| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 6, Number 3-4, October 2017, pages 71-74
Distant Cutaneous Manifestations of a Primary Gynecologic Malignancy
Alexis D. Lighta, Erin E. Higginsa, c, Faye F. Gaob, Stephanie L. Wethingtona
aDepartment of Obstetrics and Gynecology, MedStar Washington Hospital Center, 110 Irving St NW, Washington, DC 20010, USA
bDepartment of Pathology and Laboratory Medicine, MedStar Washington Hospital Center, 110 Irving St NW, Washington, DC 20010, USA
cCorresponding Author: Erin Higgins, Department of Obstetrics and Gynecology, MedStar Washington Hospital Center, 110 Irving St NW, Suite 5B-63, Washington, DC 20010, USA
Manuscript submitted August 23, 2017, accepted October 3, 2017
Short title: Distant Cutaneous Malignancy
doi: https://doi.org/10.14740/jcgo461w
| Abstract | ▴Top |
Uterine cancer is the most common gynecologic cancer in the United States. While most cases are diagnosed early and recurrence is rare with adequate treatment, late stage disease has a much worse prognosis, with 5-year survival rates of 25-45%. We report the presentation of recurrent uterine serous carcinoma with metastasis to the skin. An 80-year-old postmenopausal female with a history of endometrial intraepithelial carcinoma was diagnosed with recurrent metastatic disease 3 years after her initial presentation. During hospital admission, she was noted to have clusters of rubbery cutaneous nodules with an erythematous vesicular appearance on the left breast. Biopsy of the lesions showed metastatic serous adenocarcinoma consistent with gynecologic origin. Cutaneous metastasis is a rare finding in uterine cancer. This case highlights the importance of maintaining a wide differential diagnosis and high level of suspicion when evaluating skin lesions in the setting of uterine pathology.
Keywords: Uterine cancer; Serous adenocarcinoma; Endometrial intraepithelial carcinoma; Skin metastasis
| Introduction | ▴Top |
Uterine cancer is the most common gynecologic malignancy in the developed world. It often presents with abnormal uterine bleeding and is typically diagnosed early. It is thought to be highly curable with an overall 5-year survival of 80% [1]. Recurrence of this cancer is rare and usually occurs locally in the pelvis [2]. Cutaneous metastasis is an infrequent finding of uterine cancer, with fewer than 15 cases in the literature [3]. While rare, it is important for providers to recognize the unique presentations of distant metastasis of this gynecologic cancer. We report the case of a woman diagnosed with recurrent uterine serous adenocarcinoma who was found to have cutaneous lesions that were found to represent metastatic disease.
| Case Report | ▴Top |
An 80-year-old multigravid postmenopausal female presented to the office with right-sided abdominal pain and vaginal bleeding. Initial evaluation included an endometrial biopsy. The pathology results were consistent with simple to complex atypical hyperplasia of the endometrium, suspicious for adenocarcinoma. She subsequently underwent robotic-assisted total laparoscopic hysterectomy with right salpingo-oophorectomy (the left adnexa was surgically absent). Pathologic findings revealed a 3 mm focus of endometrial intraepithelial carcinoma (EIC) (Fig. 1). She underwent no adjuvant therapy at that time.
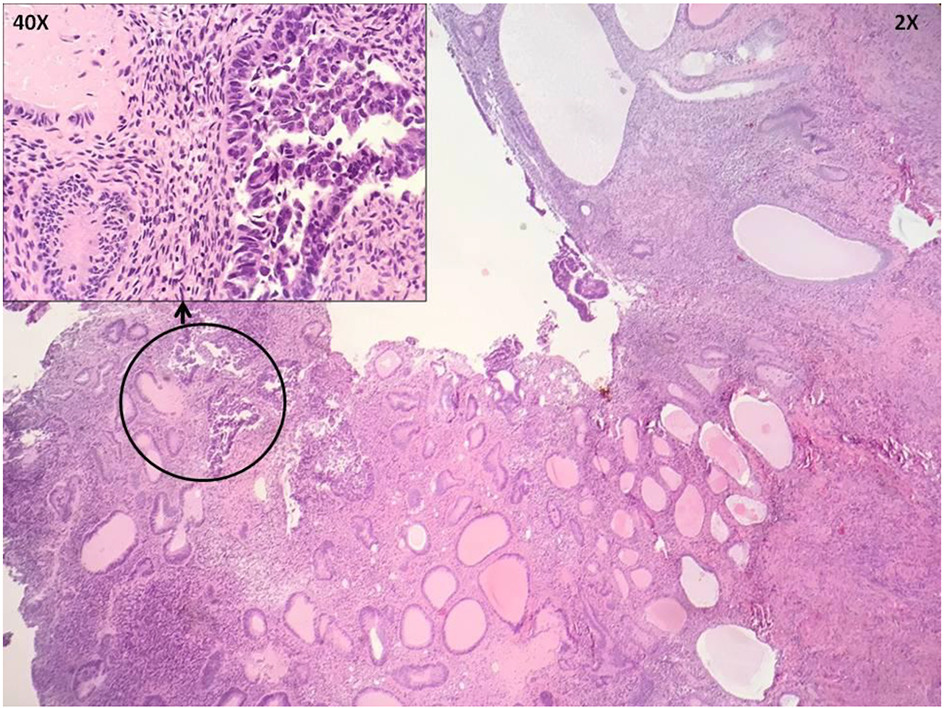 Click for large image | Figure 1. Hysterectomy specimen shows endometrial intraepithelial carcinoma (EIC) in an endometrial polyp. |
Three years later, during routine surveillance, the patient was diagnosed with a recurrence in a left axillary lymph node (PAX8, ER, and PR positive). She was treated with systemic chemotherapy, initially with carboplatin and paclitaxel (four cycles), and then with carboplatin and docetaxel (two cycles) due to peripheral neuropathy. There was no evidence of disease on a computerized tomography (CT) scan at the end of treatment and the CA-125 level normalized. Within 6 months of completing treatment, however, the CA-125 level increased and a CT scan demonstrated recurrence of disease. The patient was then treated with six cycles of single-agent docetaxel. There was poor clinical response to docetaxel, and treatment with temsirolimus was then initiated.
Shortly after receiving the first cycle of temsirolimus, the patient’s performance status rapidly declined, requiring hospitalization. Physical examination on admission was remarkable for clusters of rubbery cutaneous nodules with an erythematous vesicular appearance on the left breast (Fig. 2a). The patient reported that the skin findings had only recently appeared, and, while pruritic at first, were no longer bothersome. She denied having lesions elsewhere, but on further examination, similar nodules were noted on the left vulva (Fig. 2b). A biopsy of the left breast lesion was done, and pathology showed metastatic carcinoma with pleomorphic high-grade nuclei beneath the epidermis (Fig. 3). The epidermis showed hyperkeratosis with no evidence of dysplasia. Immunostains performed on the biopsy demonstrated that the tumor cells were positive for CK7, PAX8, and p53 (diffuse and strong) and negative for CK20, CDX-2, TTF-1, GATA3, ER, and PR. These findings were consistent with a serous carcinoma of gynecologic origin.
 Click for large image | Figure 2. (a) Lesions on patient’s left breast. Distribution suggestive of herpes zoster. (b) Vulva and mons pubis, with a single lesion visible on posterior left vulva. |
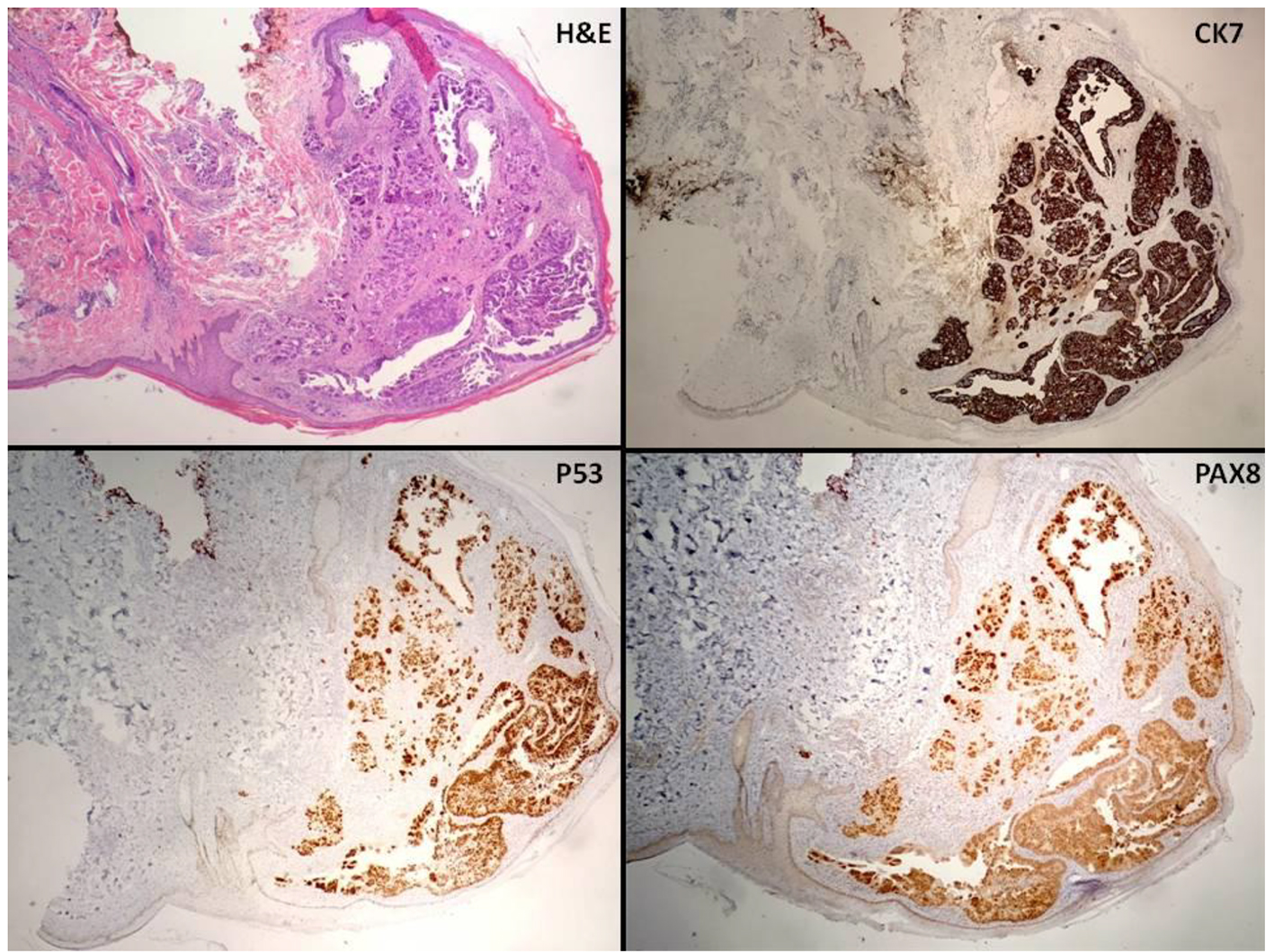 Click for large image | Figure 3. Low power view of cutaneous punch biopsy (× 4) with immunostains. |
During this admission, the patient was found to have bilateral pleural effusions and underwent thoracentesis. She was re-admitted to the hospital 1 month later with a large bowel obstruction due to widespread metastatic disease and an exploratory laparotomy with loop colostomy was performed. She was subsequently discharged to subacute rehabilitation. Her clinical status continued to decline, and she passed away 3 months after these cutaneous lesions were identified. A summary of the patient’s clinical course is shown in Table 1.
 Click to view | Table 1. Summary of Patient’s Clinical Course |
| Discussion | ▴Top |
In this report, we present the case of a woman with recurrent uterine serous carcinoma found to have cutaneous metastases. Distant cutaneous metastasis of cancer is rare, and those from gynecologic cancers are even less frequently documented in the literature [4, 5]. When seen in gynecologic oncology patients, they are most commonly described from primary ovarian malignancies with occurrence locally in the pelvis or umbilical region (e.g. Sister Mary Joseph nodule) and typically present as erosions through the skin [6-8].
This patient’s lesions were of particular interest due to the differential diagnosis that was evoked. With the erythematous vesicular appearance and dermatomal distribution on the torso, the nodules were initially suggestive of herpes zoster [9]. Additionally, the location of the lesions on the left breast was concerning for a possible primary breast cancer, as cutaneous metastasis of breast cancer is more commonly seen [10]. The differential also included contact dermatitis and an autoimmune process. The diagnosis of metastatic serous carcinoma was eventually confirmed based on punch biopsy of the breast nodule. This serves to enforce the importance of biopsy when evaluating dermatologic lesions in a patient with a history of uterine pathology.
While similar cases have been presented in the literature, there remain few reports of cutaneous metastasis from a primary uterine cancer. As Chang et al reported, skin lesions can rarely be the presenting symptom of uterine malignancy, but are more likely to occur in the setting of known disease [3]. This case highlights the diverse way in which recurrent uterine cancer can manifest. It is important for clinicians to consider metastasis when a patient presents with skin changes with a history of uterine cancer.
Conflict of Interest
The authors report no conflict of interest.
Financial Support
There was no financial support of this research.
Consent
Written informed consent for this report was obtained from the patient for publication of this case report and accompanying imaging. MedStar Washington Hospital Center’s institutional review board approved this case report.
| References | ▴Top |
- Amant F, Moerman P, Neven P, Timmerman D, Van Limbergen E, Vergote I. Endometrial cancer. Lancet. 2005;366(9484):491-505.
doi - Greven KM, Lanciano RM, Corn B, Case D, Randall ME. Pathologic stage III endometrial carcinoma. Prognostic factors and patterns of recurrence. Cancer. 1993;71(11):3697-3702.
doi - Chang ES, Baker WD, Landen CN. Metastatic papillary serous uterine cancer presenting as a rash. Gynecol Oncol Rep. 2016;18:11-13.
doi pubmed - Lookingbill DP, Spangler N, Helm KF. Cutaneous metastases in patients with metastatic carcinoma: a retrospective study of 4020 patients. J Am Acad Dermatol. 1993;29(2 Pt 1):228-236.
doi - Lookingbill DP, Spangler N, Sexton FM. Skin involvement as the presenting sign of internal carcinoma. A retrospective study of 7316 cancer patients. J Am Acad Dermatol. 1990;22(1):19-26.
doi - Cormio G, Capotorto M, Di Vagno G, Cazzolla A, Carriero C, Selvaggi L. Skin metastases in ovarian carcinoma: a report of nine cases and a review of the literature. Gynecol Oncol. 2003;90(3):682-685.
doi - Atallah D, el Kassis N, Lutfallah F, Safi J, Salameh C, Nadiri S, Bejjani L. Cutaneous metastasis in endometrial cancer: once in a blue moon - case report. World J Surg Oncol. 2014;12:86.
doi pubmed - Kara A, Belli AA, Alatas ET, Tanriverdi O, Dere Y. Widespread cutaneous metastasis from ovarian serous adenocarcinoma. Dermatol Online J. 2016;22(7).
pubmed - Schonmann R, Altaras M, Biron T, Bernheim J, Fishman A. Inflammatory skin metastases from ovarian carcinoma - a case report and review of the literature. Gynecol Oncol. 2003;90(3):670-672.
doi - Kazakov DV, Suster S, LeBoit PE, Calonje E, Bisceglia M, Kutzner H, Rutten A, et al. Mucinous carcinoma of the skin, primary, and secondary: a clinicopathologic study of 63 cases with emphasis on the morphologic spectrum of primary cutaneous forms: homologies with mucinous lesions in the breast. Am J Surg Pathol. 2005;29(6):764-782.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
