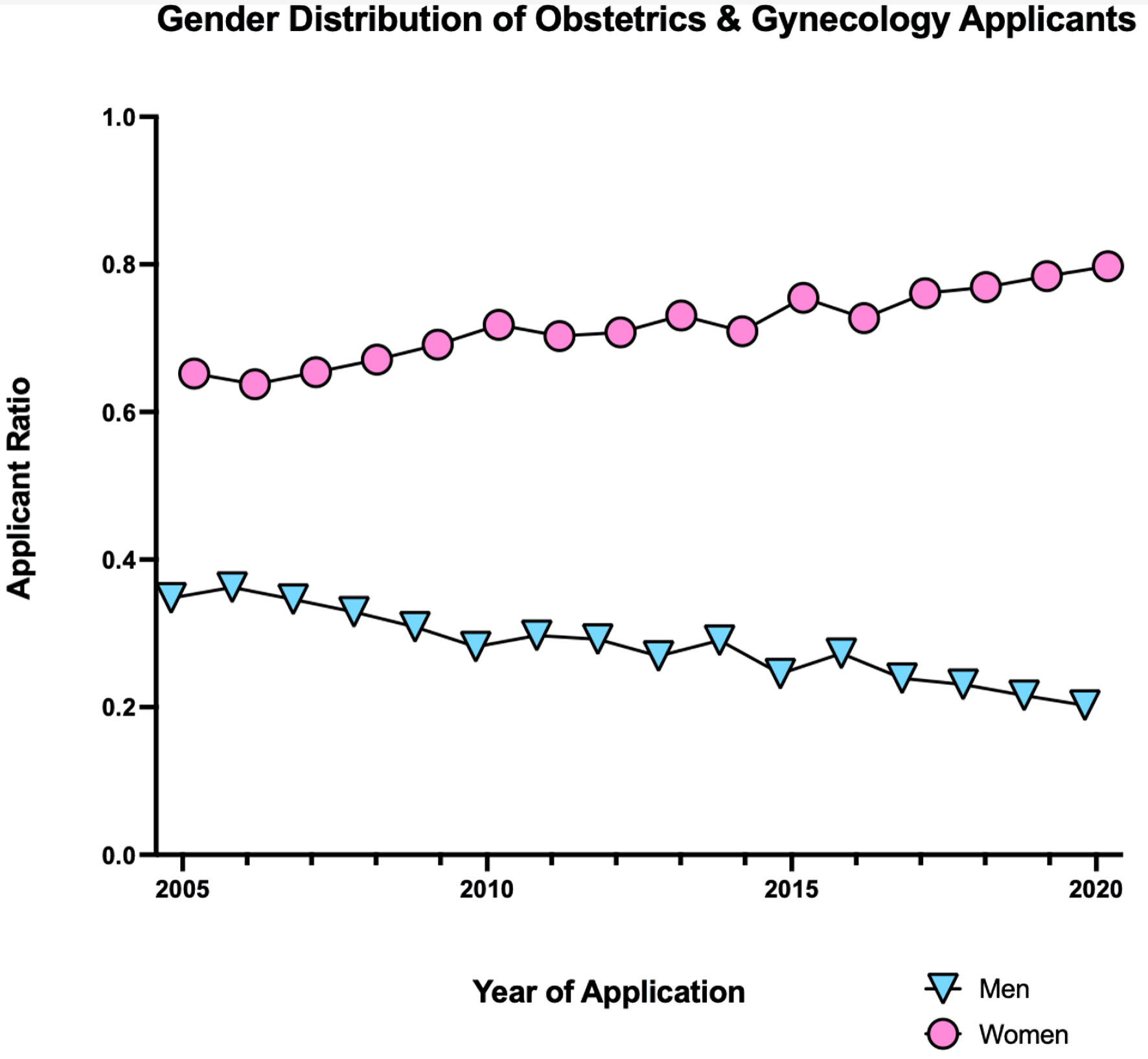 Click for large image | Figure 1. The yearly proportion of self-identified men and women applicants to Obstetrics And Gynecology residency from 2005 to 2020. |
With respect to applicant race and gender, notable change was noted in the proportion of White men applying to Ob/Gyn residency programs, decreasing from 17% to 11% between 2005 and 2020. By contrast, the proportion of White women applying for these residency positions increased from 39% to 47% (Fig. 2). The proportion of Asian women did not significantly change between 2005 and 2020 and comprised 17% of the total pool. The proportion of Asian men decreased from 7% to 3% between 2005 and 2020. The proportion of Black women applicants increased from 8% to 11%, and the proportion of Black men applicants decreased from 4% to 2% between 2005 and 2020. The proportion of Hispanic women remained stable at 6%, while the proportion of Hispanic men decreased from 4% to 2% (Table 1).
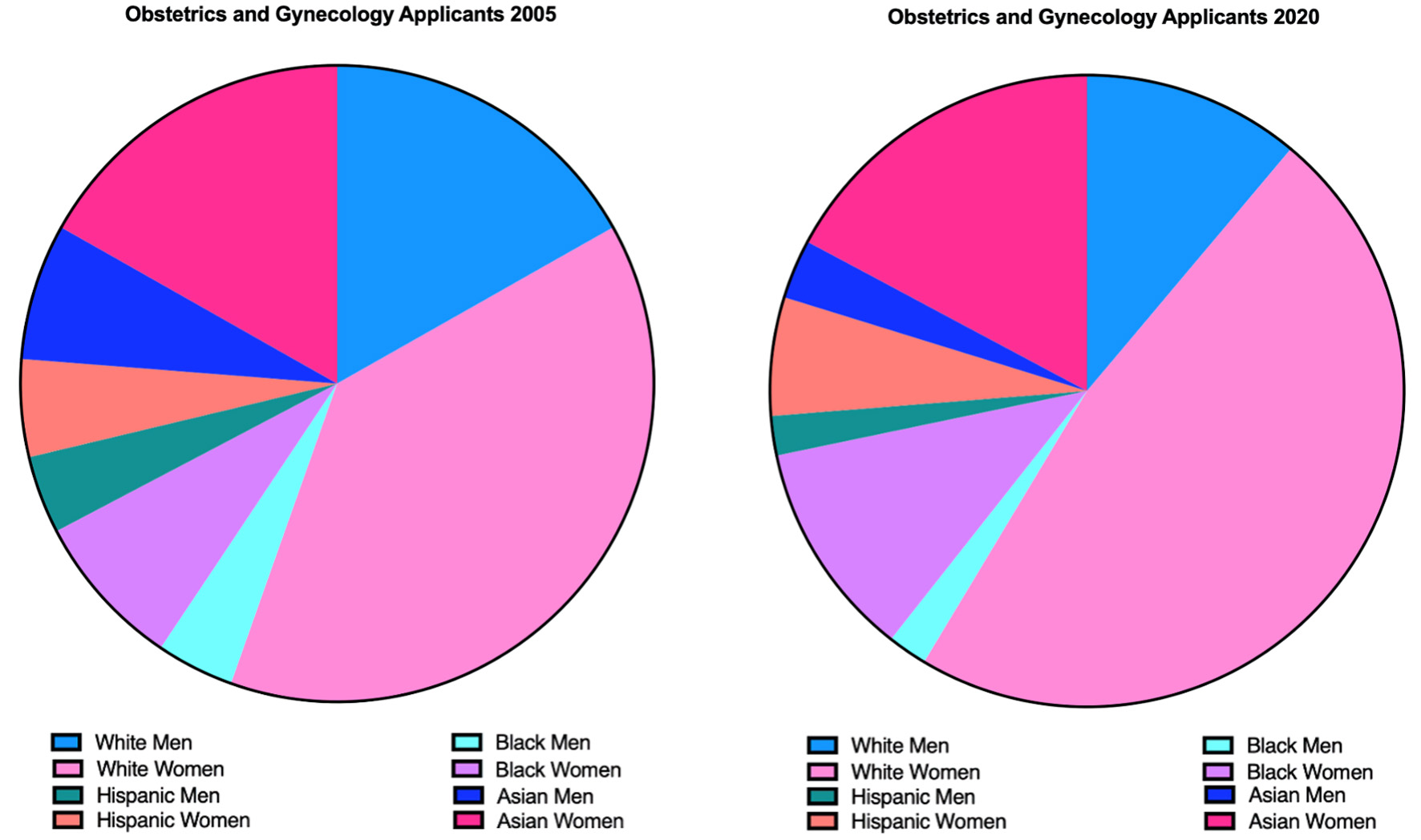 Click for large image | Figure 2. The proportion of Obstetrics and Gynecology residency applicants by self-reported gender, race, and ethnicity in 2005 and 2020. |
 Click to view | Table 1. Residency Applicant Rates by Self-Reported Gender and Race (2005 to 2020) |
The median number of publications per residency applicant increased for both genders between 2005 and 2020 and were significantly different by race and gender. Male applicants reported an average of 3.41 publications (compared to 2.4 in 2005) versus 2.75 reported by female applicants (1.5 in 2005) (P < 0.001) (Fig. 3). Applicants who were identified as Asian men had significantly more publications (6.6 in 2020, up from 3.2 in 2005) than men and women of all other races (range of significance from P = 0.049 to P = 0.001) (Fig. 4).
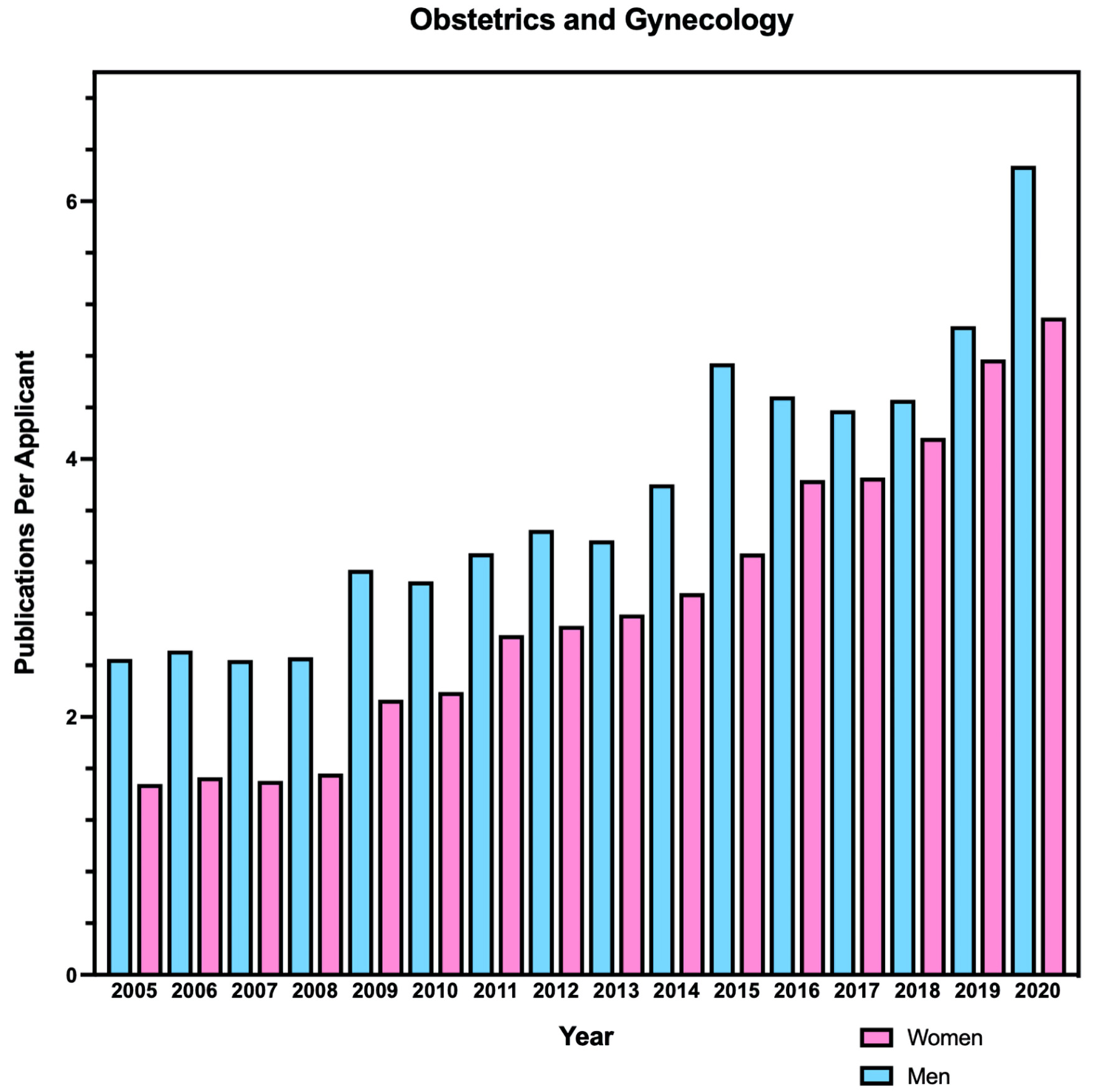 Click for large image | Figure 3. The average number of abstracts, publications, and presentations per Obstetrics and Gynecology residency program applicant between 2005 and 2020. |
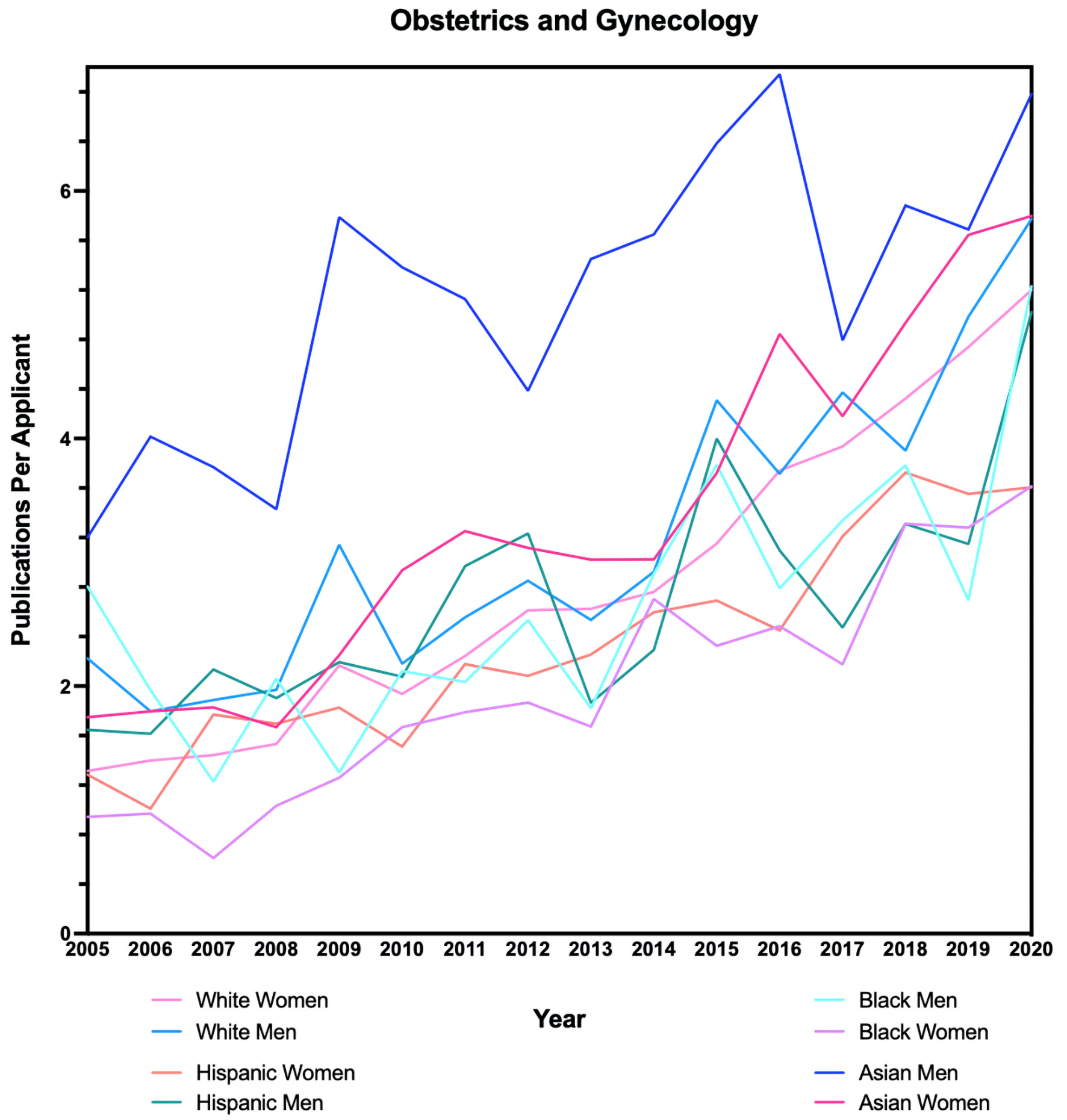 Click for large image | Figure 4. Average abstracts, publications, and presentations per Obstetrics and Gynecology residency program applicant by gender, race, and ethnicity between 2005 and 2020. |
We next examined the gender and racial balance of Ob/Gyn academic faculty, including individuals at the rank of Instructor, Assistant Professor, Associate Professor, and Full Professor (Fig. 5). The proportion of Asian women in these faculty appointments increased from 8% to 10% between 2010 and 2020. The proportion of Asian men decreased from 5% to 4% over this period. The proportion of Black women increased from 5% to 7% between 2010 and 2020, and the proportion of Black men decreased from 3% to 2%. The proportion of Hispanic women academic faculty in Ob/Gyn increased from 2% to 3% while the proportion of Hispanic men proportionally decreased from 3% to 2%. The largest absolute changes were noted in the proportions of White men and women; the proportion of White men decreased from 35% to 23% between 2010 and 2020, while the proportion of White women increased from 35% to 43%.
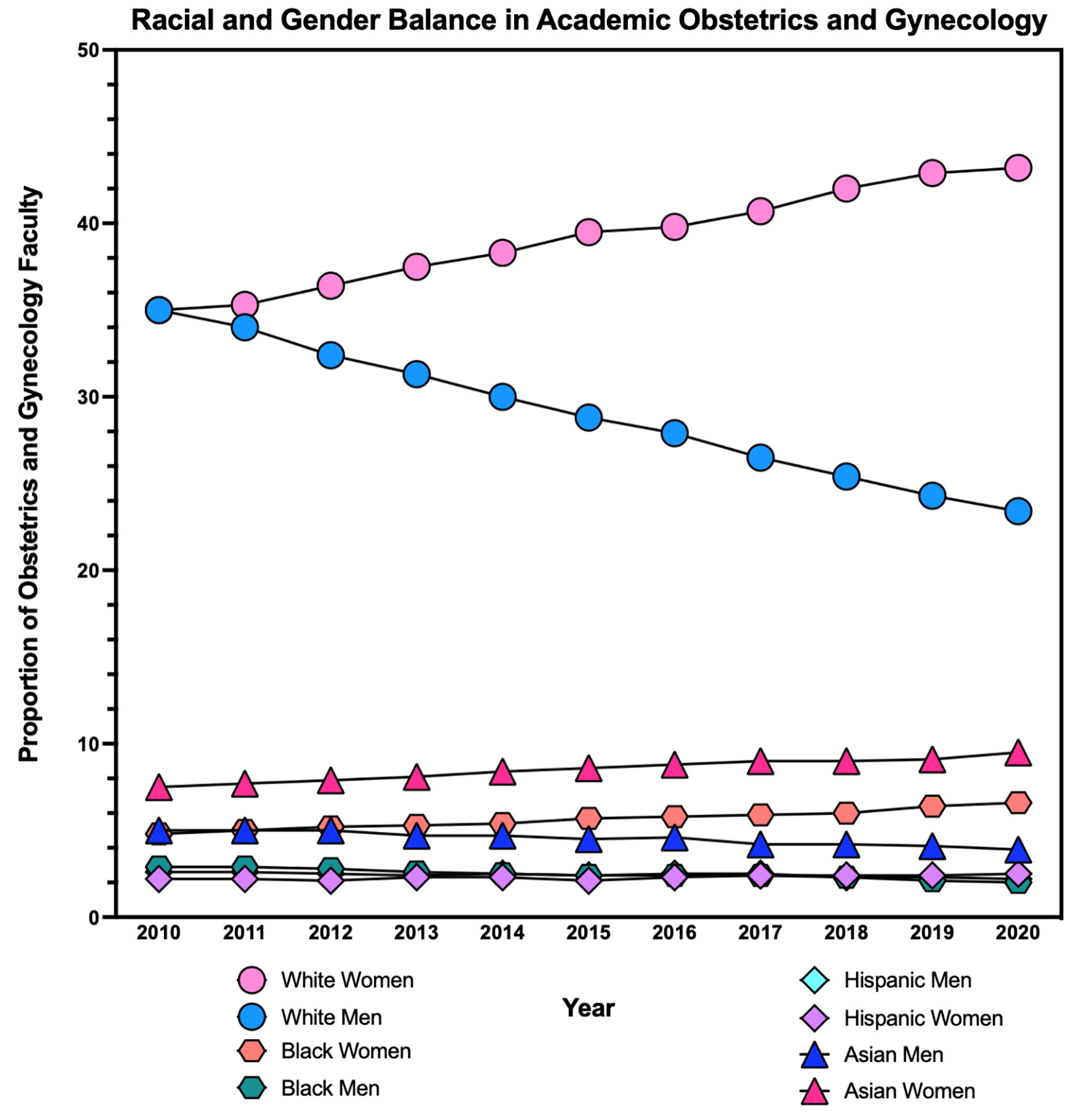 Click for large image | Figure 5. The yearly proportion of Obstetrics and Gynecology faculty by self-reported gender, race, and ethnicity from 2005 to 2020. The bottom three trends include Black men, Hispanic men, and Hispanic women. |
Promotion rates for early-career Ob/Gyn academic faculty differed by race and gender (Table 2). All full-time faculty appointed between January 1, 2000, and December 31, 2010, were followed for 10 years (a cohort of 1,916 men and 2,564 women). One-third of White and Asian men (34% for both) were promoted within 10 years of hire, compared with 23% (n = 30) of Black men and 27% (n = 27) of Hispanic men. Overall, 32% of early-career male faculty were promoted within 10 years of hire. Promotion rates for women were different by race, with 35% (n = 568) of White and 33% (n = 124) of Asian women promoted within 10 years, compared with 21% (n = 48) of Black and 25% (n = 28) of Hispanic women. Overall, 31% of early-career women faculty were promoted within 10 years of hire.
 Click to view | Table 2. Academic Faculty Promotion Rates by Self-Reported Gender and Race (2000 to 2010) |
| Discussion | ▴Top |
Our study found that the demographics of academic Ob/Gyn have shifted over the past two decades, with more women entering residency programs, as well as being promoted in academic medicine. This represents a tremendous change from what was, as recently as 30 years ago, a male-dominated specialty [6].
A notable change was noted in the proportion of White men applying to Ob/Gyn residency programs, decreasing by 6% between 2005 and 2020. In contrast, the proportion of White women applying for these residency positions increased by 8% over this period. While the increase in female applicants is noteworthy, there is a noticeable lack of racial diversity of this applicant pool. The proportion of Asian men decreased by 4%, yet the proportion of Asian women did not significantly change between 2005 and 2020. The proportion of Black male applicants decreased by 2%, while Black women applicants only increased by 3%, compared to 8% increase in White women. Lastly, the proportion of Hispanic men decreased by 2%, but the proportion of Hispanic women applying to Ob/Gyn remained unchanged.
This shift in demographics has led to decreased diversity in the field of Ob/Gyn. Also noted was the imbalance of career growth of practicing providers. This increase in female providers was not reflected at the top of the academic hierarchy.
Our findings suggest that the most substantial gains in academic Ob/Gyn have been limited to White women. Like the data regarding residency applicants, male academic faculty saw a decline across all races. The proportion of White female faculty increased substantially (35% to 43%) while Black, Asian, and Hispanic female faculty increased by just 1-2% over the past two decades. Additionally, a disparity in promotion rates by race was observed, with White men and women promoted at higher rates than faculty of all other races.
Additionally, we found a disparity when comparing the eligibility for full professorship across races and genders. There was a promotion rate of 44% for eligible White and Asian women, with Black women having just a 28% promotion rate. Moreover, Black and Asian women left academic medicine within 5 years of initial faculty appointment at higher rates than White and Hispanic women (44% versus 38%). These discrepancies persist despite the field of Ob/Gyn employing a significantly greater proportion of underrepresented minority physicians compared with other academic medical specialties [3].
Commentary on the gender imbalance in Ob/Gyn is not new. In 2003, a former Obstetrics and Gynecology Journal editor, expressed concern that having a specialty dominated by one gender could alter the quality of applicants pursuing Ob/Gyn [11, 12]. Our study, nearly 20 years later, qualitatively reaffirms this worry and found that the male applicants had objectively higher rates of publications than their female counterparts every year between 2005 and 2020 (a common metric used to measure applicant quality). Yet, males made up only 20% of applicants in 2020, and Asian males significantly outperformed all races and genders in the average number of publications but made up a progressively lower proportion of applicants year after year.
In 2005, the American College of Obstetrics and Gynecology (ACOG) Medical Student Recruitment Task Force stated, “in our attempt to attract women to the field in the 1980s and 1990s, we had inadvertently sent the message to male medical students that there no longer was a place for them in obstetrics and gynecology” [13]. Our study confirms this trend is pervasive and ongoing. Despite concern regarding gender homogeneity, the gender gap has continued to broaden over the last 20 years. The disparate clerkship experiences between the male and female medical students have been well described and have been proposed as a reason for failing to encourage men to apply [14]. Unfortunately, any changes encouraged by ACOG and others have failed to materialize as Ob/Gyn is one of the only specialties that is becoming more homogenous and less diverse over the last 20 years [14].
Our study did identify several areas of growth to be celebrated: the proportion of Ob/Gyn applicants who identified as Black women has increased over the past two decades. Additionally, the proportion of female academic faculty mirrors the gender balance of the overall Ob/Gyn workforce, and the promotion rates for male and female faculty are comparable.
However, this study highlights two areas in need of significant improvement: the recruitment of male and minority medical students; and the retainment and promotion of female faculty in academic medicine, especially underrepresented minorities.
Our study used self-reported demographic data, the gold standard for racial and gender variables [15]. Additionally, this dataset includes a large, continuous, and well-maintained database of all medical school applicants who apply through the National Ranking Resident Matching Program and all appointed faculty of medical schools that are members of the AAMC. Lastly, the number of applicants who did not self-report their gender or race was low (15% or less across all categories), allowing for increased confidence that the proportions of gender and race are accurate.
This study has several important limitations. The promotion rates are not reported each year but instead are grouped into 5- and 10-year periods by the AAMC. This does not allow for a more granular examination of the data. The publication number reported by medical school applicants is not verified and makes no distinction between first authorships, poster presentations, oral presentations, etc. Academic productivity is difficult to quantify and a first-author, peer-reviewed publication is generally held in higher regard than a fifth-author abstract. Lastly, reasons for promotion are not included in the data. Microaggressions, bullying, and socioeconomic stressors of underrepresented minorities are common reasons for leaving academic medicine that we could not assess in this study [16].
Understanding the reasons for these racial and gender disparities will further our efforts to ensure our field has racial and gender equity throughout its ranks to provide excellent healthcare delivery to patients of all backgrounds. Efforts should be made to further evaluate the root causes of these demographic changes.
Conclusions
Ob/Gyn as a field has made progressive strides towards achieving greater gender equity. Yet, despite a recent focus on equity for underrepresented minority physicians in our field, we did not find gains in Black, Hispanic, and Asian women in residency applications or academia comparable to the observed increase in the proportion of White women. Additionally, these strides may have had the unintended result of pushing men away from the specialty.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare no potential conflict of interest.
Informed Consent
Informed consent was deemed exempt for this study.
Author Contributions
Rosa M. Polan: Introduction, Methods, Results, and Discussion. Dovid Y. Rosen: Abstract, Introduction, Discussion, Conclusions, and manuscript structure and editing. Logan S. Corey: Methods and Results. Radhika P. Gogoi: Methods, Results, and manuscript structure and editing.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
Ob/Gyn: obstetrics and gynecolgy; AAMC- Association of American Colleges: ; ERAS: Electronic Residency Application Service; ACOG: American College of Obstetrics and Gynecology
| References | ▴Top |
- Diversity, equity & inclusive excellence at ACOG. n.d. Accessed March 17, 2022. https://www.acog.org/about/diversity-equity-and-inclusive-excellence.
- Rosen D. Questioning the premedical paradigm: enhancing diversity in the medical profession a century after the flexner report. JAMA: The Journal of the American Medical Association. 2011;306(9):1001.
- Rayburn WF, Xierali IM, Castillo-Page L, Nivet MA. Racial and ethnic differences between obstetrician-gynecologists and other adult medical specialists. Obstet Gynecol. 2016;127(1):148-152.
doi pubmed - Lopez CL, Wilson MD, Hou MY, Chen MJ. Racial and Ethnic Diversity Among Obstetrics and Gynecology, Surgical, and Nonsurgical Residents in the US From 2014 to 2019. JAMA Netw Open. 2021;4(5):e219219.
doi pubmed - Table B3: number of active residents, by type of medical school, GME Specialty, and Sex. n.d. AAMC. Accessed March 1, 2022. https://www.aamc.org/data-reports/students-residents/interactive-data/table-b3-number-active-residents-type-medical-school-gme-specialty-and-sex.
- Seltzer VL. Changes and challenges for women in academic obstetrics and gynecology. Am J Obstet Gynecol. 1999;180(4):837-848.
doi pubmed - Roberts LW. Women and academic medicine. academic medicine. Journal of the Association of American Medical Colleges. 2020;95(10):1459-1464.
- www.aamc.org/data-reports/students-residents/report/student-records-system-srs.
- www.aamc.org/data-reports/workforce/report/physician-specialty-data-report.
- www.mmslists.com/ama-research.
- Queenan JT. ACOG names new deputy editor for obstetric & gynecology. Obstetrics & Gynecology. 2001;98(2):357.
- Queenan JT. The future of obstetrics and gynecology. Obstet Gynecol. 2003;102(3):441-442.
doi pubmed - Bienstock JL, Laube DW. The recruitment phoenix: strategies for attracting medical students into obstetrics and gynecology. Obstet Gynecol. 2005;105(5 Pt 1):1125-1127.
doi pubmed - Craig LB, Buery-Joyner SD, Bliss S, Everett EN, Forstein DA, Graziano SC, Hampton BS, et al. To the point: gender differences in the obstetrics and gynecology clerkship. Am J Obstet Gynecol. 2018;219(5):430-435.
doi pubmed - HHS implementation guidance on data collection standards for race, ethnicity sex, primary language, and disability status. n.d. ASPE. Accessed July 25, 2022. https://aspe.hhs.gov/reports/hhs-implementation-guidance-data-collection-standards-race-ethnicity-sex-primary-language-disability-0.
- Nguyen BT, Mitchell-Chadwick N, Heyrana KJ. Declines in the proportion of US black obstetrics and gynecology residents. JAMA Netw Open. 2021;4(5):e219710.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
